Abstract
Diabetes mellitus (DM) and thyroid dysfunction (TD) often tend to coexist in patients. Both hypothyroidism and hyperthyroidism are more common in type 2 diabetes mellitus (T2DM) patients than in their nondiabetic counterparts. Current guidelines are neither clear nor specific about the frequency of thyroid function monitoring in T2DM patients. Circulating thyroid hormones affect several different organs and cells, have a major impact on glucose, lipid, and protein metabolism, and can worsen glycaemic control in T2DM. Hyperthyroidism and thyrotoxicosis can worsen subclinical DM and cause hyperglycaemia in T2DM patients, increasing the risk of diabetic complications. T2DM reduces thyroid-stimulating hormone levels and impairs the conversion of thyroxine (T4) to triiodothyronine (T3) in the peripheral tissues. Poorly managed T2DM can lead to insulin resistance and hyperinsulinaemia, which causes thyroid tissue proliferation and increases nodule formation and goitre size. In addition, while metformin can be beneficial in both T2DM and TD patients, other antidiabetics such as sulfonylureas, pioglitazone, and thiazolidinediones can negatively impact TD. Antithyroid drugs such as methimazole can impair glycaemic control in T2DM patients. Thyrovigilance in T2DM patients and diabetovigilance in TD patients may therefore be necessary to facilitate individualized care and management.
Funding: Abbott India Ltd.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) and thyroid dysfunction (TD) are endocrinopathies that are commonly seen in routine practice, and they frequently coexist. A high prevalence of TD is seen among both type 1 (T1DM) and type 2 (T2DM) diabetes mellitus patients [1, 2]. Autoimmunity can explain the common linkage between T1DM and autoimmune thyroid diseases; however, the linkage between T2DM and TD is more complicated. This review summarizes current knowledge about coexistent T2DM and TD and discusses enhanced screening recommendations as well as clinical implications for the management of these two endocrinopathies. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Search Strategy
We used the following strategy to search PubMed database for relevant articles published over the past 10 years: (“thyroid dysfunction”[All Fields] AND (“hypothyroidism”[MeSH Terms] OR “hypothyroidism”[All Fields] OR “hypothyroid”[All Fields]) AND (“hyperthyroidism”[MeSH Terms] OR “hyperthyroidism”[All Fields] OR “hyperthyroid”[All Fields])) AND (“diabetes mellitus”[MeSH Terms] OR (“diabetes”[All Fields] AND “mellitus”[All Fields]) OR “diabetes mellitus”[All Fields] OR “diabetes”[All Fields] OR “diabetes insipidus”[MeSH Terms] OR (“diabetes”[All Fields] AND “insipidus”[All Fields]) OR “diabetes insipidus”[All Fields]) AND (“2009/02/14”[PDat]: “2019/02/11”[PDat]).
In addition, we searched the websites of major diabetes and endocrine practice professional organizations for recommended guidelines on thyroid screening in persons with T2DM and diabetes screening in TD.
Prevalence of Diabetes and Thyroid Dysfunction
Both T2DM and TD are chronic diseases that require lifelong treatment and have a long-lasting effect on cardiovascular health. According to the International Diabetes Federation (IDF), in the year 2017, approximately 425 million adults worldwide were living with diabetes [3]. The total prevalence of diabetes is increasing and is expected to be 629 million by 2045 [3].
As per a large European meta-analysis, TD is present in 3.82% of the general population [4]. Its prevalence among those with T2DM is significantly higher, ranging from 9.9 to 48% [5, 6]. This wide range of prevalence can be explained by the use of different definitions for TD diagnosis, depending on the presence of anti-thyroid peroxidase (anti-TPO), antithyroglobulin antibody (anti-TG), or both. In many studies, most T2DM patients with TD had subclinical hypothyroidism (SCH), and several new cases of TD were diagnosed during clinical evaluations, highlighting the need for enhanced screening for TD in T2DM patients [5, 7, 8]. Just as in the nondiabetic population, TD was found to be more common in females than in males with diabetes [8,9,10]. TD is more common in T1DM than in T2DM patients, but the pathophysiology is more complex in T2DM patients and has greater clinical implications.
Clinical Guidelines on Screening for Thyroid Disorders in Diabetes
It is important to screen for TD in T2DM patients as each of these endocrinopathies and their complex interdependent interactions increase cardiovascular risks. However, some guidelines do not mention anything about monitoring thyroid function in T2DM [11,12,13], while others recommend a thyroid function test at baseline but are against routine annual thyroid screening in T2DM [14] (Table 1).
In its guidance for 2000, the American Thyroid Association recommended that adults who were at least 35 years old should be screened for thyroid disorders by measuring serum thyrotropin every 5 years irrespective of whether they were diabetic or nondiabetic [17]. However, the 2015 Thyroid Dysfunction: Screening Guidelines of the US Preventive Services Task Force conclude that there is insufficient evidence to recommend TD screening in nonpregnant or asymptomatic adults [18].
The recommendations for thyroid function screening of T2DM patients are not clear. The increasing evidence supporting a link between T2DM and TD, however, suggests that screening may need to be considered [19].
Clinical Implications of Diabetes and Thyroid Disease Coexistence
Both insulin and thyroid hormone are affected by autoimmune pathology, are part of metabolic syndrome, and affect the cellular metabolism. The pathophysiological association between T2DM and TD is believed to be the result of interplay between various biochemical, genetic, and hormonal malfunctions [20]. Increased expression of the hepatic glucose transporter type 2 gene (GLUT2) is found in hyperthyroidism [20]. Intracellular triiodothyronine (T3) may also play a role in insulin sensitivity [21]. It mediates the action of the GLUT4 gene in skeletal muscles and increases basal and insulin-mediated glucose transport [20]. Homozygosity for the Thr92Ala polymorphism of the deiodinase type 2 (DIO2) gene also enhances the risk for T2DM [20].
T2DM and TD have similar signs and symptoms, such as oedema, fatigue, pallor, and weight gain. Thus, T2DM can mask TD and TD can mask early diabetic complications. Antidiabetic therapy may affect thyroid function, and antithyroid drugs can worsen glycaemic control. Hence, dose adjustments may be needed during clinical practice.
Thyroid Hormones and Glucose Homeostasis
Excess circulating thyroid hormones in hyperthyroidism is associated with poor glycaemic control, including hyperglycaemia and insulinopenia. When normal individuals develop hyperthyroidism, nearly 2–3% of them develop overt diabetes [21]. Nearly 50% of those with Graves’ disease have some degree of glucose intolerance [21]. Diabetic patients with hyperthyroidism experience worsened glycaemic control. Thyrotoxicosis can precipitate diabetic complications such as diabetic ketoacidosis [22] and endothelial dysfunction [23]. Endothelial dysfunction increases the risk of cardiovascular comorbidities.
Thyroid hormone can act on various organs to affect glucose metabolism (Table 2). It increases gastrointestinal motility and enhances glucose absorption [24]. In the liver, it increases the activity of phosphoenolpyruvate carboxykinase (PEPCK), an enzyme that enhances gluconeogenesis [24]. This hepatic gluconeogenesis may occur through the direct effect of the thyroid hormone or indirectly via glucagon or catecholamine [20, 24].
The enhanced glycogenolysis and increased hepatic glucose output induces hyperinsulinaemia and glucose intolerance, causing peripheral insulin resistance [20]. This worsens subclinical diabetes and exaggerates the hyperglycaemia in T2DM, increasing the risk of diabetic complications.
In the adipose tissues, thyroid hormone increases lipolysis. The increased serum free fatty acid level causes insulin resistance [24]. Elevated lipolysis and increased hepatic β-oxidation, complicated by an insulin-deficient state, can lead to ketoacidosis [20, 24].
Hyperthyroidism increases GLUT4 gene expression and glucose uptake in skeletal muscles [24]. Thyroid hormones also directly control insulin secretion by beta cells. Hypothyroidism reduces glucose-induced insulin secretion, whereas hyperthyroidism enhances the response of beta cells to glucose. Degradation of insulin is also increased by thyroid hormone, and thyrotoxicosis increases insulin clearance [20, 24]. Thyroid hormone also increases glucagon secretion by pancreatic alpha cells [24].
Effects of Diabetes on Thyroid Disorders
Diabetes affects thyroid function by altering the thyroid-stimulating hormone (TSH) level and impairing the conversion of thyroxine (T4) to triiodothyronine (T3) in the peripheral tissues [21, 25]. In euthyroid DM patients, the nocturnal TSH peak is absent or reduced and the TSH response to thyrotropin-releasing hormone (TRH) is also impaired. Hyperglycaemia of longer duration can have a cumulative effect on TD [25]. While interpreting thyroid function tests, it is important to consider that, like other acute systemic illnesses, diabetic ketoacidosis can decrease T3 and T4 levels while TSH levels remain normal [26]. Insulin resistance and hyperinsulinaemia lead to proliferation of thyroid tissues, an increased incidence of nodular thyroid disease, and a larger goitre [21, 27].
In hypothyroid patients with coexisting diabetes, the efficacy of thyroid hormone treatment may be affected [21]. T1DM is more common in patients with Graves’ orbitopathy (GO) than in the normal population [21]; GO is more frequent and severe in Graves’ disease patients with T2DM and is significantly associated with duration, obesity, and vasculopathy [28]. Diabetic patients with GO also have a higher incidence of dysthyroid optic neuropathy than nondiabetics [21].
Diabetes Mellitus, Thyroid Dysfunction, and Pregnancy
Maternal and foetal health can be affected by both DM and TD. A significantly higher prevalence of hypothyroxinaemia is found in women with gestational DM (GDM) [21, 29]. Also, the titre of anti-TPO is higher in pregnant women with T1DM [21]. Hypothyroidism can complicate the pregnancy and cause pregnancy-induced hypertension, preeclampsia, abruptio placentae, postpartum haemorrhage, impaired neurodevelopment of the infant, preterm delivery, and low birth weight [30, 31]. Children born to hypothyroid mothers or to those with GDM have impaired neuropsychological development [32, 33].
Postpartum TD occurs in up to one-quarter of women with T1DM [21]. Though thyroid antibodies may not increase GDM risk in pregnant euthyroid women, overt hypothyroidism during pregnancy increases the risk of developing diabetes later in life [34, 35]. Women with a history of GDM also have an increased risk of developing postpartum thyroiditis [36].
Subclinical Hypo- or Hyperthyroidism in Diabetes
In several studies, SCH accounts for a large proportion of the TD encountered in diabetes patients [7, 37,38,39,40]. Subclinical hyperthyroidism has also been reported in such patients, although less commonly than SCH [38, 39].
The clinical implications of subclinical hypo- or hyperthyroidism in DM will depend on the probability of progression to overt diabetes, metabolic control of diabetes, and the potential for benefits with thyroid hormone treatment [21]. SCH causes hypertension and hyperlipidaemia, affects insulin secretion, impairs both micro- and macrovascular function, and thereby increases the risk of diabetic nephropathy, retinopathy, peripheral arterial disease, and peripheral neuropathy [41,42,43]. SCH may, however, have a protective effect on noncardiovascular mortality in T2DM [44].
Thyroid Nodules and Carcinoma in Diabetes
The association between T2DM and the incidence of thyroid cancer is a topic of debate. A large prospective cohort study found an increased incidence of differentiated thyroid cancer among diabetic women [45]. The risk was not elevated in men. Another large prospective study [46] as well as a pooled analysis of several prospective studies [47] found no significant association between diabetes and thyroid cancer. A previous literature review had suggested that any association between T2DM and thyroid cancer was probably weak [48]. More recent meta-analyses have found a 1.38-fold-increased risk for thyroid cancer in women with pre-existing diabetes [49] and a 20% increase in thyroid cancer in DM patients [50] compared to their nondiabetic counterparts. In a Korean study, however, early T2DM patients had a low incidence of thyroid cancer, with the effect lasting up to 6 years after the T2DM was first diagnosed [51]. A retrospective study published in December 2018 found a significantly higher risk of thyroid cancer among Chinese women with T2DM [52].
Glycated Albumin Levels
Glycated albumin, like glycated haemoglobin, is used as an indicator for glycaemic control in diabetes. It is affected by both glucose metabolism and albumin metabolism. Thyroid hormone promotes albumin catabolism, so the glycated albumin level may also be altered by TD [24]. Careful assessment of the glycated albumin in diabetics with TD is needed.
Seaweed in the Diet
Seaweed is a common ingredient of Asian cuisine. Its use is highly recommended in the diets of those with diabetes, as it is low in calories and high in fibre, and has a high mineral content. However, seaweed has a high iodine content and can precipitate TD in susceptible patients [24].
Effect of Drugs on Thyroid Function and Glycaemic Control
Drugs administered for diabetes, TD, and other comorbidities can alter thyroid function or glycaemic control in persons with coexisting T2DM and TD (Table 3). Dose adjustments or a change in treatment regimen may be required.
There are also reports of increased incidence of thyroid cancer with antidiabetic drugs such as incretin mimetics and insulin analogues. However, the evidence is not strong enough to discourage the use of these antidiabetic medications [59, 60].
Role of Thyroid Hormone Analogues
Thyroid hormones affect the metabolism of lipids, proteins, and carbohydrates. Strategies are being explored for the use of thyroid hormone analogues in the management of diabetes, obesity, and atherosclerosis [24, 61]. Researchers are searching for potent thyromimetics that can exert the desired therapeutic effects without producing the harmful effects of thyroid hormones.
Simplified Screening Strategy
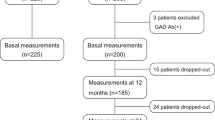
Although current guidelines on the annual screening of T2DM patients for TD are not consistent, there is no doubt that patients with diabetes are at increased risk for thyroid disorders. Unrecognized TD can worsen glycaemic control and increase the cardiovascular risk in T2DM. Kadiyala et al. recommend that all patients of diabetes should be screened for TSH and anti-TPO at baseline [62]. In euthyroid T1DM, annual TSH screening is required for all patients. In euthyroid T2DM patients, an annual TSH test is only needed in those with TSH ≥ 2.0 mU/L or detectable anti-TPO. In others, a TSH test is recommended every 3–5 years (Fig. 1).
Simplified algorithm for thyroid screening in diabetes (modified from Kadiyala et al. [62]). T1DM type 1 diabetes mellitus, T2DM type 2 diabetes melliltus, TSH thyroid-stimulating hormone, anti-TPO thyroid peroxidase antibody
Conclusion
An increased prevalence of TD is being seen among patients with T2DM. In many studies, thyroid function tests have revealed that a substantial proportion of the new T2DM patients with TD have subclinical hypothyroidism. International guidelines vary widely and do not specifically suggest routine screening for this milder form of TD in T2DM patients. Coexistent T2DM and TD pose a higher cardiovascular disease risk. Insulin resistance links these conditions. TD can worsen T2DM and diabetes can worsen thyroid function. Antidiabetic drugs can alter thyroid function, and antithyroid drugs can alter glycaemic control. Considering the clinical implications of the coexistence of T2DM and TD, a more systematic approach to thyroid testing in T2DM is needed. Regular monitoring of glycaemic control in thyroid dysfunction is also suggested. More research is warranted to study the relationship between T2DM and TD.
References
Nederstigt C, Corssmit EPM, de Koning EJP, Dekkers OM. Incidence and prevalence of thyroid dysfunction in type 1 diabetes. J Diabetes Complicat. 2016;30:420–5.
Gu Y, Li H, Bao X, Zhang Q, Liu L, Meng G, et al. The relationship between thyroid function and the prevalence of type 2 diabetes mellitus in euthyroid subjects. J Clin Endocrinol Metab. 2017;102:434–42.
International Diabetes Federation. IDF Diabetes Atlas. 2017. https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html. Accessed 11 Feb 2019.
Garmendia Madariaga A, Santos Palacios S, Guillén-Grima F, Galofré JC. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clin Endocrinol Metab. 2014;99:923–31.
Centeno Maxzud M, Gómez Rasjido L, Fregenal M, Arias Calafiore F, Córdoba Lanus M, D’Urso M, et al. Prevalence of thyroid dysfunction in patients with type 2 diabetes mellitus. Medicina (Mex). 2016;76:355–8.
Subekti I, Pramono LA, Dewiasty E, Harbuwono DS. Thyroid dysfunction in type 2 diabetes mellitus patients. Acta Med Indones. 2017;49:10.
Palma CC, Pavesi M, Nogueira VG, Clemente ELS, Vasconcellos M, de Faria Bello MP, Pereira LC, et al. Prevalence of thyroid dysfunction in patients with diabetes mellitus. Diabetol Metab Syndr. 2013;5:58.
Ozair M, Noor S, Raghav A, Siddiqi SS, Chugtai AM, Ahmad J. Prevalence of thyroid disorders in North Indian type 2 diabetic subjects: a cross sectional study. Diabetes Metab Syndr. 2018;12:301–4.
Jali MV, Kambar S, Jali SM, Pawar N, Nalawade P. Prevalence of thyroid dysfunction among type 2 diabetes mellitus patients. Diabetes Metab Syndr. 2017;11(Suppl 1):S105–8.
Witting V, Bergis D, Sadet D, Badenhoop K. Thyroid disease in insulin-treated patients with type 2 diabetes: a retrospective study. Thyroid Res. 2014;7:2.
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27:315–89.
National Institute of Healthcare and Excellence. Type 2 diabetes in adults: management. 2015. https://www.nice.org.uk/guidance/ng28/resources/type-2-diabetes-in-adults-management-pdf-1837338615493. Accessed 14 Feb 2019.
American Diabetes Association. Standards of medical care in diabetes—2017. 2017. https://professional.diabetes.org/sites/professional.diabetes.org/files/media/standardofcare2017fulldeckfinal_0.pdf. Accessed 14 Feb 2019.
British Thyroid Association, The Association for Clinical Biochemistry. British Thyroid Association and Association of Clinical Biochemistry guidelines. 2006. http://www.btf-thyroid.org/images/documents/tft_guideline_final_version_july_2006.pdf. Accessed 13 Feb 2019.
Garber J, Cobin R, Gharib H, Hennessey J, Klein I, Mechanick J, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18:988–1028.
Guastamacchia E, Triggiani V, Aglialoro A, Aiello A, Ianni L, Maccario M, et al. Italian Association of Clinical Endocrinologists (AME) & Italian Association of Clinical Diabetologists (AMD) position statement: diabetes mellitus and thyroid disorders: recommendations for clinical practice. Endocrine. 2015;49:339–52.
Ladenson PW, Singer PA, Ain KB, Bagchi N, Bigos ST, Levy EG, et al. American Thyroid Association guidelines for detection of thyroid dysfunction. Arch Intern Med. 2000;160:1573–5.
US Preventive Services Task Force. Final update summary: thyroid dysfunction: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/thyroid-dysfunction-screening. Accessed 14 Feb 2019.
Ward RJ, Heald AH, Ogunmekan S, Fryer AA, Duff CJ. Should we be screening for thyroid dysfunction in patients with type 2 diabetes mellitus? Br J Gen Pract. 2018;68:94–5.
Wang C. The relationship between type 2 diabetes mellitus and related thyroid diseases. J Diabetes Res. 2013;390534. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647563/.
Ray S, Ghosh S. Thyroid disorders and diabetes mellitus: double trouble. J Diabetes Res Ther. 2016;2:1–7.
Hage M, Zantout MS, Azar ST. Thyroid disorders and diabetes mellitus. J Thyroid Res. 2011;439463. https://www.hindawi.com/journals/jtr/2011/439463/.
Chen H-H, Yeh S-Y, Lin C-L, Chang S-N, Kao C-H. Increased depression, diabetes and diabetic complications in Graves’ disease patients in Asia. QJM Int J Med. 2014;107:727–33.
Nishi M. Diabetes mellitus and thyroid diseases. Diabetol Int. 2018;9:108–12.
Nair A, Jayakumari C, Jabbar PK, Jayakumar RV, Raizada N, Gopi A, et al. Prevalence and associations of hypothyroidism in Indian patients with type 2 diabetes mellitus. J Thyroid Res. 2018;5386129. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6106958/.
Mirboluk AA, Rohani F, Asadi R, Eslamian MR. Thyroid function test in diabetic ketoacidosis. Diabetes Metab Syndr. 2017;11(Suppl 2):S623–5.
Tang Y, Yan T, Wang G, Chen Y, Zhu Y, Jiang Z, et al. Correlation between insulin resistance and thyroid nodule in type 2 diabetes mellitus. Int J Endocrinol. 2017;1617458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5660821/.
Le Moli R, Muscia V, Tumminia A, Frittitta L, Buscema M, Palermo F, et al. Type 2 diabetic patients with Graves’ disease have more frequent and severe Graves’ orbitopathy. Nutr Metab Cardiovasc Dis. 2015;25:452–7.
Iranparvar M, Ghorbani H, Azami A, Darvishkhah H. Thyroid dysfunction and autoimmunity in pregnant women with gestational diabetes mellitus: a cross-sectional study. Int J Adv Med. 2017;2:350–3.
Velkoska Nakova V, Krstevska B, Dimitrovski C, Simeonova S, Hadzi-Lega M, Serafimoski V. Prevalence of thyroid dysfunction and autoimmunity in pregnant women with gestational diabetes and diabetes type 1. Prilozi. 2010;31:51–9.
Tirosh D, Benshalom-Tirosh N, Novack L, Press F, Beer-Weisel R, Wiznitzer A, et al. Hypothyroidism and diabetes mellitus—a risky dual gestational endocrinopathy. Peer J. 2013;1:e52.
Ramprasad M, Bhattacharyya SS, Bhattacharyya A. Thyroid disorders in pregnancy. Indian J Endocrinol Metab. 2012;16:S167–70.
Cai S, Qiu A, Broekman BFP, Wong EQ, Gluckman PD, Godfrey KM, et al. The influence of gestational diabetes on neurodevelopment of children in the first two years of life: a prospective study. PLoS One. 2016;11(9):e0162113. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5014336/.
Mannisto T, Vääräsmäki M, Pouta A, Hartikainen A-L, Ruokonen A, Surcel H-M, et al. Thyroid dysfunction and autoantibodies during pregnancy as predictive factors of pregnancy complications and maternal morbidity in later life. J Clin Endocrinol Metab. 2010;95:1084–94.
Yang Y, Li Q, Wang Q, Ma X. Thyroid antibodies and gestational diabetes mellitus: a meta-analysis. Fertil Steril. 2015;104(665–671):e3.
Maleki N, Tavosi Z. Evaluation of thyroid dysfunction and autoimmunity in gestational diabetes mellitus and its relationship with postpartum thyroiditis. Diabet Med J Br Diabet Assoc. 2015;32:206–12.
Khatiwada S, Kc R, Sah SK, Khan SA, Chaudhari RK, Baral N, et al. Thyroid dysfunction and associated risk factors among Nepalese diabetes mellitus patients. Int J Endocrinol. 2015;570198. https://www.hindawi.com/journals/ije/2015/570198/.
Khatiwada S, Sah SK, KC R, Baral N, Lamsal M. Thyroid dysfunction in metabolic syndrome patients and its relationship with components of metabolic syndrome. Clin Diabetes Endocrinol. 2016;2:3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5471726/.
Demitrost L, Ranabir S. Thyroid dysfunction in type 2 diabetes mellitus: a retrospective study. Indian J Endocrinol Metab. 2012;16:S334–5.
Khan NZ, Muttalib MA, Sultana GS, Mishu FA, Nesa A. Study of thyroid disorders among type 2 diabetic patients attending a tertiary care hospital. Mymensingh Med J MMJ. 2017;26:874–8.
Wang J, Li H, Tan M, Gao G, Zhang Y, Ding B, et al. Association between thyroid function and diabetic nephropathy in euthyroid subjects with type 2 diabetes mellitus: a cross-sectional study in China. Oncotarget. 2019;10:88–97.
Wu J, Yue S, Geng J, Liu L, Teng W, Liu L, et al. Relationship between diabetic retinopathy and subclinical hypothyroidism: a meta-analysis. Sci Rep. 2015;5:12212.
Han C, He X, Xia X, Li Y, Shi X, Shan Z, et al. Subclinical hypothyroidism and type 2 diabetes: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0135233. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4535849/.
Sathyapalan T, Manuchehri AM, Rigby AS, Atkin SL. Subclinical hypothyroidism is associated with reduced all-cause mortality in patients with type 2 diabetes. Diabetes Care. 2010;33:e37.
Aschebrook-Kilfoy B, Sabra MM, Brenner A, Moore SC, Ron E, Schatzkin A, et al. Diabetes and thyroid cancer risk in the National Institutes of Health-AARP Diet and Health Study. Thyroid Off J Am Thyroid Assoc. 2011;21:957–63.
Luo J, Phillips L, Liu S, Wactawski-Wende J, Margolis KL. Diabetes, diabetes treatment, and risk of thyroid cancer. J Clin Endocrinol Metab. 2016;101:1243–8.
Kitahara CM, Platz EA, Beane Freeman LE, Black A, Hsing AW, Linet MS, et al. Physical activity, diabetes, and thyroid cancer risk: a pooled analysis of five prospective studies. Cancer Causes Control. 2012;23:463–71.
Shih S-R, Chiu W-Y, Chang T-C, Tseng C-H. Diabetes and thyroid cancer risk: literature review. J Diabetes Res. 2012;578285. https://www.hindawi.com/journals/jdr/2012/578285/abs/.
Yeo Y, Ma S-H, Hwang Y, Horn-Ross PL, Hsing A, Lee K-E, et al. Diabetes mellitus and risk of thyroid cancer: a meta-analysis. PLoS One. 2014;9:e98135.
Li H, Qian J. Association of diabetes mellitus with thyroid cancer risk. Medicine (Baltimore). 2017;96(47):e8230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5708911/.
Seo Y-G, Choi H-C, An AR, Park DJ, Park YJ, Lee KE, et al. The association between type 2 diabetes mellitus and thyroid cancer. J. Diabetes Res. 2017. https://www.hindawi.com/journals/jdr/2017/5850879/. Accessed 30 Sept 2019.
Fang Y, Zhang X, Xu H, Smith-Warner SA, Xu D, Fang H, et al. Cancer risk in Chinese diabetes patients: a retrospective cohort study based on management data. Endocr Connect. 2018;7:1415–23.
Meng X, Xu S, Chen G, Derwahl M, Liu C. Metformin and thyroid disease. J Endocrinol. 2017;233:R43–51.
Anil C, Kut A, Atesagaoglu B, Nar A, Tutuncu NB, Gursoy A. Metformin decreases thyroid volume and nodule size in subjects with insulin resistance: a preliminary study. Med Princ Pract. 2016;25:233–6.
Tseng C-H. Thyroid cancer risk is not increased in diabetic patients. PLoS One. 2012;7:e53096.
Arnetz L, Lantz M, Brismar K, Ekberg NR, Alvarsson M, Dorkhan M. Effect of pioglitazone on thyroid hormones and IGF-I in patients with type 2 diabetes. J Thyroid Disord Ther. 2013;3:1. http://www.omicsgroup.org/journals/effect-of-pioglitazone-on-thyroid-hormones-and-igfi-in-patients-with-type-diabetes-2167-7948-3-139.php?aid=21564.
Gutch M, Bhattacharyya A, Kumar S, Pahan RK, Singh RS. Unusual antithyroid drug-induced hypoglycemia. CHRISMED J Health Res. 2017;4(3):198–200. http://www.cjhr.org/article.asp?issn=2348-3334;year=2017;volume=4;issue=3;spage=198;epage=200;aulast=Gutch.
BilicKomarica E, Beciragic A, Junuzovic D. Effects of treatment with l-thyroxin on glucose regulation in patients with subclinical hypothyroidism. Med Arch. 2012;66:364.
Nauck MA, Friedrich N. Do GLP-1-based therapies increase cancer risk? Diabetes Care. 2013;36:S245–52.
He L, Zhang S, Zhang X, Liu R, Guan H, Zhang H. Effects of insulin analogs and glucagon-like peptide-1 receptor agonists on proliferation and cellular energy metabolism in papillary thyroid cancer. OncoTargets Ther. 2017;10:5621–31.
Shoemaker TJ, Kono T, Mariash CN, Evans-Molina C. Thyroid hormone analogues for the treatment of metabolic disorders: new potential for unmet clinical needs? Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2012;18:954–64.
Kadiyala R, Peter R, Okosieme OE. Thyroid dysfunction in patients with diabetes: clinical implications and screening strategies. Int J Clin Pract. 2010;64:1130–9.
Acknowledgements
The views expressed in this article are independent views of the authors and not of Abbott India Ltd.
Funding
This review and the journal’s Rapid Service Fee were funded by Abbott India Ltd.
Medical Writing Assistance
Writing assistance was provided by Dr Natasha Das (Freelance Medical Writer, Delhi, India) through academic funding from Abbott India Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sanjay Kalra is a member of the journal’s Editorial Board. Sameer Aggarwal and Deepak Khandelwal have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.9878615.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kalra, S., Aggarwal, S. & Khandelwal, D. Thyroid Dysfunction and Type 2 Diabetes Mellitus: Screening Strategies and Implications for Management. Diabetes Ther 10, 2035–2044 (2019). https://doi.org/10.1007/s13300-019-00700-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-00700-4