Abstract
Introduction
Longer medication persistence in type 2 diabetes (T2D) is associated with improved glycaemic control. It is not clear which oral therapies have the best persistence. The objective of this study was to compare medication persistence across different oral therapies in people with T2D.
Methods
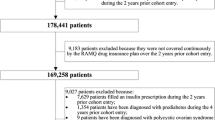
We performed a retrospective cohort analysis using a primary-care-based population, the Royal College of General Practitioners Research and Surveillance Centre cohort. We identified new prescriptions for oral diabetes medication in people with type 2 diabetes between January 1, 2004 and July 31, 2015. We compared median persistence across each class. We also compared non-persistence (defined as a prescription gap of ≥ 90 days) between classes, adjusting for confounders, using Cox regression. Confounders included: age, gender, ethnicity, socioeconomic status, alcohol use, smoking status, glycaemic control, diabetes duration, diabetes complications, comorbidities, and number of previous and concurrent diabetes medications.
Results
We identified 60,327 adults with T2D. The majority 42,810 (70.9%) of those had one or more oral medications prescribed; we measured persistence in those patients (who were prescribed 55,728 oral medications in total). Metformin had the longest median persistence (3.04 years; 95% CI 2.94–3.12). The adjusted hazard ratios for non-persistence compared with metformin were: sulfonylureas HR 1.20 (1.16–1.24), DPP-4 inhibitors HR 1.43 (1.38–1.49), thiazolidinediones HR 1.71 (95% CI 1.64–1.77), SGLT2 inhibitors HR 1.04 (0.93–1.17), meglitinides HR 2.25 (1.97–2.58), and alpha-glucosidase inhibitors HR 2.45 (1.98–3.02). The analysis of SGLT2 inhibitors was limited by the short duration of follow-up for this new class. Other factors associated with reduced medication persistence were female gender, younger age, and non-white ethnicity.
Conclusions
Persistence is strongly influenced by medication class and should be considered when initiating treatments.
Similar content being viewed by others
Introduction
Management of chronic disease often requires one or more medications to be taken over the full or partial life span of the disease. In this respect, treatment adherence and persistence should be given particular attention as failure to comply may result in earlier deterioration of the condition and sub-optimal outcomes [1]. In developed countries, adherence to therapies among patients suffering from chronic diseases averages 50%, and it is thought to be even less in developing countries due to reduced access to, and the limitations of, healthcare resources [1, 2]. With an aging population globally, the burden of people suffering from chronic diseases is expected to increase, resulting in poor health outcomes for individual patients and increases in healthcare costs leading to budgetary challenges for many governments [3, 4].
Poor adherence is a well-recognised problem among people with type 2 diabetes [5,6,7,8], with a high proportion of people failing to take their medication as prescribed [9, 10]. This can result in worse clinical outcomes, including poor glycaemic control [11,12,13,14,15,16], increased hospital admissions [17,18,19,20], increased healthcare costs [21,22,23,24,25,26,27], higher risk of cardiovascular events [28, 29], increased mortality [15, 18, 30,31,32], reduced health-related quality of life, and increased burden of diabetes. A meta-analysis by Krass et al. [33] reported a prevalence of adherence ranging from 38.5% to 93.1%, with the majority of studies (21/27) reporting good adherence in under 80% of people.
Several factors contribute to poor adherence: the World Health Organization (WHO) has identified five main categories [1]; patient-related (e.g. age), socioeconomic (e.g. medication costs), condition-related (e.g. presence of complications), health-system-related (e.g. level of continuity of care), and therapy-related (e.g. adverse effects) [12, 14]. There are two discrete patterns of medication non-use, which may be classed as missed medication doses (described by the terms adherence, compliance, or concordance) and duration of use before discontinuation (persistence) [34]. Accurate assessment of adherence and persistence behaviour, along with accurate data capture and analysis, are necessary for effective and efficient treatment planning, and for ensuring that changes in health outcomes can be attributed to the recommended regimen. Estimated level of persistence (ELPT) (the percentage of individuals remaining on therapy at a given time), the proportion of days covered (PDC) method (the number of days with the drug available divided by the number of days in the specified time interval), or the medication possession ratio (MPR) method (total days supply for all prescriptions filled within a period divided by the number of days in the specified time interval) are often used along with the number of days to discontinuation and number of prescription refills over a period of time [35, 36].
The aim of the study reported in the present paper was to compare persistence with various oral medications in type 2 diabetic patients, and to identify factors that influence persistence in a real-world setting using a primary-care-based population and with non-persistence defined as a prescription gap of ≥ 90 days.
Methods
We performed a retrospective cohort analysis in adults with type 2 diabetes to compare medication persistence across all noninsulin medication classes used in the treatment of hyperglycaemia. The cohort was identified from the Royal College of General Practitioners Research and Surveillance Centre (RCGP-RSC) database. This comprises primary care data from a sentinel network of general practices distributed across England. At the time of analysis, the database contained primary care records collected from 1,238,909 people registered with 128 practices. The database includes all recorded clinical codes with associated values and dates for the population from January 1, 2004 to January 1, 2015. These clinical codes are recorded using the Read coding system and include diagnosis codes, medication codes, investigation codes, and process of care codes. This large primary care database has been demonstrated to be representative of the UK population, although less socioeconomically deprived people are slightly overrepresented [37].
We used a two-step process to identify people with type 2 diabetes, which we have reported in full previously [38]. In brief, the first step identified all people with diabetes (of any type), defined as those who had a diagnostic code (diagnosis of diabetes), clinical investigations (two or more fasted, random, or glucose tolerance test values or HbA1c measurements consistent with diagnosis), or medication use (two or more prescriptions for oral diabetes medications, excluding metformin or injectable therapies). These people were then categorised by diabetes type using a clinically-based seven-step algorithm. This method was chosen to minimise the impact of misdiagnosis, misclassification and miscoding, which has previously been identified in people with diabetes [39, 40]. All adults (age ≥ 18 years) with identified type 2 diabetes were included for analysis.
Within the adult type 2 diabetes population, we identified all new medication prescriptions for metformin, sulfonylureas, dipeptidyl peptidase-4 (DPP-4) inhibitors, thiazolidinediones, sodium-glucose cotransporter 2 (SGLT2) inhibitors, meglitinides, and alpha-glucosidase inhibitors between January 1, 2005 and December 31, 2015. We did not examine persistence with fixed-dose combination therapies. To be included as a new prescription, we required a minimum of 6 months of registration prior to the first prescription occurrence for the medication of interest. People with only one prescription for the medication of interest were excluded from the analysis. We followed persistence for each newly prescribed medication. Non-persistence was defined as a gap in prescriptions of ≥ 90 days. The duration of persistence was defined as the time interval between the first prescription and the last identified prescription consistent with persistence. Only people currently registered with the primary care practice from which their data were extracted were included. People who had died or were unregistered at the time of data collection (January 1, 2016) were not included. People who had a final prescription for the medication within 90 days of the end of follow-up were categorised as having censored persistence and included for analysis. All available data were used to follow-up people with type 2 diabetes either from registration with their current primary care practice, the earliest available records (January 2004), or the diagnosis of type 2 diabetes (whichever was latest).
People were considered to be non-persistent if they switched medication within a class; for example, a change from sitagliptin to linagliptin was considered to be non-persistence with sitagliptin—two persistence events were then included for analysis (one with sitagliptin and one with linagliptin). People who switched medication preparation (for example metformin standard release to metformin modified release) were considered to be persistent. We only consider primary persistence (i.e. persistence from the first recorded prescription of each medication).
Statistical Methods
For each medication class included, we report the proportion of people remaining persistent at 6 months, 1 year, 2 years, and 5 years, with 95% confidence intervals (95% CI). We also report the crude median persistence duration with each class with 95% confidence intervals.
We used Cox regression analysis to identify the independent influences of multiple variables on medication persistence. Factors included in the regression analysis comprised age, gender, ethnicity, socioeconomic status (measured using the Index of Multiple Deprivation; IMD score), smoking status, alcohol intake, duration of diabetes, glycaemic control, presence of complications, presence of comorbidities, number of concurrent diabetes medications, number of previous non-persistent diabetes medications, and medication class. Ethnicity was defined using the Office of National Statistics (ONS) official UK ethnicity categories: this defines five major ethnic categories: white, mixed/multiple ethnic groups, Asian (including Indian, Pakistani, Bangladeshi, and Chinese people), black (including African and Caribbean people), and other (including Arab and other minority groups not classified elsewhere) [41].
Socioeconomic status was derived using the nationally recognised measure IMD, based on patient postcode. Smoking status and alcohol use were defined using the most recently recorded measure. Duration of diabetes was defined as the time between the first recorded indicator of diabetes (diagnostic code, blood glucose measure consistent with diabetes, or medication) in the record and the time of initiation of the medication of interest. In the population characteristics table, the duration of diabetes is defined as the time between the first indicator of diabetes and the date of data extraction (January 1, 2016). Body mass index (BMI) and blood pressure were defined using the value most recently recorded prior to the initiation of the medication of interest. The presence of diabetes complication and comorbidities was determined by the presence of diagnosis codes or other codes specific for the diagnosis (e.g. read code “6A9..” “Atrial fibrillation annual review” as a code to identify the presence of atrial fibrillation). The diabetes complications identified comprised amputation, peripheral neuropathy, retinopathy, and peripheral vascular disease. The comorbidities identified comprised hypertension, atrial fibrillation, angina, stroke, myocardial infarction, congestive cardiac failure, transient ischaemic attack (a history of), coronary artery disease, chronic kidney disease (CKD 3–5), renal replacement therapy (dialysis or transplant), dementia, depression, rheumatoid arthritis, and chronic liver disease (any cause). Chronic kidney disease was identified using estimated glomerular filtration rate (eGFR) measurements and diagnosis codes. Counts of previous and concurrent diabetes medications included fixed-dose combination therapies, which were counted as one additional medication.
All variables included were categorical to account for nonlinear relationships with the outcome measure. Model selection was performed by backwards stepwise elimination of nonsignificant variables (p > 0.05) to minimise the Akaike information criterion (AIC). The outcome event was defined as non-persistence (no repeat prescription collected within 90 days of the previous prescription), with hazard ratios (HR) for non-persistence reported with 95% confidence intervals. Each new medication started was considered a persistence event, so several persistence events were analysed for patients initiated on several medications. We report R2 as a measure of model performance. We used the statistical package R version 3.3.1 for the statistical analysis.
Compliance with Ethics Guidelines
All data used were anonymised at the point of data extraction. No clinically identifiable information was available to researchers. The study was been tested against the Health Research Authority (HRA)/Medical Research Council (MRC) “is this research” tool (http://www.hra-decisiontools.org.uk/research/), and was considered to be an audit of current practice when compared to the best available evidence. The study therefore did not require specific ethical approval. Approval for this work was granted by the RCGP RSC study approval committee prior to initiation.
Results
From a total RCGP RSC cohort of 1,238,909 people from 128 primary care practices, 64,909 (5.2%) people were identified as having diabetes. Of these 60,327 (92.9%) were categorised as type 2 diabetes; a crude prevalence of 6.05% type 2 diabetes in adults. The age-gender direct standardised prevalence for type 2 diabetes in the cohort was 6.25% (95% CI 6.20–6.30%), comparable to the 2011 UK census. In the type 2 diabetes population, the mean age was 66.1 (SD 13.8) years, and 26,792 (41.3%) were female (Table 1).
The median duration of follow-up was 6.6 (IQR 3.17–10.9) years. During the follow-up period, the majority 42,810 (70.9%) of the people had one or more oral medications prescribed. Metformin was the most commonly prescribed medication, followed by sulfonylureas (Table 2).
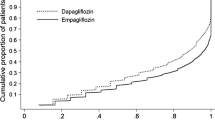
We measured persistence with 55,728 oral medications (Table 2). Non-persistence occurred with 38,169 (68.5%) of those during follow-up. The remaining 17,559 medications had ongoing persistence at the end of follow-up. The median persistence duration overall was 2.25 (95% CI 2.20–2.30) years. Metformin had the longest crude persistence and alpha-glucosidase inhibitors had the shortest, with persistence trends consistent from 6 months to 5 years (Table 3).
In Cox regression analyses (Table 4), factors associated with improved medication persistence were found to include older age, male gender, white ethnicity (Fig. 1), HbA1c 42–60 mmol/mol, presence of hypertension, and no previous glucose-lowering medication use. Factors associated with non-persistence include the presence of neuropathy, a history of myocardial infarction, heart failure, dementia, depression, and chronic liver disease. All medication classes had higher adjusted hazard ratios for non-persistence than for metformin, except for the SGLT2 inhibitors. Variables not associated with persistence (and therefore removed from the model) were smoking status, body mass index (BMI), previous amputations, retinopathy, atrial fibrillation, angina, previous stroke or transient ischaemic attack (TIA), and use of renal replacement therapy.
Discussion
Medication persistence with glucose-lowering agents differs considerably between classes; persistence with metformin was significantly longer than that with any other medication class except for SGLT2 inhibitors (although only a short duration of follow-up was available for this new drug class). Only metformin, sulfonylureas, and SGLT2 inhibitors had more than 50% persistence at 2 years. Alpha-glucosidase inhibitors have the highest rates of non-persistence in clinical practice. Younger people and people of non-white ethnicity had the lowest medication persistence.
The effect size for influence on medication persistence was largest for medication class. This suggests that the class of medication used is the major factor which influences the duration of a selected treatment in type 2 diabetes. Whilst this finding may be unsurprising, it has important implications. Careful selection of second-line therapy after metformin, with a preference for therapies which have longer treatment persistence, may facilitate better long-term diabetes control. However, medication persistence is not uniformly positive. For instance, extended duration of sulphonylureas may not be beneficial as the effects of treatment wane over time when compared to those of an insulin-independent therapy [42, 43]. Similarly, reduced persistence in those with HbA1c less than 42 mmol/mol suggests appropriate discontinuation in those at risk of hypoglycaemia.
Comparison with the Literature
We concurred with previous analyses that demonstrated reduced medication adherence in women [6, 30, 44, 45]. We found that a correlation with reduced duration of mediation persistence remained after adjusting for other factors.
The identified differences in medication persistence between people of different ethnicities should be cause for concern. It has previously been reported that ethnic minorities show reduced medication adherence [44, 46, 47], but no previous study has been able to adjust for socioeconomic status. The finding that these differences are still substantial in a healthcare system free at the point of delivery, and after adjusting for socioeconomic status, is an important finding. This is particularly so, given that a number of the ethnic groups with shorter medication persistences have higher prevalences of diabetes and diabetes-related complications [48]. These observed differences merit further investigation. In particular, possible causes of this disparity should be identified.
Our finding concurred with previous studies which found that the presence of depression and other comorbidities was associated with reduced medication adherence [49,50,51,52]. However, we found that hypertension was associated with slightly longer persistence. Our findings also concurred with others which have demonstrated reduced adherence in younger people with type 2 diabetes [6, 30, 44, 45, 53]. We have extended these previous analyses to demonstrate that the association with persistence is non-linear; there is substantially reduced medication persistence in those under 30 years old when compared to the other age groups. This may represent lifestyle factors or be due to early beta-cell failure and a misdiagnosed autoimmune aetiology (with a need for early escalation of therapy) to type 2 diabetes [54]. These factors which influence medication persistence merit further investigation, and to this end we have initiated a follow-on qualitative analysis of factors influencing medication use in people with type 2 diabetes [Integrated Research Application System (IRAS) application number; 230092].
No direct comparison of medication persistence across all groups of diabetes medications has previously been performed [55]. Our data suggest that medication class is the major influencing factor in medication persistence.
Strengths and Limitations
The large population size, long duration of follow-up and completeness of the patient record are the main strengths of this analysis. In particular, the availability of a recognised measure of socioeconomic status and of previous and concurrent medication numbers add validity to the conclusion that medication class is the major influencing factor in medication persistence.
Non-persistence is defined retrospectively, with a non-persistence event only identified 90 days after the last medication prescription. This may have artificially inflated the apparent persistence for medications that have not been available for a long time period, such as the SGLT2 inhibitors. Re-evaluation of persistence rates with these medications is needed as more data become available. Our inclusion of drug switching within a class as a non-persistence event may mean our data shows lower persistence rates than others that have not included this. In the absence of a formal definition, we have chosen this method to fit best with previous recommendations [34].
We were unable to adjust for some factors which have been shown to be associated with medication adherence or persistence, such as proximity to pharmacy, continuity of care, and level of trust in the healthcare provider [56,57,58]. However, it is unlikely that the inclusion of these factors would substantially alter the associations identified here. Factors underlying the reasons for differences in non-persistence between classes were not explored in this analysis.
Conclusions
Important factors associated with reduced medication persistence are female gender, younger age, and non-white ethnicity. After adjusting for these and other factors, medication persistence varies considerably across different medication classes and within medication classes, with medication class being the most important predictor of persistence. Metformin was associated with significantly longer persistence than all other medication classes except for SGLT2 inhibitors. SGLT2 inhibitors also show early promise for good persistence, although median persistence was not reached by the end of the follow-up in this study because only a short follow-up duration for this class was available.
References
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: WHO; 2003.
Jermendy G, et al. Persistence of initial oral antidiabetic treatment in patients with type 2 diabetes mellitus. Med Sci Monit. 2012;18(2):Cr72–7.
Abegunde DO, et al. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–38.
Trogdon JG, et al. Peer reviewed: costs of chronic diseases at the state level: the chronic disease cost calculator. Prev Chron Dis. 2015;12:150131.
Al-Majed HT, et al. Adherence of type-2 diabetic patients to treatment. Kuwait Med J. 2014;46(3):225–32.
Awodele O, Osuolale JA. Medication adherence in type 2 diabetes patients: study of patients in Alimosho General Hospital, Igando, Lagos, Nigeria. Afr Health Sci. 2015;15(2):513–22.
Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with type 2 diabetes: a retrospective cohort study. Diabet Med. 2002;19(4):279–84.
Peyrot M, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29(5):682–9.
Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–24.
Iglay K, et al. Meta-analysis of studies examining medication adherence, persistence, and discontinuation of oral antihyperglycemic agents in type 2 diabetes. Curr Med Res Opin. 2015;31(7):1283–96.
Aikens JE, Piette JD. Longitudinal association between medication adherence and glycaemic control in type 2 diabetes. Diabet Med. 2013;30(3):338–44.
Buysman EK, et al. Impact of medication adherence and persistence on clinical and economic outcomes in patients with type 2 diabetes treated with liraglutide: a retrospective cohort study. Adv Ther. 2015;32(4):341–55.
Kim N, Agostini JV, Justice AC. Refill adherence to oral hypoglycemic agents and glycemic control in veterans. Ann Pharmacother. 2010;44(5):800–8.
Penning-van Beest FJ, et al. Effect of non-persistent use of oral glucose-lowering drugs on HbA1c goal attainment. Curr Med Res Opin. 2008;24(9):2523–9.
Rozenfeld Y, et al. Oral antidiabetic medication adherence and glycemic control in managed care. Am J Manag Care. 2008;14(2):71–5.
Wu CH, et al. The eight-item Morisky Medication Adherence Scale (MMAS-8) score was associated with glycaemic control in diabetes patients. Hypertension. 2014;64(Suppl 1):A558.
Heaton PC, Tundia NL, Luder HR. US emergency departments visits resulting from poor medication adherence: 2005–07. J Am Pharm Assoc. 2003;53(5):513–9.
Hong JS, Kang HC. Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea. Med Care. 2011;49(4):378–84.
Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27(9):2149–53.
Zhu VJ, et al. Oral hypoglycemic agent adherence and hospitalization among patients with type 2 diabetes: a call for enhanced guidelines. Pharmacoepidemiol Drug Saf. 2012;21(S3):29.
Egede LE, et al. Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care. 2012;35(12):2533–9.
Hansen RA, et al. A retrospective cohort study of economic outcomes and adherence to monotherapy with metformin, pioglitazone, or a sulfonylurea among patients with type 2 diabetes mellitus in the United States from 2003 to 2005. Clin Ther. 2010;32(7):1308–19.
Lee WC, et al. Prevalence and economic consequences of medication adherence in diabetes: a systematic literature review. Manag Care Interface. 2006;19(7):31–41.
Macewan JP, et al. Penny-wise, pound-foolish: association between medication adherence, out-of-pocket expenses, and health care costs in medicare patients with type 2 diabetes. Diabetes. 2015;64(S1):A69.
Nasseh K, et al. Cost of medication nonadherence associated with diabetes, hypertension, and dyslipidemia. Am J Pharm Benefits. 2012;4(2):e41–7.
Shenolikar RA, et al. Comparison of medication adherence and associated health care costs after introduction of pioglitazone treatment in African Americans versus all other races in patients with type 2 diabetes mellitus: a retrospective data analysis. Clin Ther. 2006;28(8):1199–207.
Stuart BC, et al. Increased persistency in medication use by US Medicare beneficiaries with diabetes is associated with lower hospitalization rates and cost savings. Diabetes Care. 2009;32(4):647–9.
Hong S, et al. Compliance with anti-diabetic medication improves cardiovascular outcomes in patients with type 2 diabetes. Diabetes. 2013;62(S1):A372.
Wu C-S. Antihyperglycemic adherence and risk of stroke among type II diabetes mellitus: a population-based retrospective cohort study. Dissertation. University of South Carolina: Columbia; 2012.
Currie CJ, et al. The impact of treatment noncompliance on mortality in people with type 2 diabetes. Diabetes Care. 2012;35(6):1279–84.
Pladevall M, et al. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27(12):2800–5.
Salas M, et al. Costs of medication nonadherence in patients with diabetes mellitus: a systematic review and critical analysis of the literature. Value Health. 2009;12(6):915–22.
Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–37.
Cramer JA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Peterson AM, et al. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10(1):3–12.
Raebel MA, et al. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–21.
Correa A, et al. Royal College of General Practitioners Research and Surveillance Centre (RCGP RSC) sentinel network: a cohort profile. BMJ Open. 2016;6(4):e011092.
McGovern A, et al. Real-world evidence studies into treatment adherence, thresholds for intervention and disparities in treatment in people with type 2 diabetes in the UK. BMJ Open. 2016;6(11):e012801.
de Lusignan S, et al. A method of identifying and correcting miscoding, misclassification and misdiagnosis in diabetes: a pilot and validation study of routinely collected data. Diabet Med. 2010;27(2):203–9.
de Lusignan S, et al. Miscoding, misclassification and misdiagnosis of diabetes in primary care. Diabet Med. 2012;29(2):181–9.
Office for National Statistics. Ethnicity. 2015. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity. Accessed 28 Dec 2017.
Del Prato S, et al. Long-term glycaemic response and tolerability of dapagliflozin versus a sulphonylurea as add-on therapy to metformin in patients with type 2 diabetes: 4-year data. Diabetes Obes Metab. 2015;17(6):581–90.
Matthews DR, et al. UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group. Diabet Med. 1998;15(4):297–303.
Fisher L, et al. Emotional distress is linked to medication adherence in type 2 diabetes. Diabetes. 2009;58:A478.
Bezie Y, et al. Therapeutic compliance: a prospective analysis of various factors involved in the adherence rate in type 2 diabetes. Diabetes Metab. 2006;32(6):611–6.
Egede E, et al. Regional, geographic, and ethnic differences in medication adherence among adults with type 2 diabetes. Ann Pharmacother. 2011;45(2):169–79.
Shenolikar RA, et al. Race and medication adherence in medicaid enrollees with type-2 diabetes. J Natl Med Assoc. 2006;98(7):1071–7.
Oldroyd J, et al. Diabetes and ethnic minorities. Postgrad Med J. 2005;81(958):486–90.
Gonzalez JS, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31(12):2398–404.
Leblond J, et al. Predictors of nonpersistence with thiazolidinediones in patients with type 2 diabetes. Can J Diabetes. 2005;29(2):95–102.
Gwadry-Sridhar F, et al. Influence of previous medication compliance on future compliance in patients with type 2 diabetes. Diabetes. 2010;59:A346.
Toyoda M, et al. Predictors of response to liraglutide in Japanese type 2 diabetes. Diabetes Res Clin Pract. 2014;106(3):451.
Feldman BS, et al. Defining the role of medication adherence in poor glycemic control among a general adult population with diabetes. PLoS One. 2014;9(9):e108145.
Hawa MI, et al. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: action LADA 7. Diabetes Care. 2013;36(4):908–13.
McGovern A, et al. A comparison of adherence and persistence by medication class in type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2017. https://doi.org/10.1111/dom.13160.
Gwadry-Sridhar F, et al. Understanding predictors of compliance in fixed-dose combination vs loose-dose combination therapy for treatment of type 2 diabetes. Diabetes. 2010;59:A346.
Chen CC, Tseng CH, Cheng SH. Continuity of care, medication adherence, and health care outcomes among patients with newly diagnosed type 2 diabetes: a longitudinal analysis. Med Care. 2013;51(3):231–7.
Hessler DM, et al. Low patient trust in their primary care provider predicts medication nonadherence 12 months later. Diabetes. 2014;63:A194.
Acknowledgements
Funding
This study was funded by Eli Lilly and Company. The funders were involved in the study design. Data collection, data analysis, and manuscript preparation were performed independently from the funder. The funder had no influence on the decision to publish but has provided funds to cover the publication cost.
Authorship
The authors from the University of Surrey had full access to all of the data in this study, and all authors take complete responsibility for the integrity of the data and accuracy of the data analysis. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. The authors would like to acknowledge the support of Kate van Brunt and Bradley Curtis from Eli Lilly and Company for assistance in setting up and designing the University of Surrey-Lilly Real World Evidence (RWE) projects. We are also grateful to additional members of the University of Surrey team: Filipa Ferreira (project management), Jeremy van Vlymen (statistical support), Ana Correa, and Rachel Byford (database support and SQL programming).
Disclosures
Andrew McGovern has undertaken research funded by Eli Lilly and Company and AstraZeneca. William Hinton has undertaken research funded by Eli Lilly and Company. Simon de Lusignan has also undertaken research funded by GlaxoSmithKline, AstraZeneca, Eli Lilly and Company, and Takeda. Neil Munro has undertaken research funded by Eli Lilly and Company and has received fees for serving as a speaker, a consultant or an advisory board member for Allergan, Bristol-Myers Squibb, AstraZeneca, GlaxoSmithKline, Eli Lilly and Company, Lifescan, MSD, Metronic, Novartis, Novo Nordisk, Pfizer, Sankio, Sanofi, Roche, Servier, and Takeda. Martin Whyte has undertaken research funded by Eli Lilly and Company and received speaker fees from AstraZeneca. Silvio Calderara is an employee of Eli Lilly and Company.
Compliance with Ethics Guidelines
All data used were anonymised at the point of data extraction. No clinically identifiable information was available to researchers. The study was tested against the Health Research Authority (HRA)/Medical Research Council (MRC) “is this research” tool (http://www.hra-decisiontools.org.uk/research/) and was considered to be an audit of current practice when compared to the best available evidence. The study therefore did not require specific ethical approval. Approval for this work was granted by the RCGP RSC study approval committee prior to initiation.
Data Availability
The datasets obtained during and/or analyzed during the current study are available from the corresponding author on reasonable request and subject to access approval.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/C31DF0607ED36CA2.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McGovern, A., Hinton, W., Calderara, S. et al. A Class Comparison of Medication Persistence in People with Type 2 Diabetes: A Retrospective Observational Study. Diabetes Ther 9, 229–242 (2018). https://doi.org/10.1007/s13300-017-0361-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-017-0361-5