Abstract
Insulin hypersensitivity—a rare occurrence with currently available insulin preparations—may have varied manifestations, ranging from a local injection site allergy to severe generalized anaphylactic reactions. While various additives included in commercial insulin preparations and insulin peptides themselves remain the primary allergens responsible, faulty injection technique may at times potentiate the development of insulin allergy. Management of insulin allergy is complex, potentially dangerous at times, and can be challenging for the treating physician. We report a case of insulin allergy due to intradermal insulin injections which was cured by adopting a proper injection technique.
Similar content being viewed by others
Introduction
Hypersensitivity to insulin preparations, ranging from a minor local injection site allergy to severe generalized and at times life-threatening anaphylactic reactions, currently affects <4% of diabetic patients treated with insulin [1]. The insulin peptide itself and the various additives present in the formulations are proposed to be the allergens responsible. A faulty injection technique and the resulting intradermal insulin administration can facilitate the development of such allergic reactions.
Case Report
A 65-year-old gentleman (body mass index 32.2 kg/m2) with a 10-year history of type 2 diabetes presented with a month-long history of burning sensation followed by appearance of a pruritic maculopapular rash in and around the injection site within half an hour after insulin administration. He had been using oral antihistaminics and topical steroids for symptomatic relief during the previous two weeks without much effect while the rash kept appearing after each shot of insulin administered. Frustrated with the repetitive allergic reactions, he became desperate to find an effective noninjectable antidiabetic medication. However, due to low stimulated C-peptide levels (0.4 ng/ml), his primary care physician insisted on continuation of the existing insulin therapy, which led him to omit the scheduled doses of insulin in a desperate attempt to avoid unpleasant local adverse reactions. Three months prior to this presentation he had been prescribed a twice-daily premixed human insulin (30% regular and 70% neutral protamine Hagedorn) in view of sustained poor glycemic control with optimal dosage of oral antidiabetic drugs. During the initial 2 months, his daughter used to inject insulin into his anterior abdomen after being taught how to perform insulin injection by the care giver. During that period, the injections were virtually painless, and the patient noticed satisfactory glycemic control without any skin changes around the injection site. However, with the marriage of his daughter he had started to self-inject himself and noticed development of an itchy rash after each and every injection. He did not experience itching on other body parts, or any cough, wheeze, or shortness of breath.
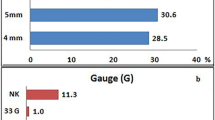
Examination of the injection sites revealed two long-standing keloid scars with multiple tender violaceous maculopapular rashes all over the anterior abdomen (Fig. 1). Baseline investigations (including a complete blood count, renal function test, liver function test, lipid profile, electrolytes, chest X-ray, and ECG) were normal except for an elevated absolute eosinophil count (982/cmm) and a mildly elevated serum IgE level [121.2 IU/ml (reference: 1–87 IU/ml)]. The urine spot albumin–creatinine ratio (ACR) was 178 mg/gm and the HbA1c was 9% on an NGSP allied assay. His detailed history revealed that he had been using a U-40 insulin syringe with a needle length of 4 mm and inserting the needle horizontally (at less than 15°) with respect to the plane of skin fold. With every faulty injection, he experienced significant pain and noticed the development of a small bleb over the application site. The faulty injection technique, new-onset pain, and the appearance of an intradermal bleb over the injection site was suggestive of intradermal insulin administration instead of subcutaneous administration. He had no family history of allergy or atopy, and he could not recollect any form of local or systemic allergic reaction to a particular agent in the past.
The insulin injection technique was rectified and the patient was advised to have a skin biopsy, which he declined. However, all of the rashes disappeared completely after 2 weeks and the patient did not notice similar symptoms after adopting the proper injection technique (Fig. 2).
Causality analysis for intradermal insulin injection and the allergic cutaneous lesions was performed using the World Health Organization–Uppsala Monitoring Centre (WHO-UMC) causality assessment scale and the Naranjo adverse drug reaction probability scale, and it was found that intradermal injection was the probable cause of the adverse drug reaction [probable/likely on the WHO-UMC causality assessment scale and probable (total score 8) on the Naranjo probability scale].
Discussion
The frequency of allergic reactions to insulin has declined significantly since the introduction of human recombinant insulin and insulin analogs into clinical practice. A common occurrence during the era of animal insulins because of altered peptide structures, presence of contaminants, highly immunogenic components such as C-peptide and proinsulin and the resulting greater antigenic potential, hypersensitivity reactions are now usually due to the presence of various pharmaceutical formula additives (protamine, meta-cresol, phenol, sodium phosphate, zinc, etc.) [2]. However, human insulin and insulin analogs can also act as potential allergens at times, and this has been observed with almost all currently available insulins. Insulin allergies can be local or systemic, as well as immediate or delayed. The underlying mechanisms of insulin-associated allergy can be divided into three types: type I (IgE-mediated), type III (IgG-mediated immune complex), and type IV (T-cell-mediated delayed-type) hypersensitivity. Type I hypersensitivity, which manifests as local edema, itching, wheals, and flares, is the most common form [3].
Various treatment options, ranging from symptom relief using simple antihistaminics to more complicated insulin desensitization therapy, have been advocated for managing allergic reactions to insulin [1, 3]. Though systemic corticosteroids can be used for symptom relief, they aggravate hyperglycemia, and changing the insulin to oral hypoglycemic agents may not possible in cases of type 1 or a long-standing insulinopenic spectrum of type 2 diabetes, as in this patient. Changing the insulin preparation to another preparation has also been used with success due to subtle differences in amino acid sequences and antigenicities between different insulins [4, 5].
Epidermal Langerhans cells acting as antigen-presenting cells transport foreign antigen to T lymphocytes and play a pivotal role in the initiation of cutaneous immune responses, including immune responses to chemical allergens encountered at skin surfaces. The development of insulin allergy following intradermal insulin administration may be explained by easy and extensive availability of antigens to resident Langerhans cells in the epidermis and subsequent augmentation of a localized immune response [6].
Conclusion
Though faulty injection technique is a simple and easily treatable cause of injection site allergy in insulin-treated diabetics, it is often overlooked in clinical practice. To the best of our knowledge, such an association has rarely been described in the global literature [7]. To conclude, treating physicians should enquire about injection technique when managing patients with an insulin allergy, as this may avoid the need to explore other costly, complicated, and potentially dangerous treatment alternatives.
References
Jacquier J, Chik CL, Senior PA. A practical, clinical approach to the assessment and management of suspected insulin allergy. Diabet Med. 2013;30:977–85.
Belhekar MN, Pai S, Tayade P, Dalwadi P, Munshi R, Varthakavi P. A case of hypersensitivity to soluble and isophane insulins but not to insulin glargine. Indian J Pharmacol. 2015;47(2):227–9.
Rojas J, et al. Successful management of insulin allergy and autoimmune polyendocrine syndrome type 4 with desensitization therapy and glucocorticoid treatment: a case report and review of the literature. Case Reports Immunol. 2014;2014:394754.
Kim GJ, et al. Two cases of allergy to insulin in gestational diabetes. Endocrinol Metab (Seoul). 2015;30(3):402–7.
Fujishiro M, et al. A case of insulin allergy successfully managed using multihexamer-forming insulin degludec combined with liraglutide. Diabet Med. 2016. doi:10.1111/dme.12998 (Epub ahead of print).
Cumberbatch M, Dearman RJ, Griffiths CE, Kimber I. Epidermal langerhans cell migration and sensitisation to chemical allergens. APMIS. 2003;111(7–8):797–804.
Sanyal T, Ghosh S, Chowdhury S, Mukherjee S. Can a faulty injection technique lead to a localized insulin allergy? Indian J Endocrinol Metab. 2013;17:S358–9.
Acknowledgments
No funding or sponsorship was received for this study or the publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this manuscript, take responsibility for the integrity of the work as a whole, and have given their final approval of the version to be published.
Disclosure
Partha Pratim Chakraborty, Sugata Narayan Biswas, and Shinjan Patra declare no conflict of interest.
Compliance with Ethics Guidelines
Informed consent to be included in this study was obtained from the patient.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chakraborty, P.P., Biswas, S.N. & Patra, S. Faulty Injection Technique: A Preventable But Often Overlooked Factor in Insulin Allergy. Diabetes Ther 7, 163–167 (2016). https://doi.org/10.1007/s13300-016-0151-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-016-0151-5