Abstract
Introduction
In Sweden an estimated 10,000 people with type 1 diabetes use continuous subcutaneous insulin infusion (CSII). Sensor-augmented pump therapy (SAP) is associated with higher acquisition costs but provides additional clinical benefits (e.g. reduced rate of hypoglycemic events) over and above that of CSII alone. The aim of the analysis was to assess the cost-effectiveness of SAP with automated insulin suspension relative to CSII alone in two different groups of patients with type 1 diabetes in Sweden.
Methods
Cost-effectiveness analyses were performed using the QuintilesIMS CORE Diabetes Model, with clinical and economic input data derived from published literature. Separate analyses were performed for patients at increased risk of hypoglycemia and for patients with uncontrolled glycated hemoglobin (HbA1c) at baseline. Analyses were performed from a societal perspective over a lifetime time horizon. Future costs and clinical outcomes were discounted at 3% per annum.
Results
SAP with automated insulin suspension was associated with an incremental gain in quality-adjusted life expectancy versus the CSII of 1.88 quality-adjusted life years (QALYs) in patients at high risk of hypoglycemia and of 1.07 QALYs in patients with uncontrolled HbA1c at baseline. Higher lifetime costs for SAP with automated insulin suspension resulted in projected incremental cost-effectiveness ratios for the SAP with automated insulin suspension versus CSII of Swedish Krona (SEK) 139,795 [euros (EUR) 14,648] per QALY gained for patients at increased risk for hypoglycemia and SEK 251,896 (EUR 26,395) per QALY gained for patients with uncontrolled HbA1c. In both groups, SAP with automated insulin suspension also reduced the incidence of diabetes-related complications relative to CSII.
Conclusions
In Sweden, SAP with automated insulin suspension likely represents a cost-effective treatment option relative to CSII for the management of patients with type 1 diabetes with a history of severe hypoglycemic events or patients who struggle to achieve good glycemic control despite the use of CSII.
Funding
Medtronic International Trading Sàrl.
Similar content being viewed by others
Introduction
Data from the Swedish National Diabetes Register (NDR) indicate that in Sweden in 2013, there were approximately 36,000 people with type 1 diabetes being treated in specialist clinics [1], of whom an estimated 21% were using insulin pumps [continuous subcutaneous insulin infusion (CSII)]. Notably, the proportion of adults using CSII was reported to vary considerably with age, with CSII use being more common in younger and in female patients [1].
CSII represents an important treatment option for type 1 diabetes patients and is a particularly valuable alternative for several subgroups of patients, including those who cannot achieve good glycemic control with multiple daily injections (MDI) of insulin, patients with frequent or severe hypoglycemic events and young children with a fear of needles. There are also several other potential reasons why CSII may be preferable, such as erratic lifestyles with irregular shiftwork or travel across time zones that may complicate disease management. Indeed, in a study of routine clinical practice by Jendle et al. the most common indications for CSII were glucose excursions (35.8%), elevated glycated hemogloblin (HbA1c; 33.0%), patient preference (11.5%), frequent hypoglycemic events (7.9%) and facilitation of glycemic control (6.4%) [2]. Many patients may also prefer CSII to MDI, with patient satisfaction having been reported to be significantly higher in patients using CSII than in those receiving MDI [3].
In terms of clinical benefits, CSII has been shown to improve glycemic control and reduce the incidence of severe hypoglycemic events relative to MDI, particularly in patients with very poor baseline glycemic control [4,5,6,7]. Data from the Swedish NDR has also shown that CSII is associated with a significantly lower hazard ratio for fatal coronary heart disease, fatal cardiovascular disease and all-cause mortality relative to MDI [8].
Sensor-augmented pump therapy (SAP) combines real time continuous glucose monitoring (CGM) with CSII and provides additional benefits beyond those provided by CSII alone. Studies conducted to date have shown that SAP is associated with improved glycemic control and a reduced frequency of hypoglycemic events compared with CSII [9,10,11]. Moreover, SAP-related technology is continually evolving, and SAP with automated insulin suspension includes devices incorporating features such as low glucose suspend (LGS) or predictive low glucose suspend (SmartGuard™ technology), both of which are features designed to minimize the risk of hypoglycemia. With the LGS feature, insulin delivery is temporarily suspended if glucose levels drop below a pre-defined threshold level. Predictive low glucose suspend is the most recently introduced feature and a more sophisticated feature, whereby insulin delivery can be suspended based on the prediction of low glucose levels within the next 30 min and insulin delivery is automatically resumed once blood glucose levels start to recover [12]. Recently published findings from the ASPIRE study report that SAP with LGS, compared with no LGS, was associated with a reduction in both the rate and severity of hypoglycemia, particularly nocturnal hypoglycemic events [13,14,15].
One of the main barriers to wider uptake of SAP is the higher device costs relative to CSII. Therefore, the additional clinical benefit must be weighed against the increased acquisition costs. There is a widespread acceptance that technologies including CSII, CGM and SAP improve patient outcomes; indeed the American Association of Clinical Endocrinologists consensus statement on CGM states that “expanding CGM coverage and utilization is likely to improve the health outcomes of people with diabetes” (page 1009) [16]. CSII with CGM was also recommended in the Endocrine Society Clinical Practice guidelines for type 1 diabetes patients failing to achieve HbA1c targets as well as for well-controlled patients willing to use CGM on an almost daily basis [17]. Long-term health economic analyses are required to assist policy-makers and payers in the decision-making process with regard to the uptake and reimbursement of technologies such as SAP. The aim of the current analysis was to assess the cost-effectiveness of the latest generation of SAP with automated insulin suspension (MiniMed™ 640G insulin pump; Medtronic International Trading Sarl, Tolochenaz, Switzerland) versus CSII alone in two different populations of type 1 diabetes patients in Sweden.
Methods
Model Description
Cost-effectiveness analysis was performed using the QuintilesIMS CORE Diabetes Model (referred to hereafter in text as CDM; QuintilesIMS, Basel, Switzerland). The CDM is a non-product-specific policy analysis tool for cost-effectiveness analysis in type 1 or type 2 diabetes. Details of the model structure and validation have been published elsewhere [18,19,20]. The CDM is based on a series of inter-dependent sub-models that simulate disease progression and the incidence of diabetes-related complications. The sub-models have a semi-Markov structure and use time, time-in-state and diabetes type-dependent probabilities derived from published sources to simulate disease progression. Monte Carlo simulation using tracker variables is used to overcome the memory-less properties of a standard Markov model and allows for interconnectivity and interaction between individual sub-models.
Simulation Cohorts and Treatment Effects
Analyses were performed in two different patient populations. The first patient cohort consisted of patients with type 1 diabetes who were considered to be at increased risk for hypoglycemic events, with patient cohort data, including age, duration of diabetes and baseline HbA1c, taken from a randomized controlled trial conducted by Ly et al. [21], which was a 6-month trial that compared the use of SAP versus CSII in 95 patients with type 1 diabetes in Australia (Table 1). The hypoglycemic event rates included in the analysis were also sourced from the Ly et al. study [21]; after 6 months the rate of severe hypoglycemic events was 2.2 per 100 patient-months for CSII versus 0 per 100 patient-months for SAP.
The second patient cohort consisted of patients with type 1 diabetes with uncontrolled HbA1c at baseline. For this patient population, cohort characteristics were sourced primarily from the Swedish NDR (NDR data on file; Table 1) and supplemented with data from the Diabetes Control and Complications Trial (DCCT) for any missing parameters [22]. Treatment effects for this patient group in terms of change in HbA1c reduction were −0.58% for the SAP with automated insulin suspension group and −0.14% for the CSII group; these were derived from formulae published by Pickup et al. [23]. For this analysis, severe hypoglycemic event rates were assumed to be equal in both treatment arms (a rate of 2.6 severe hypoglycemic events per 100 patient-months was assumed, based on data from Pickup et al. [23]). In both analyses a sensor use of 49 sensors per year (corresponding to 80% of the time) was assumed for the SAP with automated insulin suspension arm (based on the assumption of each sensor lasting 6 days and patients using CGM for an average of 5.64 days per week) [21].
This analysis does not contain data from any new studies with human or animal subjects performed by any of the authors and therefore did not require Institutional Review Board approval.
Intervention and Complication Costs
With regard to treatment cost, only the incremental cost of SAP with automated insulin suspension relative to CSII was included in the analysis. This included the cost (list price) for the sensor, assuming a usage of 49 sensors per year, corresponding to 80% usage, inserter, batteries and transmitter. Costs of self-monitoring of blood glucose (SMBG) strips and lancets were also included. In both analyses an SMBG use of 7.11 strips/day was assumed for the CSII group and 4.35 strips/day for the SAP with automated insulin suspension group, based on findings of an observational analysis conducted in Sweden [24]. The total incremental treatment cost for SAP with automated insulin suspension versus CSII was SEK (Swedish Krona) 24,174.69 per year.
Costs of diabetes-related complications were sourced from published literature and, where necessary, inflated to 2015 SEK (Table 2). Indirect costs were calculated using the human capital approach [25].
Utility Values
Utilities/disutilities for diabetes-related complications were sourced from Beaudet et al. [26]. For the cohort at increased risk of hypoglycemia a utility adjustment was made that combined fear of hypoglycemia (FoH) with the reduction in hypoglycemic event rate, based on rates reported by Ly et al. [21] and on published findings on the impact of SAP on health-related quality of life by McBride et al. [27]. A utility decrement of −0.035 was applied to the CSII arm and a utility benefit of 0.038 was applied to the SAP with automated insulin suspension arm; no specific disutilities for individual severe hypoglycemic events were applied.
A utility benefit associated with reduced FoH was also applied to the SAP with automated insulin suspension arm of the cohort with uncontrolled HbA1c at baseline. A utility benefit of 0.0552 was applied, which was based on the findings of the INTERPRET study. Here, SAP was associated with a decrease in FoH; patients using SAP had a mean decrease of 6.9 units in the Hypoglycemia Fear Survey (HFS) [28, 29]. Currie et al. [30] had reported earlier that a 1 unit increase in the HFS corresponds to a 0.008 increase in the EQ-5D health status questionnaire (EuroQoL-5 dimensions); therefore, a 6.9 unit reduction in HFS corresponds to a utility benefit of 0.0552.
Perspective, Time Horizon and Discounting
The base case analysis was performed from the societal perspective (incorporating indirect costs and lost productivity) in line with recommendations for the Swedish setting. For indirect costs, an average of 233 working days per year, age at first income of 24 years and retirement age of 65 years were assumed. An average salary of SEK 403,200 per year for males and SEK 350,400 per year for females was assumed based on data from Statistics Sweden [31]. The number of days off work for diabetes-related complications were sourced from a study by Sørensen et al. conducted in Denmark [32]. The analysis was performed over a lifetime time horizon, and future costs and clinical outcomes were discounted at a rate of 3% per annum in line with Swedish recommendations [33].
Sensitivity Analyses
To establish the principal drivers of cost-effectiveness outcomes we performed a series of one-way sensitivity analyses. For the cohort at increased risk for hypoglycemia sensitivity analyses were performed in which the utility benefit for reduced FoH was negated, and an analysis in which the benefit was reduced to 0.0184, based on a 2.3 unit reduction in FoH reported by Yeh et al. [34]. Also for the cohort at increased risk for hypoglycemia, sensitivity analyses were performed in which the severe hypoglycemia event rate in the CSII arm was altered to 1 and 8 events, respectively, per 100 patient-months. Other sensitivity analyses conducted in this population included changes in time horizon and discount rate.
In the cohort with uncontrolled HbA1c the sensitivity analyses included both increasing and decreasing baseline HbA1c, increasing and decreasing sensor use to 61 and 43 sensors per year, respectively (vs. 49 per year in the base case analyses), changes in SAP with automated insulin suspension costs (−20, −10 and +10% relative to the base case), change in SMBG reduction (no reduction and SMBG use of 6.11 per day and 2.11 per day in the SAP with automated insulin suspension arm) and changes in time horizon, perspective and discount rate.
Results
Cohort at Increased Risk of Hypoglycemic Events
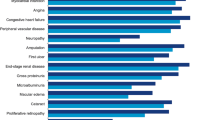
In the cohort at increased risk for hypoglycemia SAP with automated insulin suspension was associated with higher overall lifetime costs but also with a substantial gain in quality-adjusted life expectancy in the base-case analysis (Table 3). Total mean lifetime costsFootnote 1 were SEK 2,671,858 [euro (EUR) 279,968] per patient in the SAP with automated insulin suspension arm versus SEK 2,409,462 (EUR 252,473) per patient in the CSII arm. Direct costs were higher in the SAP with automated insulin suspension arm, but indirect costs were lower in this arm, likely driven by lower levels of lost productivity due to a lower cumulative incidence of diabetes-related complications. Mean quality-adjusted life expectancy was 13.11 quality-adjusted life years (QALYs) in the SAP with automated insulin suspension arm versus 11.23 QALYs in the CSII arm, leading to an incremental cost-effectiveness ratio (ICER) of SEK 139,795 (EUR 14,648) per QALY gained for SAP with automated insulin suspension versus CSII. Life expectancy (undiscounted) was also improved in the SAP with automated insulin suspension arm by an additional 0.45 years. When only direct costs were included in the analysis, the ICER for SAP with automated insulin suspension versus CSII increased to SEK 199,199 (EUR 20,873) per QALY gained. At a willingness-to-pay threshold of SEK 300,000 (EUR 31,435) per QALY gained, the likelihood of SAP with automated insulin suspension being considered cost-effective versus CSII was estimated to be 99%. Higher costs in the SAP with automated insulin suspension arm were driven primarily by higher incremental lifetime treatment costs [SEK 659,570 (EUR 69,112) vs. SEK 141,864 (EUR 14,865)], although these were partially offset by a lower projected incidence and by delay of onset of diabetes-related complications with SAP with automated insulin suspension (Table 4). The mean onset of all diabetes-related complications included in the analysis was delayed in the SAP with automated insulin suspension group relative to the CSII group; mean delay in onset with SAP with automated insulin suspension ranged from 0.1 years for microalbuminuria to 0.44 years for end-stage renal disease.
Sensitivity analysis showed that for this patient group the ICER was most sensitive to changes in severe hypoglycemic event rate in the CSII arm as such events can be associated with substantial medical resource use and high direct costs (Table 5). When the severe hypoglycemic event rate in the CSII arm was reduced to 1 per 100 patient-months the ICER increased to SEK 204,442 (EUR 21,422) per QALY gained. However, when the event rate for CSII was increased to 8 severe hypoglycemic events per 100 patient-months SAP with automated insulin suspension was dominant relative to CSII.
Cohort with Uncontrolled HbA1c at Baseline
In the base-case analysis for this patient group, SAP with automated insulin suspension was associated with higher total lifetime costs than CSII [SEK 1,925,040 (EUR 201,713) vs. SEK 1,656,141 (EUR 173,537)] and higher quality-adjusted life expectancy (9.22 vs. 8.16 QALYs), resulting in an ICER of SEK 251,896 (EUR 26,395) per QALY gained for SAP with automated insulin suspension versus CSII (Table 3). If only direct costs were included in the analysis, the ICER increased to SEK 328,323 (EUR 34,403) per QALY gained. The higher costs in the SAP with automated insulin suspension arm were driven by higher lifetime treatment costs [SEK 467,551 (EUR 48,992) vs. SEK 99,090 (EUR 10,383)], which were partially offset by lower complication costs due to a delay in onset and reduced cumulative incidence of diabetes-related complications in the SAP with automated insulin suspension arm. For this patient group, at a willingness-to-pay threshold of SEK 300,000 (EUR 31,435), the likelihood of SAP with automated insulin suspension being considered cost-effective compared with CSII was 58%, which increased to 74% at a willingness-to-pay threshold of SEK 360,000 (EUR 37,722) per QALY gained and to 84% at a threshold of SEK 420,000 (EUR 44,009) per QALY gained. In the SAP with automated insulin suspension arm the mean onset of diabetes-related complications included in the analysis was delayed by at least 0.6 years (Table 4). The most pronounced delays in onset of a long-term diabetes-related complication was for neuropathy, with an onset delay of a mean of 1.04 years in the SAP with automated insulin suspension arm relative to the CSII arm.
Sensitivity analyses in the cohort with uncontrolled HbA1c showed that outcomes were most sensitive to changes in baseline HbA1c and assumptions relating to the impact of FoH on quality of life (Table 5). In the base case, mean baseline HbA1c was 7.9% (63.1 mmol/mol). If baseline HbA1 was reduced to 7.5% (58 mmol/mol), then incremental gain in quality-adjusted life expectancy with SAP with automated insulin suspension decreased to 0.75 QALYs (compared with 1.07 QALYs in the base case), resulting in the ICER increasing to SEK 294,117 (EUR 30,819) per QALY gained. However, if baseline HbA1c was increased to 9.0% (75 mmol/mol), the ICER for SAP with automated insulin suspension versus CSII was reduced to SEK 196,009 (EUR 20,539) per QALY gained, suggesting that the SAP with automated insulin suspension may be most cost-effective in those patients with the poorest glycemic control at baseline. The benefit associated with reduced FoH was also found to be a key driver of outcomes. In a sensitivity analysis in which this utility benefit was entirely negated, the incremental gain in quality-adjusted life expectancy was reduced to 0.261 QALYs, which resulted in the ICER increasing to SEK 1,028,295 (EUR 107,749) per QALY gained. Similarly, when the FoH utility benefit was reduced to 0.0184 (compared with 0.0552 in the base case), the ICER increased to SEK 507,261 (EUR 53,153) per QALY gained.
Discussion
The results of our cost-effectiveness analyses of SAP with automated insulin suspension versus CSII in patients with type 1 diabetes in Sweden suggest that the former represents good value for money. SAP with automated insulin suspension was associated with better life expectancy and quality-adjusted life expectancy but higher costs relative to CSII, leading to ICERs of SEK 139,795 (EUR 14,648) per QALY gained for patients at increased risk for hypoglycemia and SEK 251,896 (EUR 26,395) per QALY gained for patients with uncontrolled HbA1c at baseline. It should also be noted that in analyses such as those presented here, for interventions that improve life expectancy this longer life expectancy can contribute to a “survival paradox” whereby patients accrue direct costs and experience complications over a longer period of time owing to higher life expectancy. Although there is no official willingness-to-pay threshold in Sweden, for both patient groups the ICERs estimated in the present analysis fall below a willingness-to-pay threshold of SEK 500,000 (EUR 52,392) per QALY gained. Indeed, at this threshold the probability of SAP with automated insulin suspension being considered cost-effective versus CSII exceeds 98% in both patient populations in the current analysis.
CSII is widely used in Sweden relative to many other European settings; in 2013, there were an estimated 10,000 patients using CSII, although figures on the proportion using SAP are lacking [35]. Further, the assessment of CSII by the Swedish Council on Health Technology Assessment (SBU) reported that CSII is the first choice treatment modality for young children with recently diagnosed type 1 diabetes. Use of CSII in adults is typically limited to those patients who cannot achieve adequate glycemic control on MDI, although data from the Swedish NDR suggest that this may be a sizable proportion of the overall type 1 diabetes population. Additionally, the SBU assessment of CGM, despite noting high levels of patient satisfaction with SAP, acknowledged that there is a general reluctance to offer CGM to adults in Sweden, even though short-term use has been shown to improve HbA1c [36]. The SBU report on CGM also highlighted uncertainty around the effect of CGM on rates of severe hypoglycemic events and ketoacidosis. However, since publication of that report, clinical evidence has accrued which suggests that SAP with automated insulin suspension contributes to a reduced incidence of hypoglycemic events, particularly nocturnal hypoglycemic events [12, 13, 16, 21].
Sensitivity analyses in the cohort with uncontrolled HbA1c showed that SAP with automated insulin suspension was most cost-effective in those patients with poorest glycemic control at baseline. This is likely driven by the fact that the incremental benefits of SAP with automated insulin suspension (in terms of improved HbA1c) are likely to be most pronounced in those patients with the worst glycemic control at baseline. Indeed, the treatment effect in terms of HbA1c reduction was sourced from formulae published by Pickup et al. [23] that take into account baseline HbA1c, in that patients with higher baseline HbA1c values have greater reductions in HbA1c that those with lower baseline HbA1c values. The resultant improvement in glycemic control with SAP with automated insulin suspension is a key driver of long-term outcomes. Patients with poor glycemic control are known to be at increased risk of diabetes-related complications. Data from the Swedish setting indicate that relative to the general population, type 1 diabetes patients with HbA1c levels of >7.8% (62 mmol/mol) have a more than threefold higher hazard ratio (HR) for all-cause mortality and a more than fourfold HR for cardiovascular mortality [37]. Additionally, data from the NDR suggest that the proportion of type 1 diabetes patients in Sweden not achieving good glycemic control, particularly in the younger age groups, may be substantial. For example, in one single-center retrospective longitudinal study in patients aged 18–24 years in Sweden, less than 10% patients had a mean HbA1c of ≤7.0% (53 mmol/mol) during the study period. Further, 22% of 24-year-olds and >50% of 18-year-olds had mean HbA1c values ≥9.1% (76 mmol/mol) [38]. In another analysis, also using NDR data from a total of 7454 patients aged 20–65 years, a total of 3268 (44%) patients had HbA1c levels of 8.0–11.9% (64–107 mmol/mol) at the start of the study [37]. Additionally, in Sweden, patients with poor glycemic control are also more likely to initiate insulin pump therapy, with this likelihood increasing in a non-linear fashion with higher HbA1c. For example, in one large-scale study involving >7000 patients, the HR for CSII initiation in patients with HbA1c values of ≥9.8% (83 mmol/mol) relative to those with HbA1c values of <6.0% (<42 mmol/mol) was 5.65 (95% confidence interval 2.98–10.72) [39]. Taken together, these figures suggest that, in Sweden, there is potentially a substantial number of patients with type 1 diabetes for whom switching to SAP with automated insulin suspension could be both clinically beneficial and cost-effective. In this patient cohort the impact of SAP with automated insulin suspension in terms of reduced FoH was also a key driver of outcomes. FoH has been shown to be particularly pronounced at night, and it also influences many aspects of disease management including diet, physical activity and insulin dosing, to the extent that some patients may deliberately tolerate higher blood glucose levels in order to lessen the risk of hypoglycemia [40]. For these patients, switching to SAP, especially advanced SAP devices with an automated insulin suspension feature, may help to alleviate the considerable burden associated with FoH while simultaneously enabling better glycemic control.
Sensitivity analysis in the cohort with uncontrolled HbA1c at baseline showed that outcomes were also influenced by the frequency of sensor use. Quality-adjusted life expectancy was 9.34 QALYs when a sensor use of 61 per year was assumed (compared with 9.22 QALYs with 49 sensors per year in the base-case analysis), but total costs in the SAP with automated insulin suspension arm also increased to SEK 1,967,223 (EUR 206,133). These projected outcomes are in line with findings from the STAR 3 trial, which reported that the magnitude of clinical benefit associated with SAP was influenced by the frequency of sensor use, with higher rates of sensor use being associated with better glycemic control [41]. In the STAR 3 trial, patients who used the sensor 0–20% of the time had a HbA1c reduction (from baseline to 1 year) of −0.43%, whereas for patients who used the sensor 81–100% of the time the reduction in HbA1c was −1.21%.
In the cohort at increased risk for hypoglycemic events the projected incidence of severe hypoglycemic events was a key driver of outcomes. Severe hypoglycemic events, although rare for most patients, can have potentially catastrophic consequences, including coma and even death; recent data have also indicated that a history of severe hypoglycemic events may lead to an elevated risk of mortality following cardiovascular events [42]. These events may also be associated with extensive medical resource use and high direct medical costs. In the current analysis, the direct cost of a severe hypoglycemic event was SEK 30,333 (EUR 3,178), based on published data from Jönsson et al. [43]. However, the current analysis did not take into account any potential benefit in terms of minor hypoglycemic events or indirect costs associated with severe hypoglycemic events. Indirect costs of non-severe hypoglycemic events are often overlooked but can be substantial, with estimates of lost work time ranging from 8.3 to 15.9 h per month [44].
There are a number of limitations associated with the findings of the analysis presented here. Notably, a fundamental limitation common to all health economic modeling analyses is the use of short-term clinical data to project long-term outcomes. For the analysis in patients at increased risk of hypoglycemic events, data from a clinical trial of 6 months duration in patients aged 5–49 years were utilized. The CORE diabetes model was developed using data from adult type 1 diabetes populations; as such, the inclusion of clinical input data from children and adolescents may limit the accuracy of projected long-term clinical outcomes for such patients. A further limitation is the relatively small-scale nature of the trial, which enrolled fewer than 100 patients. However, long-term, large-scale studies comparing SAP with automated insulin suspension versus CSII are lacking; therefore, the use of short-term clinical data represents the best available proxy for projecting long-term outcomes.
The findings of the current analysis concur with those of a previous cost-effectiveness analysis conducted in Sweden, which reported an ICER of SEK 367,571 (EUR 38,516) per QALY gained for SAP versus CSII [45]. However, SAP technology has advanced since the publication of this earlier analysis, with new features, such as predictive low glucose suspension, improving clinical benefits and, therefore, the cost-effectiveness of SAP. More recent analyses of SAP with automated insulin suspension versus CSII have been conducted in type 1 diabetes patients in other settings, including the UK [46], France [47] and Denmark [48]. The findings of these analyses concur with those of the present analysis in suggesting that SAP with automated insulin suspension is cost-effective compared with CSII in particular groups of type 1 diabetes patients in the UK, France and Denmark as well as Sweden.
Overall, the findings of our analysis suggest that in Sweden, for type 1 diabetes patients who continue to experience poor glycemic control, or severe hypoglycemic events despite CSII use, switching to SAP with automated insulin suspension is likely to represent a cost-effective treatment alternative.
Notes
Total costs refer to the total direct and indirect costs attributable to diabetes-related complications as well as the incremental device costs in the SAP arm. The cost of the CSII device was not included in the analysis as this was assumed to be the same in both arms.
References
Swedish National Diabetes Register. Annual report 2013. https://www.ndr.nu/pdfs/Annual_Report_NDR_2013.pdf. Accessed 19 Oct 2016.
Jendle JH, Rawshani A, Svensson AM, Avdic T, Gudbjörnsdóttir S. Indications for insulin pump therapy in type 1 diabetes and associations with glycemic control. J Diabetes Sci Technol. 2016;10:1027–33.
Skogsberg L, Fors H, Hanas R, Chaplin JE, Lindman E, Skogsberg J. Improved treatment satisfaction but no difference in metabolic control when using continuous subcutaneous insulin infusion vs. multiple daily injections in children at onset of type 1 diabetes mellitus. Pediatr Diabetes. 2008;9:472–9.
Fredheim S, Johansen A, Thorsen SU, et al. Nationwide reduction in the frequency of severe hypoglycemia by half. Acta Diabetol. 2014;52:591–9.
Jeitler K, Horvath K, Berghold A, et al. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in patients with diabetes mellitus: systematic review and meta-analysis. Diabetologia. 2008;51:941–51.
Monami M, Lamanna C, Marchionni N, Mannucci E. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in type 1 diabetes: a meta-analysis. Acta Diabetol. 2010;47(Suppl 1):77–81.
Misso ML, Egberts KJ, Page M, O’Connor D, Shaw J (2010) Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database Syst Rev. 20(1):CD005103.
Steineck I, Cederholm J, Eliasson B, Register Swedish National Diabetes, et al. Insulin pump therapy, multiple daily injections, and cardiovascular mortality in 18,168 people with type 1 diabetes: observational study. BMJ. 2015;350:h3234.
Battelino T, Conget I, Olsen B, et al., and the SWITCH Study Group (2012) The use and efficacy of continuous glucose monitoring in type 1 diabetes treated with insulin pump therapy: a randomised controlled trial. Diabetologia. 55:3155–62.
O’Connell MA, Donath S, O’Neal DN, et al. Glycaemic impact of patient-led use of sensor-guided pump therapy in type 1 diabetes: a randomised controlled trial. Diabetologia. 2009;52:1250–7.
Leelarathna L, Thabit H, Hartnell S, et al.; AP@home Consortium (2016) Rapid benefits of structured optimization and sensor-augmented insulin pump therapy in adults with type 1 diabetes. J Diabetes Sci Technol1(1):180-181.
Medtronic Inc. MNMiniMed 640G insulin pump with SmartGuard®. Medtronic Inc., Minneapolis, MN. https://www.medtronic-diabetes.co.uk/minimed-system/minimed-640g-insulin-pump. Accessed 20 July 2017.
Choudhary P, Shin J, Wang Y, et al. Insulin pump therapy with automated insulin suspension in response to hypoglycemia: reduction in nocturnal hypoglycemia in those at greatest risk. Diabetes Care. 2011;34:2023–5.
Agrawal P, Zhong A, Welsh JB, Shah R, Kaufman FR. Retrospective analysis of the real-world use of the threshold suspend feature of sensor-augmented insulin pumps. Diabetes Technol Ther. 2015;17:316–9.
Weiss R, Garg SK, Bode BW, et al. Hypoglycemia reduction and changes in hemoglobin A1c in the ASPIRE in-home study. Diabetes Technol Ther. 2015;17:542–7.
Fonseca VA, Grunberger G, Anhalt H, Committee Consensus Conference Writing, et al. Continuous glucose monitoring: a consensus conference of the American Association of Clinical Endocrinologists and American College of Endocrinology. Endocr Pract. 2016;22:1008–21.
Peters AL, Ahmann AJ, Battelino T, et al. Diabetes technology-continuous subcutaneous insulin infusion therapy and continuous glucose monitoring in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:3922–37.
Palmer AJ, Roze S, Valentine WJ, et al. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5–26.
Palmer AJ, Roze S, Valentine WJ, et al. Validation of the CORE diabetes model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20[Suppl 1]:S27–40.
McEwan P, Foos V, Palmer JL, Lamotte M, Lloyd A, Grant D. Validation of the IMS CORE diabetes model. Value Health. 2014;17:714–24.
Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. JAMA. 2013;310:1240–7.
Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Diabetes control and complications trial/epidemiology of diabetes interventions and complications (DCCT/EDIC) study research group. intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–53.
Pickup JC, Freeman SC, Sutton AJ. Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. BMJ. 2011;343:d3805.
Lynch P, Attvall S, Persson S, Barsoe C, Gerdtham U. Routine use of personal continuous glucose monitoring system with insulin pump in Sweden [abstract 1052]. Diabetologia. 2012;55[Suppl 1]:S432.
Statistics Sweden. Salary structures, whole economy. http://www.scb.se/en/finding-statistics/statistics-by-subject-area/labour-market/wages-salaries-and-labour-costs/salary-structures-whole-economy/. Accessed 19 Aug 2016.
Beaudet A, Clegg J, Thuresson PO, Lloyd A, McEwan P. Review of utility values for economic modeling in type 2 diabetes. Value Health. 2014;17:462–70.
McBride M, Eggleston A, Jones T, Ly T. PDB98—health-related quality of life in patients with type 1 diabetes and impaired hypoglycaemia awareness: the role of sensor-augmented insulin pump therapy with automated insulin suspension. Value Health. 2013;16(7):A448.
Nørgaard K, Scaramuzza A, Bratina N, et al. Sensor-augmented pump therapy in real-life: patients reported outcomes results of the INTERPRET observational study. Abstract 1058. European Association for the Study of Diabetes, Berlin 2012.
Nørgaard K, Scaramuzza A, Bratina N, et al. Routine sensor-augmented pump therapy in type 1 diabetes: the INTERPRET study. Diabetes Technol Ther. 2013;15:273–80.
Currie CJ, Morgan CL, Poole CD, et al. Multivariate models of health-related utility and the fear of hypoglycaemia in people with diabetes. Curr Med Res Opin. 2006;22:1523–34.
Statistics Sweden. Average monthly salary by sector 1992–2015. http://www.scb.se/en_/Finding-statistics/Statistics-by-subject-area/Labour-market/Wages-salaries-and-labour-costs/Salary-structures-whole-economy/Aktuell-Pong/14374/149087/. Accessed 4 Nov 2016.
Sørensen J, Ploug, Uffe J (2013) The cost of diabetes-related complications: registry-based analysis of days Absent from Work. Econ Res Int. 2013:e618039. doi:10.1155/2013/618039
Tandvårds-Och Läkemedelsförmånsverket 2003. General guidelines for economic evaluations from the Pharmaceutical Benefits Board (LFNAR 2003:2). http://www.tlv.se/Upload/English/Guidelines-for-economic-evaluations-LFNAR-2003-2.pdf. Accessed 20 Oct 2016.
Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2012;157:336–47.
Swedish Council on Health Technology Assessment. Insulin pumps for diabetes [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 22 Oct 2013. https://www.ncbi.nlm.nih.gov/books/NBK316443/pdf/Bookshelf_NBK316443.pdf. Accessed 21 Oct 2016.
Swedish Council on Health Technology Assessment. Continuous subcutaneous glucose monitoring for diabetes [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2013. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0084407/pdf/PubMedHealth_PMH0084407.pdf. Accessed 21 Oct 2016.
Lind M, Svensson AM, Kosiborod M, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014;371:1972–82.
Sparud-Lundin C, Ohrn I, Danielson E, Forsander G. Glycaemic control and diabetes care utilization in young adults with Type 1 diabetes. Diabet Med. 2008;25:968–73.
Carlsson BM, Andersson PN, Alnervik J, Carstensen J, Lind M. Availability of insulin pump therapy in clinical practice. Diabet Med. 2012;29:1055–9.
Martyn-Nemeth P, Schwarz Farabi S, Mihailescu D, Nemeth J, Quinn L. Fear of hypoglycemia in adults with type 1 diabetes: impact of therapeutic advances and strategies for prevention—a review. J Diabetes Complications. 2016;30:167–77.
Bergenstal RM, Tamborlane WV, Ahmann A et al. STAR 3 Study Group (2010) Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 363:311–20.
Lung TW, Petrie D, Herman WH, et al. Severe hypoglycemia and mortality after cardiovascular events for type 1 diabetic patients in Sweden. Diabetes Care. 2014;37:2974–81.
Jönsson L, Bolinder B, Lundkvist J. Cost of hypoglycemia in patients with Type 2 diabetes in Sweden. Value Health. 2006;9:193–8.
Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health. 2011;14:665–71.
Roze S, Saunders R, Brandt AS, de Portu S, Papo NL, Jendle J. Health-economic analysis of real-time continuous glucose monitoring in people with Type 1 diabetes. Diabet Med. 2015;32:618–26.
Roze S, Smith-Palmer J, Valentine WJ, Cook M, Jethwa M, de Portu S, Pickup JC. Long-term health economic benefits of sensor-augmented pump therapy vs continuous subcutaneous insulin infusion alone in type 1 diabetes: a UK perspective. J Med Econ. 2016;19(3):236–42.
Roze S, Smith-Palmer J, Valentine W, Payet V, de Portu S, Papo N, Cucherat M, Hanaire H. Cost-effectiveness of sensor-augmented pump therapy with low glucose suspend versus standard insulin pump therapy in two different patient populations with type 1 diabetes in France. Diabetes Technol Ther. 2016;18(2):75–84.
Roze S, de Portu S, Smith-Palmer J, Delbaere A, Valentine W, Ridderstråle M. Cost-effectiveness of sensor-augmented pump therapy versus standard insulin pump therapy in patients with type 1 diabetes in Denmark. Diabetes Res Clin Pract. 2017;128:6–14.
Henriksson F. Applications of economic models in healthcare: the introduction of pioglitazone in Sweden. Pharmacoeconomics. 2002;20(Suppl 1):43–53.
DRG costs for Sweden. http://sas.lf.se/kppprod/rap_vikt_tot_2004.htm.
Ghatnekar O, Persson U, Willis M, Odegaard K. Cost effectiveness of Becaplermin in the treatment of diabetic foot ulcers in four European countries. Pharmacoeconomics. 2001;19:767–78.
Acknowledgements
The study was funded by Medtronic International Trading Sàrl, Tolochenaz, Switzerland. Medtronic International Trading Sàrl also funded the article processing charges for this manuscript. All authors had full access to all of the data in this analysis and take complete responsibility for the integrity of the data and accuracy of the data analysis.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Simona de Portu, Alexis Delbaere, Natalie Papo, Johan Jendle and Stéphane Roze contributed to the design of the analysis, Stéphane Roze performed the analysis, Jayne Smith-Palmer prepared the first draft of the manuscript. William Valentine, Simona de Portu, Alexis Delbaere, Natalie Papo and Johan Jendle contributed to, reviewed and revised the first draft and subsequent drafts.
Disclosures
Stéphane Roze is a current employee of HEVA HEOR, which has received consulting fees from Medtronic. Jayne Smith-Palmer is a current employee of Ossian Health Economics and Communications, which has received consulting fees from Medtronic. William Valentine is a current employee of Ossian Health Economics and Communications, which has received consulting fees from Medtronic. Simona de Portu owns shares in and is a current employee of Medtronic International Trading Sarl. Alexis Delbaere is a current employee of Medtronic International Trading Sarl. Natalie Papo owns shares in and is a current employee of Medtronic International Trading Sarl. Johan Jendle has received honoraria from Medtronic for lectures and participating in advisory boards.
Compliance with Ethics Guidelines
This analysis does not contain data from any new studies with human or animal subjects performed by any of the authors.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any non-commercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/62FBF06076C858FE.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jendle, J., Smith-Palmer, J., Delbaere, A. et al. Cost-Effectiveness Analysis of Sensor-Augmented Insulin Pump Therapy with Automated Insulin Suspension Versus Standard Insulin Pump Therapy in Patients with Type 1 Diabetes in Sweden. Diabetes Ther 8, 1015–1030 (2017). https://doi.org/10.1007/s13300-017-0294-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-017-0294-z