Abstract
Aims
To examine the association of baseline patient characteristics with study outcomes in people with type 2 diabetes receiving insulin glargine 300 U/mL (Gla-300) versus glargine 100 U/mL (Gla-100), over a 6-month period.
Methods
A post hoc patient-level meta-analysis using data from three multicenter, randomized, open-label, parallel-group, phase 3a studies of similar design, in people previously receiving either basal and prandial insulin, basal insulin + oral antihyperglycemic drugs, or no prior insulin (EDITION 1, 2 and 3, respectively). The endpoints, glycated hemoglobin (HbA1c), hypoglycemia, body weight change, and insulin dose were investigated by subgroups: age (< 65 and ≥ 65 years), body mass index (BMI; < 30 and ≥ 30 kg/m2), age at onset (< 40, 40–50, and > 50 years), and diabetes duration (< 10 and ≥ 10 years).
Results
Reduction in HbA1c was comparable between insulins, regardless of subgroup. The lower risk of ≥ 1 nocturnal (00:00–05:59 h) confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemic event with Gla-300 versus Gla-100 was also unaffected by participant characteristics. While heterogeneity of treatment effect between diabetes duration subgroups was seen for the risk of ≥ 1 confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemic event at any time (24 h), treatment effect consistently favored Gla-300; no evidence of heterogeneity was observed for the other subgroups. Annualized rates of confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemia and body weight change were not influenced by participant characteristics; a similar pattern was observed with insulin dose.
Conclusions
Comparable glycemic control was observed with Gla-300 versus Gla-100, with less hypoglycemia, regardless of age, BMI, age at onset or diabetes duration.
Funding
Sanofi.
Plain Language Summary
Plain language summary available for this article.
Similar content being viewed by others
Plain Language Summary
Treatments for patients with type 2 diabetes aim to reduce the levels of blood glucose and can include injections with insulin. However, care must be taken to prevent blood glucose levels falling too low (a state called hypoglycemia). Previous studies have shown that insulin glargine 300 units/mL (Gla-300) provides similar reductions in blood glucose levels as insulin glargine 100 units/mL (Gla-100) but is less likely to cause hypoglycemia. However, different patients may respond differently to treatments depending on their individual clinical and biological characteristics. The aim of this study was to evaluate how different profiles of patients with type 2 diabetes responded to Gla-300 and Gla-100 injections. Patients were grouped by different ages, weights, age at diabetes diagnosis, and number of years since diagnosis of diabetes. We found that Gla-300 and Gla-100 reduced glycated hemoglobin (HbA1c; a marker of blood glucose control over the previous 2–3 months) similarly, regardless of how patients were grouped. However, patients treated with Gla-300 were less likely to experience hypoglycemia than those treated with Gla-100, and this association was also true regardless of different patient characteristics. We therefore concluded that Gla-300 is an effective and safe treatment in patients with type 2 diabetes, regardless of their age, weight, age at diabetes diagnosis, and years since diagnosis.
Introduction
Type 2 diabetes (Type 2 DM) is a heterogeneous disease, with a population that exhibits diverse clinical and biological characteristics [1, 2]. Current recommendations for the management of Type 2 DM encourage a patient-centered approach [3], such that less stringent glycemic targets (e.g. glycated hemoglobin [HbA1c] < 64 mmol/mol [8.0%]) may be considered on an individual basis [4], to take into account, for example, factors such as polypharmacy, comorbidities, frailty, renal disease, and reduced life expectancy found to be associated with increased risk of hypoglycemia. To most appropriately individualize treatments and glycemic targets, it is important to understand how the characteristics of each individual might affect the outcomes of treatment. Studies investigating potential predictors of response have highlighted several demographic and clinical factors that may influence the effectiveness of particular diabetes therapies, as well as the attainment of glycemic targets [5,6,7,8].
Insulin glargine 300 U/mL (Gla-300; Toujeo®; Sanofi S.A., Paris, France) is a long-acting basal insulin analog with prolonged and more stable pharmacokinetic and pharmacodynamic profiles than insulin glargine 100 U/mL (Gla-100; Lantus®; Sanofi S.A.) [9]. The EDITION program included three multinational clinical studies that compared the efficacy and safety of Gla-300 to those of Gla-100 in different populations of people with Type 2 DM [10,11,12]. In the individual EDITION studies and a post hoc, patient-level meta-analysis, Gla-300 provided comparable glycemic control to Gla-100 with fewer hypoglycemia events over 6 months of treatment [10,11,12,13]. Change in body weight was low in both treatment groups, with slightly less weight gain in patients receiving Gla-300 [10,11,12,13].
The objective of the current post hoc analysis was to investigate the potential association of participant characteristics with key outcomes reported from the EDITION 1–3 trials, in Type 2 DM participants randomized to Gla-300 or Gla-100. The characteristics chosen for this post hoc analysis were those previously reported to influence glycemic control in participants with Type 2 DM [5,6,7,8]. For example, age, body weight, and duration of diabetes have been shown to be associated with change in HbA1c [5]. Similarly, multivariate analyses in individuals with Type 2 DM showed a higher success rate of achieving glycemic control targets in older participants, those with higher body mass index (BMI), and those with a shorter duration of diabetes [7]. In addition, older people with Type 2 DM are at a greater risk of hypoglycemia than are younger individuals [14]. In the current analysis, glycemic control, hypoglycemia, and body weight were assessed in subgroups of participants defined by age, BMI, age at onset of diabetes, and duration of diabetes, in a patient-level meta-analysis of data from the three trials over a 6-month period.
Methods
Study Design
This post hoc analysis was performed on patient-level data from the EDITION 1, EDITION 2, and EDITION 3 studies. EDITION 1, 2, and 3 were multicenter, randomized, open-label, two-arm, parallel-group, phase 3a studies with 6-month treatment periods (NCT01499082, NCT01499095, and NCT01676220, respectively), the study designs of which have been described previously [10,11,12]. All participants were ≥ 18 years of age with a diagnosis of Type 2 DM (according to World Health Organization criteria) [15], and prior to study enrolment they were receiving either basal (≥ 42 units/day) and prandial insulin therapy with or without metformin for at least 1 year (EDITION 1) [10], at least 6 months of basal insulin treatment (≥ 42 units/day) in combination with oral antihyperglycemic drugs (OADs) (EDITION 2) [11], or at least 6 months of OADs and were insulin naïve (EDITION 3) [12]. In the EDITION 2 and 3 studies, participants discontinued the use of sulphonylurea 2 months prior to screening and at baseline, respectively. In all three studies, participants were randomized (1:1) to receive once-daily evening injections of either Gla-300 or Gla-100, and they were titrated to a fasting self-monitored plasma glucose target of 4.4–5.6 mmol/L (80–100 mg/dL).
For the current analysis, the patient-level dataset from EDITION 1, 2, and 3 was grouped according to baseline: age (< 65 and ≥ 65 years), BMI (< 30 and ≥ 30 kg/m2), age at onset of diabetes (< 40, 40–50, and > 50 years), and diabetes duration (< 10 and ≥ 10 years). The cut-offs in the age at onset analysis, which were not predefined, were chosen to be clinically meaningful, while limiting the difference in sample size between subgroups.
Outcomes
The analysis was carried out for the following endpoints, from baseline to treatment month 6: change in HbA1c (%); number and percentage of participants with at least one hypoglycemic event, and annualized rates of hypoglycemia (events per participant-year), both nocturnal (00:00–05:59 h) and at any time of day (24 h), and change in body weight. Daily basal insulin dose and change in dose from baseline to treatment month 6 was also reported by subgroup.
Hypoglycemia was defined as confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe, or as documented symptomatic (≤ 3.9 mmol/L [≤ 70 mg/dL]), based on American Diabetes Association (ADA) categories described at the time when the EDITION studies were undertaken [16]. The confirmed or severe definition of hypoglycemia combined three ADA categories: documented symptomatic hypoglycemia, asymptomatic hypoglycemia, and severe hypoglycemia.
Data Analysis and Statistics
For each endpoint considered, differences of treatment effect across subgroups were assessed with a heterogeneity test. Differences of treatment effect across subgroups were only considered to be relevant if evidence of heterogeneity was observed (p < 0.05). The p values of the heterogeneity test were generated using a subgroup-by-treatment interaction.
Change in HbA1c was analyzed using a mixed model for repeated measurements. The percentage of participants with at least one hypoglycemic event was analyzed using the Cochran–Mantel–Haenszel method, and annualized rates of hypoglycemia (events per participant-year) were analyzed using an over-dispersed Poisson regression model. Change in body weight was assessed using an analysis of covariance model (ANCOVA), from baseline to last on-treatment value. Daily basal insulin dose was assessed using descriptive statistics.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the appropriate local or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Results
Baseline Characteristics
In total, 2496 participants were included in this patient-level meta-analysis of the three EDITION Type 2 DM studies, of whom 1247 were randomized to Gla-300 and 1249 were randomized to Gla-100. Baseline characteristics of this study population have been reported previously [13] and are summarized together with the age at onset of diabetes in Table 1. Mean age, BMI, age at onset of diabetes, and diabetes duration were similar in both treatment arms.
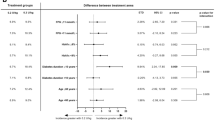
Glycemic Control
Reduction in HbA1c over the 6-month study period was comparable between the Gla-300 and Gla-100 treatment arms, regardless of age, BMI, age at onset of diabetes, or diabetes duration (Fig. 1). These findings were consistent with the overall pooled study population. No evidence of heterogeneity of treatment effect across subgroups was observed over the 6-month treatment period (p > 0.05).
Reduction in glycated hemoglobin (HbA1c [%]) in people with type 2 diabetes (Type 2 DM) over 6 months of treatment by subgroup (mITT population; pooled data from EDITION 1, 2 and 3). *Diabetes duration not available for 8 participants. BMI Body mass index, CI confidence interval, Gla-300/Gla-100 insulin glargine 300 units/mL/insulin glargine 100 units/mL, LS least squares, mITT modified intent-to-treat
Hypoglycemia
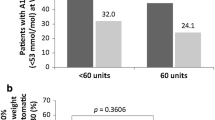
The lower risk of nocturnal (00:00–05:59 h) confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemia with Gla-300 versus Gla-100 seen in the overall pooled study population was not affected by age, BMI, age at onset of diabetes, or diabetes duration, as no evidence of heterogeneity of treatment effect across subgroups was seen over the 6-month treatment period (p > 0.05; Fig. 2a). Similarly, the lower risk of confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemia at any time of day (24 h) with Gla-300 versus Gla-100 was not affected by age, BMI, or age at onset of diabetes (no evidence of heterogeneity of treatment effect across subgroups: p > 0.05; Fig. 2b). For the diabetes duration subgroup analysis, some degree of heterogeneity of treatment effect was observed between participants with a diabetes duration of < 10 years and those with a diabetes duration of ≥ 10 years (p = 0.006), although the treatment benefit was consistently in favor of Gla-300 regardless of diabetes duration (Fig. 2b).
Relative risk (RR) of experiencing confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemia during the night (00:00–05:59 h) (a) and at any time of day (24 h) (b), over 6 months of treatment by subgroup (% participants with ≥ 1 event; safety population; pooled data from EDITION 1, 2, and 3). *Diabetes duration not available for 8 participants
When confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemic events were considered in terms of annualized rates (events per participant-year), no evidence of heterogeneity of treatment effect was observed across any subgroups, either at night (00:00–05:59 h) or at any time of day (24 h) (p > 0.05; Fig. 3a, b).
Annualized rates of confirmed (≤ 3.9 mmol/L [≤ 70 mg/dL]) or severe hypoglycemia during the night (00:00–05:59 h) (a) and at any time of day (24 h) (b), over 6 months of treatment by subgroup (events per participant-year; safety population; pooled data from EDITION 1, 2, and 3). *Diabetes duration not available for 8 participants. RR rate ratio
Similar findings were observed for documented symptomatic (≤ 3.9 mmol/L [≤ 70 mg/dL]) hypoglycemia, both in terms of relative risk and rate ratios; however, some degree of heterogeneity of treatment effect was observed for annualized rates at any time of day (24 h) between participants with a BMI of < 30 kg/m2 and those with a BMI of ≥ 30 kg/m2 (p = 0.037; Electronic Supplementary Material ([ESM] Figs. S1–2).
The risk of at least one severe hypoglycemic event at any time of day (24 h) was comparable between the Gla-300 and Gla-100 treatment arms, regardless of age, BMI, age at onset of diabetes, or diabetes duration (ESM Fig. S3). No evidence of heterogeneity of treatment effect across subgroups was observed for all subgroups (ESM Fig. S3).
Body Weight
Over the 6-month treatment period, change in body weight was comparable between subgroups, with a trend for slightly less weight gain in those patients on Gla-300 compared with those on Gla-100 (Table 2). No evidence of heterogeneity of treatment effect was observed in the age, BMI, age at onset of diabetes, or diabetes duration subgroups (p = 0.486, 0.942, 0.566, 0.663, respectively).
Insulin Dose
Daily basal insulin dose increased over the 6-month treatment period in both treatment groups, with a slightly higher dose (10–16%) at treatment month 6 for Gla-300 compared with Gla-100 in each of the subgroups (ESM Table S1). The treatment difference in change from baseline to month 6 was generally comparable across the subgroups (ESM Table S1).
Discussion
Guidelines for the management of Type 2 DM recommend a patient-centered approach that considers the needs and preferences of each individual [3]. The outcomes of diabetes treatment can differ depending on an individual’s characteristics [5,6,7, 17]. The objective of this post hoc analysis of the EDITION studies was to examine the association between participant characteristics and study outcomes in people with Type 2 DM receiving Gla-300 versus Gla-100. Glycemic control was comparable between the treatment groups, as expected in a ‘treat-to-target’ study, but there was less nocturnal hypoglycemia in patients on Gla-300 than in those on Gla-100 regardless of participant age, BMI, age at onset of diabetes, or duration of diabetes. The benefits of Gla-300 observed across these subgroups were consistent with those observed in the overall pooled study population.
The heterogeneity of treatment effect observed across the diabetes duration subgroups (for risk of hypoglycemia at any time of day [24 h]) suggests that Gla-300 may be particularly beneficial in reducing hypoglycemia in people with a longer duration of diabetes (≥ 10 years) compared with Gla-100. However, these findings may have been driven by differences in the study populations reflecting the individual study inclusion criteria. Participants with a diabetes duration of < 10 years are most likely to have been from the EDITION 3 study, which enrolled insulin-naïve people with a mean diabetes duration of 10 years [12]. In contrast, the mean durations of diabetes in EDITION 1 and EDITION 2 were 16 years and 13 years, respectively [10, 11]. Other differences between the individual study populations could also have affected these findings; for example, the use of mealtime insulin in EDITION 1, which would have been overrepresented in the ≥ 10 years diabetes duration group, may have impacted hypoglycemia occurring during the day. However, it is interesting to note that there was a trend towards heterogeneity of treatment effect across the diabetes duration subgroups for change in HbA1c. It is therefore possible that the heterogeneity between the diabetes duration subgroups was due to a difference in treatment approaches in the two subgroups of participants—as those with a longer duration of diabetes are a more complex population and more likely to have a greater pharmacological treatment burden at baseline and an increased risk of hypoglycemia—rather than simply a difference between the treatments used.
Although a heterogeneity of treatment effect was observed between BMI subgroups for annualized rates of documented symptomatic (≤ 3.9 mmol/L [≤ 70 mg/dL]) hypoglycemia at any time of day (24 h), the benefit of Gla-300 versus Gla-100 (in terms of direction of effect) was apparent in both BMI subgroups.
An earlier age at onset of diabetes has also been associated with higher HbA1c [8], as well as being linked to a greater risk of diabetes complications, such as diabetic retinopathy and more severe albuminuria, in people with Type 2 DM [18, 19]. In the current analysis, those with an earlier age at onset showed a trend towards having higher baseline BMI and body weight (ESM Table S2), which may suggest a specific phenotype for this subgroup; however, this may be expected based on the pathophysiology of diabetes, and further analysis is required to confirm this.
There was a trend for lower weight gain in patients on Gla-300 compared with those on Gla-100, as observed in the EDITION studies [10, 12, 13, 20], and no evidence of heterogeneity of treatment effect across the subgroups of participant characteristics was observed. As also previously observed in the EDITION studies [10, 12, 13, 20], a slightly higher mean basal insulin dose was seen at month 6 with Gla-300 compared with Gla-100. In the current analysis, insulin dose profiles appeared to be unaffected by participant characteristics, although this parameter was not assessed statistically.
The limitations of this study include the post hoc exploratory nature of the analysis. An imbalance in the number of participants across the subgroups may have introduced some bias within the analysis. Nevertheless, the cut-offs chosen are meant to demonstrate the lack of association between these participant characteristics and treatment outcomes with Gla-300 versus Gla-100. Furthermore, the age cut-off (≥ 65 years) is aligned with that used throughout the ADA guidelines for the treatment of older people with diabetes [21]. In addition, other imbalances between subgroups may have affected the results. For example, the age at onset of diabetes subgroup of participants < 40 years had a higher proportion of individuals from the EDITION 1 study than did the other studies. However, it should be noted that the cut-offs for the age at onset of diabetes subgroup were chosen to ensure a comparable number of participants in each subgroup. Finally, EDITION 3 contributed a greater proportion of participants to the subgroup BMI < 30 kg/m2 than did EDITION 1 and 2. These imbalances could have potentially impacted the results of risk/rates of hypoglycemia at any time of day, due to the use of prandial insulin therapy.
An individual’s characteristics may also influence the effectiveness of specific therapies; for example, metformin has been shown to be less effective than intensive lifestyle changes in people with low BMI and in older people [22, 23]. Given the potential impact on response to therapy, the profile of an individual can influence clinical decisions relating to disease management and treatment at the individual level. When considering initiating or switching to basal insulin therapy with Gla-300, it is reassuring that in this analysis the benefits of Gla-300 were consistent regardless of subgroup, suggesting that age, BMI, age at onset of diabetes, and diabetes duration are not important influencing factors for such treatment decisions.
Conclusion
The comparable glycemic control of Gla-300 versus Gla-100 with less hypoglycemia seen in the EDITION studies of people with Type 2 DM was observed irrespective of participant age, BMI, age at onset of diabetes, or duration of diabetes in this analysis.
References
Karalliedde J, Gnudi L. Diabetes mellitus, a complex and heterogeneous disease, and the role of insulin resistance as a determinant of diabetic kidney disease. Nephrol Dial Transplant. 2016;31:206–13.
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37[Suppl 1]:S81–90.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2018. Diabetes Care. 2018;41[Suppl 1]:S55–64.
Home PD, Shen C, Hasan MI, Latif ZA, Chen JW, Gonzalez Galvez G. Predictive and explanatory factors of change in HbA1c in a 24-week observational study of 66,726 people with type 2 diabetes starting insulin analogs. Diabetes Care. 2014;37:1237–45.
Hanefeld M, Fleischmann H, Schiffhorst G, Bramlage P. Predictors of response to early basal insulin treatment in patients with type 2 diabetes—the EARLY experience. Diabetes Technol Ther. 2014;16:241–6.
Mannucci E, Monami M, Dicembrini I, Piselli A, Porta M. Achieving HbA1c targets in clinical trials and in the real world: a systematic review and meta-analysis. J Endocrinol Invest. 2014;37:477–95.
Hsieh A, Ong PX, Molyneaux L, et al. Age of diabetes diagnosis and diabetes duration associate with glycated haemoglobin. Diabetes Res Clin Pract. 2014;104:e1–4.
Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units mL−1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units mL−1. Diabetes Care. 2015;38(4):637–43.
Riddle MC, Bolli GB, Ziemen M, Muehlen-Bartmer I, Bizet F, Home PD. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37:2755–62.
Yki-Jarvinen H, Bergenstal R, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37:3235–43.
Bolli GB, Riddle MC, Bergenstal RM, et al. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naive people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17:386–94.
Ritzel R, Roussel R, Bolli GB et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab 2015;17:859–67.
American Diabetes Association. 11. Older adults: standards of medical care in diabetes—2018. Diabetes Care. 2018;41[Suppl 1]:S119–25.
World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization. 1999.
ADA Workgroup on Hypoglycemia. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245–9.
Balkau B, Calvi-Gries F, Freemantle N, Vincent M, Pilorget V, Home PD. Predictors of HbA1c over 4 years in people with type 2 diabetes starting insulin therapies: the CREDIT study. Diabetes Res Clin Pract. 2015;108:432–40.
Wong J, Molyneaux L, Constantino M, Twigg SM, Yue DK. Timing is everything: age of onset influences long-term retinopathy risk in type 2 diabetes, independent of traditional risk factors. Diabetes Care. 2008;31:1985–90.
Al-Saeed AH, Constantino MI, Molyneaux L, et al. An inverse relationship between age of type 2 diabetes onset and complication risk and mortality: the impact of youth-onset type 2 diabetes. Diabetes Care. 2016;39:823–9.
Yki-Jarvinen H, Bergenstal R, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37:3235–43.
American Diabetes Association. Standards of medical care in diabetes—older adults. Diabetes Care. 2017;40:S99–104.
Crandall J, Schade D, Ma Y, et al. The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. J Gerontol A Biol Sci Med Sci. 2006;61:1075–81.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Acknowledgements
The authors thank the study participants, trial staff, and investigators for their participation, and Marie-Lise Grisoni (who provided consultancy for Sanofi while an employee of AIXIAL, Levalois-Perret, France) for the statistical analyses.
Funding
This study was sponsored by Sanofi, Paris, France. The article processing charges were also funded by Sanofi, Paris, France. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Editorial Assistance
Editorial assistance in the preparation of this article was provided by Matthew Robinson, DPhil, of Fishawack Communications, UK, and was funded by Sanofi.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Sanofi was the sponsor of the EDITION studies and was responsible for the design and coordination of the trials. Sanofi monitored the clinical sites and collected and managed the data. All authors participated in the interpretation of the results and in writing, reviewing, and editing the manuscript.
Disclosures
Stephen M. Twigg—Advisory panel: Abbott Diabetes Care, AstraZeneca, Boehringer Ingelheim, Novo Nordisk, Takeda, Eli Lilly, Abbott, Sanofi; Speakers bureau: Abbott Diabetes Care, AstraZeneca, MSD, Novartis, Novo Nordisk, Takeda, Sanofi. Javier Escalada—Advisory panel: MSD, Novo Nordisk, Sanofi; Speakers bureau: AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Novo Nordisk, Sanofi. Peter Stella—Employee: Sanofi. Ana Merino-Trigo—Employee: Sanofi; Stocks/shares: Sanofi. Fernando Lavalle-Gonzalez—Advisory panel: AstraZeneca, Boehringer Ingelheim, Janssen, Novo Nordisk, Eli Lilly, Sanofi; Speakers bureau: AstraZeneca, Boehringer Ingelheim, Janssen, MSD, Novo Nordisk, Eli Lilly, Sanofi; Board member: AstraZeneca, Boehringer Ingelheim, Janssen, Novo Nordisk, Sanofi. Bertrand Cariou—Advisory panel: Amgen, Eli Lilly, MSD, Novo Nordisk, Regeneron, Sanofi; Speakers bureau: Amgen, AstraZeneca, Pierre Fabre, Eli Lilly, Janssen, MSD, Novo Nordisk, Novartis, Regeneron, Sanofi. Luigi F. Meneghini—Advisory panel: Novo Nordisk, Sanofi, Intarcia; Consultant: Novo Nordisk, Sanofi.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the appropriate local or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.701676.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Twigg, S.M., Escalada, J., Stella, P. et al. Association of Patient Profile with Glycemic Control and Hypoglycemia with Insulin Glargine 300 U/mL in Type 2 Diabetes: A Post Hoc Patient-Level Meta-Analysis. Diabetes Ther 9, 2043–2053 (2018). https://doi.org/10.1007/s13300-018-0498-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-018-0498-x