Abstract
Introduction
Hypoglycaemia and hyperglycaemia are common adverse events associated with antidiabetic medications. They are also a common cause of hospital admissions for people with diabetes. The objective of the study was to explore the trends in hospital admissions due to hypoglycaemia and hyperglycaemia and in the prescriptions of antidiabetic medications in England and Wales.
Methods
We conducted an observational study during the period 1999–2016. Hospital admission data for patients from all age groups were extracted from the Hospital Episode Statistics database in England and the Patient Episode Database for Wales. Data on prescriptions of antidiabetic medications were extracted from the Prescription Cost Analysis database from 2004 to 2016.
Results
Between 1999 and 2016, the hospital admission rate increased by 173.0% [from 17.2 (95% CI 16.9–17.6) to 47.1 (95% CI 46.5–47.6) per 100,000 persons] for hypoglycaemia and by 147.0% [from 22.8 (95% CI 22.4–23.2) to 56.3 (95% CI 55.7–56.9) per 100,000 persons] for hyperglycaemia. The prescription rate for all antidiabetic medications increased between 2004 and 2016 by 116.0% [from 373.0 (95% CI 373.0–373.0) to 806.0 (95% CI 806.0–806.0) prescriptions per 1000 persons]. There was a parallel increase in the rate of antidiabetic medication prescriptions during the same study period, with correlation coefficients of 0.94 for hypoglycaemia and 0.98 for hyperglycaemia, respectively.
Conclusions
There have been parallel increases in the rate of admissions due to dysglycaemia and the rate of antidiabetic prescriptions in England and Wales. Further analytical studies are required to investigate whether increased admission for dysglycaemia is associated with increased use of antidiabetic medications.
Similar content being viewed by others
Introduction
In the United Kingdom, there are around 4 million people living with diabetes mellitus, corresponding to an estimated prevalence rate of about 6.2% in 2015 [1]. During the same year, diabetes mellitus accounted for around 23,000 deaths in people aged between 20 and 79 years old [1]. Diabetes mellitus is a chronic condition in which glycaemic control should be managed in order to prevent the development of complications such as microvascular and macrovascular diseases [2]. Antidiabetic therapy, in addition to diet and lifestyle modifications, is an essential component of the management of people with diabetes mellitus with uncontrolled HbA1C levels [3, 4].
Current treatment guidelines recommend the initiation of intensive diabetes therapy in uncontrolled HbA1C patients to achieve better control over their HbA1C levels, since the use of a single antidiabetic agent does not always achieve the targeted glycaemic control [5]. One of the main drawbacks of intensive antidiabetic therapy is the incidence of adverse drug events such as hypoglycaemic events [6]. On the other hand, inappropriate use of antidiabetic therapy is the main leading cause of raised blood glucose levels and the occurrence of hyperglycaemic events [7, 8].
Hospitalisation increased by 11.7% and declined by 38.6% due to hypoglycaemia and hyperglycaemia, respectively, among US Medicare beneficiaries aged 65 years and older between 1999 and 2011 [9]. In England, a previous study showed that hypoglycaemic admissions increased by 14.0% between 2005 and 2014 [10]. However, no study has investigated hospital admissions due to hyperglycaemia in patients aged below 65 years old.
The objective of this ecological study was to explore national trends in hospital admissions due to dysglycaemia among patients from all age groups in England and Wales from 1999 to 2016. Additionally, we examined antidiabetic medication prescriptions for the available period of 2004–2016 to investigate a potential correlation between the trend in admissions due to dysglycaemia and the trend in antidiabetic medication prescriptions.
Methods
Study Sources and the Population
This was a secular trend study using publicly available national data taken from the Hospital Episode Statistics (HES) database in England [11] and the Patient Episode Database for Wales (PEDW) for the period between April 1999 and March 2016 [12]. The HES and PEDW databases contain hospital admission data for hypoglycaemia and hyperglycaemia in patients from all age groups that were subdivided into four categories; below 15 years, 15–59 years, 60–74 years, and 75 years and above. Hospital admissions were identified using the diagnostic codes E16.0, E16.1, E16.2, and T38.3 for hypoglycaemia admissions and E10.1, E11.1, E12.1, E13.1, E14.1, and R73.9 for hyperglycaemia admissions from the 10th version of the International Statistical Classification of Diseases (ICD) system. Admission codes for hypoglycaemia and hyperglycaemia were consistent with those used in previous studies [9, 10, 13]. Hyperglycaemia admission codes were selected and included based on the clinical fact that ketoacidosis, if presented in patients with diabetes mellitus, is considered a sign of hyperglycaemia, where the body is unable to produce enough insulin in response to raised blood glucose levels [14]. In addition, the diagnostic code (R73.9) was selected based on its description, which stands for unspecified hyperglycaemia.
HES and PEDW are the main healthcare databases in England and Wales. They record all hospital admissions, outpatients and Accident and Emergency (A&E) activities performed at all National Health Service (NHS) trusts and any independent sector funded by NHS trusts. Data for hospital admissions in England and Wales are available from the years 1999/2000 onwards. Available data include patient demographics, clinical diagnoses, procedures, and durations of stay. HES and PEDW data are checked regularly to ensure their validity and accuracy [11, 15].
Mid-year population data for the period between 1999 and 2016 were collected from the Office for National Statistics (ONS) to calculate the admission rate on a yearly basis [16].
Antidiabetic medication prescription data in England and Wales were extracted from the Prescription Cost Analysis (PCA) database for the available period of April 2004–March 2016 [17, 18]. The PCA database provides information about all items that are prescribed by general practitioners and other healthcare professionals, such as hospital physicians, pharmacists and nurses, and dispensed in the community, whether by dispensing physicians, pharmacy contractors or appliance contractors in England and Wales [19,20,21]. The British National Formulary (BNF) therapeutic classification system is used to report the data to the PCA database. Prescription data became available in England from 2004 [17] and in Wales from 2000 [18]. Only prescriptions dispensed in the community in England and Wales and submitted to NHS Prescription Services are reported in the PCA database [19]. The accuracy of the prescriptions recorded in the PCA database was estimated by NHS Prescription Services to reach 98.5% for patients in England and 99.2% for patients in Wales [19, 22].
Compliance with Ethics Guidelines
This study was based on publicly available data and did not involve any new studies of human or animal subjects performed by any of the authors.
Statistical Analysis
Hospital admission rates with their 95% confidence intervals (CIs) were calculated using the number of hypoglycaemia/hyperglycaemia admissions for each age group divided by the mid-year population of the same age group of the same year. Antidiabetic prescription rates were calculated using the number of antidiabetic prescriptions divided by the total mid-year population during the same year.
The chi-squared test was used to assess the difference between the admission rates in 1999 and 2016 and the difference between the antidiabetic medication prescription rates in 2004 and 2016. The trend in hospital admissions for hypoglycaemia and hyperglycaemia was assessed using a Poisson model. The correlation between hospital admissions for hypoglycaemia/hyperglycaemia and antidiabetic prescriptions was assessed using the Pearson correlation coefficient. All analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA).
Results
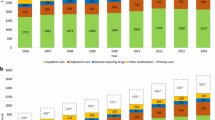
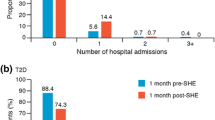
The annual number of hospital admissions for hypoglycaemia rose from 8985 in 1999 to 27,485 in 2016, representing an increase of 173.0% [from 17.2 (95% CI 16.9–17.6) per 100,000 persons in 1999 to 47.1 (95% CI 46.5–47.6) in 2016, trend test, p < 0.01]. The rate of hospital admissions due to hyperglycaemia over the same period increased by 147.0% [from 22.8 (95% CI 22.4–23.2) to 56.3 (95% CI 55.7–56.9) per 100,000 persons] (Fig. 1a), with 11,904 admissions in 1999 and 32,867 admissions in 2016. There were no significant differences in hypoglycaemia and hyperglycaemia admission rates between men and women (p > 0.05).
Hospital admission rates due to dysglycaemia in England and Wales between 1999 and 2016. a Hypoglycaemia and hyperglycaemia admission rates in England and Wales for the total population. b Rates of hospital admissions due to hypoglycaemia across different age groups. c Rates of hospital admissions due to hyperglycaemia across different age groups
The increases in the rates of admissions due to hypoglycaemia and hyperglycaemia were synchronised with an increase in the rate of antidiabetic medication prescriptions from all therapeutic classifications; the correlation coefficients were 0.94 and 0.98, respectively (Fig. 2).
The hospital admission rate due to hypoglycaemia and the rates of insulin and sulfonylurea prescriptions all increased in parallel, with a correlation coefficient of 0.96 obtained for both insulin and sulfonylurea. The correlation coefficients for hypoglycaemia and biguanides or other antidiabetics were 0.94 and 0.85, respectively. The increase in the rate of admissions due to hyperglycaemia was synchronised with the increase in the rates of antidiabetic medication prescriptions from all therapeutic classifications. The correlation coefficients were 0.99, 0.94, 0.98 and 0.95 for insulin, sulfonylurea, biguanides and other antidiabetics, respectively.
In 2015/2016, unspecified hypoglycaemia was the main cause of hypoglycaemic admissions, contributing 78.0% of the total number of admissions due to hypoglycaemia (Table 1). Ketoacidosis in patients with insulin-dependent diabetes mellitus was the main reason for hospital admission due to hyperglycaemia, contributing 73.4%. These proportions were similar to the proportions of the whole period of the study at which unspecified hypoglycaemia and ketoacidosis among patients with insulin-dependent diabetes mellitus were the key reasons for dysglycaemia admissions, contributing to 80.0% and 72.7% of those admissions, respectively, for the period between 1999 and 2016.
Antidiabetic Medication Prescriptions
The total number of antidiabetic prescriptions dispensed annually in England and Wales increased from 19.8 million in 2004 to 47.0 million prescriptions in 2016. Prescription rates for all antidiabetic medications between 2004 and 2016 increased by 116.0% [from 373.0 (95% CI 373.0–373.0) to 806.0 (95% CI 806.0–806.0) prescriptions per 1000 persons].
Antidiabetic prescription rates of sulfonylurea, insulin, biguanide and other antidiabetic medications increased by 41.6% [from 109.0 (95% CI 109.0–109.0) to 154.0 (95% CI 154.0–154.0) prescriptions per 1000 persons], 51.5% [from 84.8 (95% CI 84.7–84.9) to 129.0 (95% CI 128.0–129.0) prescriptions per 1000 persons], 152.0% [from 150.0 (95% CI 150.0–150.0) to 378.0 (95% CI 377.0–378.0) prescriptions per 1000 persons] and 399.0% [from 29.1 (95% CI 29.1–29.2) to 145.0 (95% CI 145.0–145.0) prescriptions per 1000 persons], (Fig. 2).
Hypoglycaemia Hospital Admissions by Age Group
Hospital admissions due to hypoglycaemia were found to be directly related to age. Admission rates for patients aged 75 years and above were higher than those aged 60–74 years, followed by patients aged 15–59 years and below 15 years (Fig. 1b). Between 1999 and 2016, hospital admission rates increased for all age groups. The highest increase in admission rate was in the age group 75 years and above, which increased by 267.0% [from 63.9 (95% CI 61.4–66.4) to 234.0 (95% CI 230.0–239.0) per 100,000 persons], followed by the age group 15–59 years, which increased by 126.0% [from 10.4 (95% CI 10.0–10.7) to 23.3 (95% CI 22.8–23.9) per 100,000 persons], and then the age group below 15 years, which increased by 124.0% [from 12.4 (95% CI 11.7–13.1) to 27.7 (95% CI 26.7–28.7) per 100,000 persons], and the age group 60–74 years, which increased by 112.0% [from 29.0 (95% CI 27.7–30.2) to 61.3 (95% CI 59.7–63.0) per 100,000 persons].
The rates of hypoglycaemia admission in 2015/2016 for patients aged 75 years and above were 3-fold, 10-fold and 8-fold higher than the rates among patients aged 60–74 years, 15–59 years and below 15 years, respectively.
Hyperglycaemia Hospital Admissions by Age Group
Hospital admissions due to hyperglycaemia were found to be higher in those aged 15–59 years and 75 years and above, followed by patients aged 60–74 years and those below 15 years (Fig. 1c). Between 1999 and 2016, hospital admission rates increased markedly—by 198.0% [from 25.7 (95% CI 24.1–27.3) to 76.5 (95% CI 74.1–79.0) per 100,000 persons]—in those aged 75 years and above, followed by 170.0% [from 25.2 (95% CI 24.7–25.8) to 68.2 (95% CI 67.3–69.1) per 100,000 persons] in the 15–59 years group, then by 119.0% [from 18.7 (95% CI 17.7–19.7) to 40.9 (95% CI 39.6–42.2) per 100,000 persons] in the 60–74 years group, and by 24.6% [from 17.0 (95% CI 16.2–17.8) to 21.2 (95% CI 20.3–22.1) per 100,000 persons] in the age group below 15 years.
Compared with patients aged 60–74 years, 15–59 years and below 15 years, the rate of hyperglycaemia admission in patients aged 75 years and above in 2015/2016 was approximately double, the same, and quadruple, respectively.
Discussion
Our study found a significant increase in the rate of hospital admissions due to hypoglycaemia and hyperglycaemia in England and Wales, with an average increase of 10.2% and 9.2%, respectively, per year during the past 17 years. This increase was accompanied by a rise in the rate of antidiabetic medication prescriptions from all therapeutic classifications during the past 13 years.
The average annual increase in the prevalence rate of diabetes mellitus in England in the past 10 years is estimated to be 7.7% [23] and 4.0% in Wales [24]. Prevalence data in England and Wales are restricted only for patients aged 17 years and above, and are estimated based on the percentage of diabetes mellitus patients registered in the total practice list [23, 24]. The increase in antidiabetic prescriptions may reflect an increase in the prevalence of diabetes itself or an intensification of treatment in people with diabetes. Based on the available prevalence data, we assume that the average yearly increase in the rate of dysglycaemia admissions and the rate of antidiabetic medication prescriptions was higher than the average increase in the prevalence of diabetes mellitus. Based on this, we hypothesise that intensive antidiabetic therapy using multiple antidiabetic medications has played a role in increasing the rate of dysglycaemia admissions in the past few years (i.e. hypo may be associated with aggressive treatment and hyper could be the result of uncontrolled diabetes due to nonadherence). This hypothesis was tested by a study conducted in the USA, which found that patients who were exposed to intensive therapy were at higher risk of hypoglycaemia admission [25]. Furthermore, it was found that the higher the number of medications being used, the more likely it is that the patient will be nonadherent, which diminishes the benefit of therapy and increases the risk of harm [26].
We are unable to make a direct comparison with previous studies as they used different ICD codes. The rate of dysglycaemia admissions in our study was higher than in previous studies [9, 10, 27]. There are several possible explanations for this. First, the study design itself: as this study is an ecological study monitoring trends in dysglycaemia admission at the population level without access to patient-level data, we cannot be certain that all of these admissions are for patients with diabetes mellitus. Second, different ICD codes were used in the identification of hypoglycaemia admission. This study included ICD code T38.3 [poisoning: insulin and oral hypoglycaemic (antidiabetic) drugs], which contributed 11.1% of the hypoglycaemia admissions. As investigated in a previous study on hyperglycaemia admissions, we used the ICD code E10.1 [9], in addition to four other ICD codes (E11.1, E12.1, E13.1 and E14.1) that are based on the presence of ketoacidosis, as well as the ICD code R73.9, which is used for unspecified hyperglycaemia. These additional five ICD codes contributed around 27.2% of the hyperglycaemia admissions. Third, different age groups were investigated. Fourth, different study periods were examined. Finally, different populations were used to calculate dysglycaemia admission rates.
Hypoglycaemia-Related Hospital Admissions
The increase in admissions due to hypoglycaemia in England and Wales found in our study is higher than what has been reported previously in the USA (11.7%) [9] and in England (14.0%) [10]. Those studies reported that admissions increased by 1.0% and 1.4% per year, respectively. However, a study in Canada reported that the hypoglycaemia admission rate decreased by 50.0% over a period of 12 years between 2002 and 2013, at an average of 4.2% per year [27].
Our study confirmed that there is a difference between the hypoglycaemia admission rates for patients from different age groups. Patients aged 60 years and older are at higher risk of hypoglycaemia-related admission than younger patients, which is consistent with previous studies [9, 10, 28]. Hypoglycaemia in older people could be influenced by several factors, such as susceptibility to hypoglycaemia and other adverse events, cognitive dysfunction, disease comorbidities, and the use of multiple medications [29]. In addition, more aggressive antidiabetic treatment of patients could potentially explain the increasing rate of hypoglycaemia over the last 17 years.
The factors that contribute to hypoglycaemia differ between patients aged 15 years and below and older patients. Children have a higher possibility of developing 2–5 (or even more) mild hypoglycaemic events per week, and are also at high risk of severe events [30]. Furthermore, a previous study has reported that the presence of other comorbidities (for example, gastroenteritis) in children is associated with hypoglycaemia events [31]. While we do not have data on the prescribing of insulin in children, it is reasonable to assume that the increased rate of hypoglycaemia admissions may be attributable to the use of insulin for the treatment of type I diabetes mellitus (T1DM) in children.
Hyperglycaemia-Related Hospital Admissions
The increase in admissions due to hyperglycaemia in England and Wales is higher than and opposite to what was observed in the USA, where there was a decrease of 38.6% between 1999 and 2011, representing an average 3.2% decline per year [9].
In line with the USA-based study [9], our study found that patients aged 75 years and above were at particularly high risk of admission due to hyperglycaemia. We also found that young patients aged 15–59 years were at higher risk of hospital admission due to hyperglycaemia than other age groups. No previous study has reported hyperglycaemia in this young age group of patients.
In 2015/2016, our study found that 73.4% of hyperglycaemia admissions were coded “insulin-dependent diabetes mellitus—with ketoacidosis”, highlighting that hyperglycaemia admission is prevalent among uncontrolled HbA1C patients treated with insulin. This could explain the reason for the higher rate of hyperglycaemia admissions in the group aged 15–59 years, since T1DM is common among young adults aged 40 years and below [32]. Furthermore, for patients aged 75 years and above, the raised rate of hyperglycaemia admissions could be due to uncontrolled diabetes and the use of insulin therapy to achieve a better control over the disease.
Several factors could potentially stimulate uncontrolled hyperglycaemia, such as a sedentary lifestyle, an unhealthy diet, inappropriate use of oral antidiabetic medications and insulins, and inappropriate administration of insulins [33]. Adherence to antidiabetic therapy and infections are also considered important factors that are linked with the incidence of hyperglycaemic episodes [6]. Medication adherence among people with diabetes is influenced by age, complexity of treatment and use of polypharmacy [7]. Poor adherence to antidiabetic therapy consisting of multiple antidiabetic medications could explain raised blood glucose levels and therefore poor disease control. Additionally, patient behaviour towards and perceptions of their medications have been linked to adherence and can contribute to increased admissions related to hyperglycaemia among patients aged 15–59 years. It has been observed that younger patients may feel that they have other priorities and are able to manage their disease without adhering to physician directions regarding their medication regimen [34]. Furthermore, antidiabetic medication adverse events and (especially) hypoglycaemia are important issues related to nonadherence to therapy [35], and consequently increase the incidence of hyperglycaemic events. Based on the evidence, we suggest that elderly patients aged 75 years and above may experience hyperglycaemic events due to fear of hypoglycaemic events.
Trends in Dysglycaemia Admissions and Antidiabetic Medication Prescriptions
We found a simultaneous increase in the rate of admissions due to dysglycaemia and the prescription rates of all antidiabetic medications from all therapeutic classifications with correlation coefficients ranging from 0.94 to 0.99, reflecting a strong positive linear relationship.
Our research has generated an important safety signal on the potential inappropriate use of antidiabetic medications among patients with diabetes mellitus. This signal urgently requires investigation. Future analytical studies should be conducted to investigate whether intensifying antidiabetic treatment using multiple antidiabetic medications or by increasing the dose is associated with hypoglycaemia, and whether uncontrolled blood glucose is associated with intensive antidiabetic treatment. Earlier studies have shown that insulin therapy and insulin secretagogues are high-risk medications that are most frequently associated with hypoglycaemic events [6, 36]. Based on current evidence, healthcare professionals should be aware of the risk of dysglycaemia that is associated with the use of antidiabetic medications. Furthermore, educating children with diabetes and their parent/caregiver on the appropriate insulin management and administration is a vital part of diabetes management [37].
Strengths and Limitations
The study was a population study at the national level. However, it was an ecological study and therefore we were unable to access data on patient level to confirm that these hypoglycaemia and hyperglycaemia admissions were of patients with diabetes mellitus. Furthermore, we were unable to identify other risk factors such as the presence of comorbidities, the presence of polypharmacy or other factors associated with hypoglycaemia and hyperglycaemia without patient level data. Other limitations include a lack of information on gender at age group level, rural/urban residence and ethnicity for dysglycaemia admission or antidiabetic medication prescription data.
Conclusions
This study suggests that there are parallel increases in the rate of hospital admissions due to dysglycaemia and the rate of antidiabetic prescriptions in England and Wales over the past 13 years. Further studies should be conducted at the patient level to investigate the association between the use of multiple antidiabetic medications and the risk of hypoglycaemic and hyperglycaemic events.
Change history
04 January 2018
In the original publication, the fifth author’s name was incorrectly published as Simon J. Bell. The correct name should read as ‘J. Simon Bell’.
References
International Diabetes Federation. IDF diabetes atlas. 7th ed. Brussels: International Diabetes Federation; 2015. p. 16–64.
Hanssen KF. Blood glucose control and microvascular and macrovascular complications in diabetes. Diabetes. 1997;46(2):S101–3.
National Institute for Health and Care Excellence. Managing blood glucose in adults with type 2 diabetes. https://pathways.nice.org.uk/pathways/type-2-diabetes-in-adults. Accessed 24 Aug 2017.
National Institute for Health and Care Excellence. Type 1 diabetes in adults: diagnosis and management. https://www.nice.org.uk/guidance/ng17. Accessed 24 Aug 2017.
Riedel A, et al. Loss of glycemic control in patients with type 2 diabetes mellitus who were receiving initial metformin, sulfonylurea, or thiazolidinedione monotherapy. Pharmacotherapy. 2007;27(8):1102–10.
Umpierrez G, Korytkowski M. Diabetic emergencies—ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12(4):222–32.
Garcia-Perez LE, et al. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4(2):175–94.
Mayoclinic. Hyperglycemia in diabetes: causes. http://www.mayoclinic.org/diseases-conditions/hyperglycemia/basics/causes/con-20034795. Accessed 24 Aug 2017.
Lipska KJ, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116–24.
Zaccardi F, et al. Trends in hospital admissions for hypoglycaemia in England: a retrospective, observational study. Lancet Diabetes Endocrinol. 2016;4(8):677–85.
Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics. http://content.digital.nhs.uk/hes. Accessed 24 Aug 2017.
NHS Wales Informatics Service. Annual PEDW Data Tables. http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869. Accessed 24 Aug 2017.
Gomez-Huelgas R, et al. The frequency and impact of hypoglycemia among hospitalized patients with diabetes: a population-based study. J Diabetes Complicat. 2015;29(8):1050–5.
American Diabetes Association. DKA (ketoacidosis) & ketones. http://www.diabetes.org/living-withdiabetes/complications/ketoacidosis-dka.html. Accessed 24 Aug 2017.
NHS Wales Informatics Service. Data quality status report: admitted patient care data set. http://www.infoandstats.wales.nhs.uk/Documents/869/APC%20DQ%20Status%20Report%202015-16-v1.pdf. Accessed 24 Aug 2016.
Office for National Statistics (ONS) Population estimates. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland. Accessed 24 Aug 2017.
National Health Service. Prescription Cost Analysis England 2016. https://digital.nhs.uk/search?q=%22Prescription+Cost+Analysis+(PCA)+provides+details+of+the+number+of+items+and+the+net+ingredient+cost+%22&s=r. Accessed 24 Aug 2017.
Welsh Government. Prescriptions dispensed in the community. http://gov.wales/statistics-and-research/prescriptions-dispensed-community/?lang=en. Accessed 24 Aug 2017.
Welsh Government. Prescribing statistics quality report 2012. p. 1–9. http://gov.wales/docs/statistics/2012/120216prescribingqualityen.pdf. Accessed 24 Aug 2017.
National Health Service. Prescription Cost Analysis (PCA) data. http://www.nhsbsa.nhs.uk/PrescriptionServices/3494.aspx. Accessed 24 Aug 2017.
Primary Care Service. Explanatory notes for the Prescription Cost Analysis. http://www.primarycareservices.wales.nhs.uk/prescription-cost-analysis. Accessed 24 Aug 2017.
Health and Social Care Information Centre (HSCIC). Prescription Cost Analysis England: 2015 data quality. Leeds: HSCIC; 2016. p. 1–2.
National Health Service. Quality and Outcomes Framework 2016. http://content.digital.nhs.uk/qof. Accessed 24 Aug 2017.
Welsh Government. General medical services contract: Quality and Outcomes Framework. http://gov.wales/statistics-and-research/general-medical-services-contract/?tab=previous&lang=en. Accessed 24 Aug 2017.
McCoy RG, et al. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med. 2016;176(7):969–78.
Lipska KJ, et al. Polypharmacy in the aging patient: a review of glycemic control in older adults with type 2 diabetes. JAMA. 2016;315(10):1034–45.
Clemens KK, et al. Trends in antihyperglycemic medication prescriptions and hypoglycemia in older adults: 2002–2013. PLoS One. 2015;10(9):1–13.
Zammitt NN, Frier BM. Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care. 2005;28(12):2948–61.
Kirkman MS, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650–64.
Sunehag A, Haymond MW. Causes of hypoglycemia in infants and children. https://www.uptodate.com/contents/causes-of-hypoglycemia-in-infants-and-children?source=search_result&search=causes-of-hypoglycemia-in-infants-andchildren%3Fsource%3Dsee_link&selectedTitle=2~150. Accessed 24 Aug 2017.
Reid SR, Losek JD. Hypoglycemia complicating dehydration in children with acute gastroenteritis. J Emerg Med. 2005;29(2):141–5.
Norman J. Type 1 diabetes: symptoms, diagnosis, and treatments of type 1 diabetes. https://www.endocrineweb.com/conditions/type-1-diabetes/type-1-diabetes. Accessed 24 Aug 2017.
National Health Service. Hyperglycaemia (high blood sugar). http://www.nhs.uk/conditions/Hyperglycaemia/Pages/Introduction.aspx. Accessed 24 Aug 2017.
Jin J, et al. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–86.
Walz L, et al. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Prefer Adherence. 2014;8:593–601.
Diabetes Teaching Center at the University of California. Insulin releasing pills (secretagogues). http://dtc.ucsf.edu/types-of-diabetes/type2/treatment-of-type-2-diabetes/medications-and-therapies/type-2-non-insulin-therapies/insulin-releasing-pills-secretagogues/. Accessed 24 Aug 2017.
Crawford E. Recommendations for management of diabetes for children in school. Burlington: Vermont Department of Health Diabetes Control Program. p. 1–43.
Acknowledgements
No funding or sponsorship was received for this study or the publication of this article. The article processing charges were funded by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval of the version to be published.
Disclosures
Abdallah Y. Naser, Qian Wang, Lisa Y. L. Wong, Jenni Ilomaki, J. Simon Bell, Gang Fang, Ian C. K. Wong and Li Wei have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
The datasets obtained and/or analysed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised: The fifth author’s name was incorrectly published as Simon J. Bell. The correct name should read as ‘J. Simon Bell’.
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/E9FCF0602042168F.
A correction to this article is available online at https://doi.org/10.1007/s13300-017-0363-3.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Naser, A.Y., Wang, Q., Wong, L.Y.L. et al. Hospital Admissions due to Dysglycaemia and Prescriptions of Antidiabetic Medications in England and Wales: An Ecological Study. Diabetes Ther 9, 153–163 (2018). https://doi.org/10.1007/s13300-017-0349-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-017-0349-1