Abstract
Introduction
Although insulin is one of the most effective interventions for the treatment of type 2 diabetes, its disadvantages incur substantial medical cost. This study was designed to evaluate the medical costs of Swedish type 2 diabetic patients initiating insulin on top of metformin and/or sulfonylurea (SU), and to evaluate if costs before and after insulin initiation differ for patients where insulin is initiated above or below the recommended glycosylated hemoglobin (HbA1c) level (7.5%).
Methods
This was a register-based retrospective cohort study in which patients were identified from the Sörmland county council diabetes register. Patients being prescribed at least one prescription of metformin and/or SU from 2003 to 2010, and later prescribed insulin, were included.
Results
One hundred patients fulfilled the inclusion criteria and had at least 1 year of follow-up. The mean age was 61 years and 59% of patients were male. Mean time since diagnosis was 4.1 years, and since initiation of insulin was 2.2 years. The mean HbA1c level at index date was 8.0%. Total mean costs for the whole cohort were SEK 17,230 [standard deviation (SD) 17,228] the year before insulin initiation, and SEK 31,656 (SD 24,331) the year after insulin initiation (p < 0.0001). When stratifying by HbA1c level, patients with HbA1c <7.5% had total healthcare costs of SEK 17,678 (SD 12,946) the year before the index date and SEK 35,747 (SD 30,411) the year after (p < 0.0001). Patients with HbA1c levels ≥7.5% had total healthcare costs of SEK 16,918 (SD 19,769) the year before the index date and SEK 28,813 (SD 18,779) the year after (p < 0.0001).
Conclusion
Despite the small sample size, this study demonstrates that mean annual medical costs almost double the year after patients are initiated on insulin. The costs increased the year after insulin initiation, regardless of the HbA1c level at initiation of insulin, and the largest increase in costs were due to increased filled prescriptions.
Similar content being viewed by others
Introduction
In Sweden, the prevalence of diabetes mellitus has recently been estimated to be 4.4% among the adult population, with type 2 diabetes accounting for approximately 90% of all cases [1]. As diabetes is a major cause of morbidity and premature mortality, the disease has a significant impact on healthcare costs and quality of life (QoL) [2, 3].
It is well established that adequate glycemic control [glycosylated hemoglobin (HbA1c) below 6.5–7%] reduces the risk of diabetes-related complications, and this is therefore the key goal in management of type 2 diabetes [4]. Insulin is one of the most effective HbA1c-lowering interventions and, due to the progressive nature of type 2 diabetes at higher HbA1c-levels, insulin may be the only treatment option for many patients [5]. According to the Swedish National Board of Health and Welfare’s clinical guidelines on management of type 2 diabetes [6], the first preventive measure to decrease HbA1c is lifestyle intervention and later initiation of metformin. When these measures fail to control glucose levels and the HbA1c-level rises to 7.5%, treatment with a sulfonylurea (SU) or insulin should be initiated. There are alternative approved treatment options that may be initiated before prescribing insulin, if HbA1c levels are <7.5% and the patient does not respond to metformin, including sitagliptins and GLP-1 receptor antagonists. However, many physicians choose to initiate insulin before the patient has reached an HbA1c level of 7.5%. Insulin treatment has a number of disadvantages, such as weight gain, reaction from the injection and hypoglycemia [7], and in particular during the early period of initiating insulin, patients most likely show psychologic insulin resistance [8] resulting in complications and increased healthcare costs.
Although there are a number of published studies evaluating the costs of Swedish patients with type 2 diabetes [9–11], there are to our knowledge no Swedish studies comparing the costs of pre- and post-initiation of insulin. There is also little evidence when stratifying annual medical costs before and after initiation of insulin in patients with HbA1c-level of <7.5%, where other treatment options are still available, versus HbA1c-level ≥7.5%. The aims of this study were to evaluate the healthcare costs of patients with type 2 diabetes initiating insulin on top of metformin and/or SU, and to understand if these costs differ if the patient has reached HbA1c levels of 7.5% or not. If the results from this study indicate that treatment with insulin on top of metformin is related to substantially higher healthcare costs compared with treatment with metformin and/or SU alone, this could be an indication that other oral anti-diabetic drugs (OADs) apart from metformin could be favored while HbA1c is still below critical levels. This could have an impact both in terms of savings of healthcare resources and on patients’ QoL.
Methods
This study is a register-based retrospective cohort study including Swedish patients with type 2 diabetes who started treatment with metformin and/or SU and were later prescribed insulin.
Study Population
All patients were identified from the Sörmland county council diabetes register. The register includes information on patients with type 2 diabetes receiving treatment within the county council from 2003 to 2004 onwards, as well as information on caregiver contacts, laboratory tests (including HbA1c values), diagnoses, procedures, prescribed drugs, and demographics. Information on filled prescriptions and devices were retrieved from the prescribed drug register, which is a national register held at the National Board of Health and Welfare containing information on all prescribed medicines and pharmaceutical aids dispensed at Swedish pharmacies since June 2005. Information on mortality during the follow-up period was retrieved from the cause of death register at the National Board of Health and Welfare. The register includes nationwide data since 1961 and includes underlying and contributory causes of death according to the International Classification of Disease (ICD) system. This study included all patients in the diabetes register identified as being prescribed at least one prescription of metformin and/or SU from 2003 to 2010 and later prescribed treatment with insulin. Patients were excluded from the study if they were being prescribed insulin before June 2005, had an initial diagnosis of type 1 diabetes, had records of prescriptions of OADs other than metformin or SU prior to the index date, or if they had no records of metformin or SU prior to the index date.
After approval from an ethical committee, data were extracted from the diabetes register based on the inclusion criteria and linked to the administrative registers at the National Board of Health and Welfare through the patients’ national registration number. All identifiable data were replaced with new study IDs to de-identify the data.
For each identified patient, the index date was defined as the date of the first insulin prescription in the diabetes register during the period January 1, 2005 through December 31, 2009. The HbA1c level at initiation of insulin used in the stratified analysis was chosen as the last HbA1c lab value measured prior to the index date. The aim was to choose a value measured within 1 month and not longer than 3 months before insulin initiation.
HbA1c was measured using the Mono-S method [12]. For conversion to measurements with the DCCT/NGSP method, the following conversion formula may be used: HbA1c (NGSP) (%) = 0.956 × HbA1c (Mono S) (%) + 1.182 (see e.g., http://www.hba1c.nu/).
Annual medical costs were computed from the third party payer perspective for healthcare visits, treatment interventions, and procedures (described as DRG) and prescriptions of anti-glycemic medications, diabetic devices, and aids. For the purpose of estimating costs incurred in the management before and after the initiation of insulin, unit costs for individual procedures were derived based on DRG-codes in the diabetes register. Unit costs for healthcare resources were obtained through three different county council lists for costs and calculated as a mean of the three measures (including Skane county [13], Vastragotaland region county council [14] and Norrlands lans county council [15]) according to Swedish standards. These unit costs varied by resource use, and were applied to the resource utilization items, which were used to calculate the overall medical costs of healthcare utilization. Costs for prescribed drugs were primarily based on the information from the prescribed drug register including updated information on national costs from the latest reference year. Costs were calculated on an individual basis by summing the products of unit costs with quantities of different types of resources consumed and presented as means for all patients. The latest reference year for unit costs was used (SEK 2012; 1 € = 8.4 SEK on March 25, 2013).
Analyses were conducted using patient-level data, but all reporting was on an aggregated level. All data management and statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Statistical Considerations
The resource use items available within this study were visits to primary care, outpatient admissions to medical wards, surgeries and procedures through DRG-codes, prescription pharmaceuticals, and devices for glucose-monitoring and insulin administration. Annual quantities of these resource items during the 12-month post-initiation of insulin were determined for each patient. Healthcare costs during the 12-month post-initiation of insulin were estimated by multiplying quantities of resource use by unit costs from published sources. Similarly, annual quantities of resource use during the year pre-initiation of insulin were determined for each patient, and corresponding healthcare costs were estimated by multiplying quantities of resource use with unit costs.
Descriptive statistics on an aggregated level were used to present patient characteristics, resource utilization, and costs for all patients in the dataset. For continuous variables, the arithmetic mean, standard deviation (SD), minimum, and maximum are presented. For categorical variables, the proportions (percentage) in each category are presented. The normality of the distributions was tested employing the Shapiro–Wilks test and by plotting the data. If found not to be normally distributed, means and SD were estimated using the bias corrected accelerated bootstrapping method with replacement. To test differences between costs before and after the index date, a t test was used to measure if the difference between the two costs was separated from zero. There were no missing values in the dataset and imputation of missing data was not necessary. Variables describing patient characteristics included age at the index date, sex, height, weight, co-morbidities, HbA1c level at the index date, systolic blood pressure at the index date, and diastolic blood pressure at the index date.
The estimated healthcare costs were subsequently stratified by HbA1c level at index date and statistical tests were used to compare costs pre- and post-initiation of insulin for each HbA1c-group separately (Group 1 <7.5%, Group 2 ≥7.5%).
Results
The selection of patients is presented in Fig. 1. In total, 667 patients initiated on insulin during the study period were identified and extracted from the diabetes register. After removing patients who had been treated with OADs other than metformin or SU prior to the index date, had a primary diagnosis of type 1 diabetes, had been prescribed insulin prior to the index date, had not been prescribed metformin or SU prior to the index date, and had <365 days follow-up before or after the index date, 100 patients were eligible for the analysis.
Patient Characteristics
Patient characteristics are demonstrated in Table 1. The mean age of the patients was 64 (SD 10) years, ranging from 35 to 80 years. Most patients were men (n = 59, 59%).
There were 41 patients who were initiated on insulin at HbA1c levels <7.5%, and 59 patients at Hba1c levels ≥7.5%. Patient characteristics comparing patients with HbA1c level <7.5% and ≥7.5% at the index date are shown in Table 2. Patients with HbA1c levels <7.5% were older than those with HbA1c levels ≥7.5% at the index date [67 (SD 7) vs. 63 (SD 11) years, p = 0.051]. The mean HbA1c level at the index date was 6.7% (SD 0.7%) among the HbA1c level <7.5% group and 8.9% (SD 1.6%) among the HbA1c ≥7.5% group (p = 0.0001). There was also a statistically significant difference between the two groups in terms of diastolic blood pressure [77.2 mmHg (SD 9.1) vs. 82.1 mmHg (SD 11.3), p = 0.018]. Even though total number of co-morbidities did not differ between the two groups, patients with HbA1c levels <7.5% had a higher number of cardiovascular events (see Table 3).
Costs
Total medical costs for the total cohort, and stratified by HbA1c-level, are shown in Tables 4 and 5, respectively.
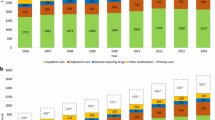
The total medical healthcare costs for the entire cohort the year before initiation of insulin (Table 4) were SEK 17,230 (SD 17,228), and the year after were SEK 31,656 (SD 24,331) (p < 0.0001). The highest proportion of costs before the index date was as a result of visits to primary care followed by costs due to visits to medical wards, procedures and medications, whilst the highest proportion after the index date were due to medications, followed by visits to primary care, visits to medical wards, and procedures.
When stratifying total medical healthcare costs by HbA1c group (Table 5), the group with HbA1c levels <7.5% had total medical costs of SEK 17,678 (SD 12,946) the year before the index date, and SEK 35,747 (SD 30,411) the year after the index date (p < 0.0001). The group with HbA1c levels ≥7.5% had total medical costs of SEK 16,918 (SD 19,769) the year before the index date and SEK 28,813 (SD 18,779) the year after the index date (p < 0.0001). In patients with HbA1c levels <7.5%, the year before initiation of insulin, the highest proportion of costs was due to visits to primary care, followed by costs due to visits to medical wards, medications, and procedures. The year after the index date, the highest costs were due to medications, followed by costs due to visits to primary care, visits to medical wards, and procedures. In the group with HbA1c levels ≥7.5% at the index date, the year before initiation of insulin, the highest proportion of costs was due to visits to primary care, followed by costs due to visits to medical wards, procedures, and medications. The year after the index date, the highest costs were due to medications, followed by costs due to visits to primary care, visits to medical wards, and procedures.
The total medical costs due to health care visits in the entire patient cohort were SEK 11,795 (SD 10,366) the year before the index date and SEK 18,289 (SD 16,955) the year after the index date (p < 0.0001). The highest proportion of this was due to visits to primary care both before and after the index date [SEK 6,801 (SD 4,539) pre-index; SEK 10,486 (SD 7,202) post-index, p < 0.0001]. The costs due to visits to medical wards were SEK 4,994 (SD 9,565) the year before the index date and SEK 7,803 (SD 16,224) the year after the index date (p = 0.039). Even though not statistically significant, the costs related to visits to medical wards included visits to physicians and nurses, both before and after the index date. There were no statistically significant differences in mean costs the year before and after the index date due to procedures.
There were no statistically significant differences in costs due to health care visits before and after the index date compared with the year before the index date in patients with HbA1c levels <7.5% at the index date (p = 0.118). The mean total medical costs due to health care visits were lower in the group with HbA1c levels ≥7.5% at the index date compared with the group with HbA1c levels <7.5%, both the year before the index date [SEK 10,400 (SD 10,423)], and the year after [SEK 17,084 (SD 16,856)]. The total mean costs the year after the index date were statistically significantly higher than the year before (p < 0.0001). The highest proportion of these costs were due to visits to primary care [SEK 6,302 (SD 4,776) pre-index; SEK 10,823 (SD 7,898) post-index, p < 0.0001], whereas the costs due to visits to medical wards incurred SEK 4,098 (SD 9,268) the year before the index date and SEK 6,262 (SD 16,296), the year after the index date (p = 0.711).
In the total cohort, there was a statistically significant increase in mean total medical costs related to filled prescriptions the year after the index date [SEK 10,522 (SD 5,624)] compared with the year before the index date [SEK 2,540 (SD 1,929); p < 0.0001]. The highest mean costs related to insulin devices and aids were due to test sticks both before and after the index date [SEK 1,447 (SD 1,554) pre-index; SEK 3,342 (SD 3,290) post-index; p < 0.0001] (data not presented in the table).
The total mean costs due to filled prescriptions among the HbA1c <7.5% group were statistically significantly higher the year after the index date compared with the year before the index date [SEK 3,024 (SD 2,306) pre-index; SEK 9,732 (SD 4,657) post-index; p < 0.0001]. The same statistically significant difference was seen in the group with HbA1c levels ≥7.5% at the index date [SEK 2,203 (SD 1,551) pre-index; SEK 11,071 (SD 6,187) post-index; p < 0.0001].
Discussion
This study aimed at estimating and comparing annual medical costs the year before and after initiation of insulin (index date) among Swedish patients with type 2 diabetes. The study also aimed at estimating these costs stratified by HbA1c level at the date of initiation of insulin, based on the recommended cut-off level (HbA1c ≥7.5%).
Our results demonstrated almost doubled, statistically significant increases in mean annual costs the year after the initiation of insulin compared with the year before. The highest proportion of mean annual medical costs was due to visits to primary care the year before the index date, but shifted to costs due to filled prescriptions the year after. This demonstrates that filled prescriptions of insulin have a significant impact on the total medical costs. The increased costs of filled prescriptions were also due to increased filled packages of devices and aids such as glucose monitoring, injection needles, and lancets. Besides filled prescriptions, the increased costs the year after initiation of insulin were also due to increased visits to nurses and physicians, to both medical wards (not statistically significant), and to primary care.
As can be expected in a diabetes population, many of the patients in this study had cardiovascular co-morbidities that might explain some of the increased costs the year after initiation of insulin.
There were no major differences in demographic and clinical characteristics at the index date when comparing patients with HbA1c-levels <7.5% or ≥7.5% at the index date. Both groups had statistically significant increased mean annual costs the year after initiation of insulin compared with the year before. Interestingly, patients with HbA1c-levels <7.5% at the index date had higher total medical costs, both the year before the index date and the year after, compared with the HbA1c-level ≥7.5% group. This might be explained by the higher proportion of major cardiovascular events in this group, but the major increase in costs the year before and after index date was still explained by an increase in filled prescriptions. For both groups, costs were mainly dominated by costs due to health care visits before the index date, whereas costs due to filled prescriptions were more prominent in both groups after the index date.
There are a number of published studies assessing the health-related costs in patients treated with insulin. In a German study published in 1997, estimation of costs for insulin treated patients was approximately six times as high as those for patients treated with OADs, and 30 times as high as for patients treated with life-style interventions through specific diets [8]. Another German study by Liebl et al. [16], estimated direct annual costs 6 months before and after initiation of insulin. The authors demonstrated that there was a significant increase in blood glucose devices during the 6 months after initiation of insulin, and that the mean 6-month costs increased from €579 to €961. A more recent study conducted in Spain [10] in 2011 reported that mean total healthcare costs per patient 6 months before and after insulin start were €639 and €1,110, respectively. Mean total costs 6 months after insulin treatment was initiated included costs of hospitalization (31%), insulin (16%), primary care (14%), blood glucose monitoring (14%), specialized care (13%), OADs (8%), and other diabetes-related treatments (4%). In a Canadian cost-effectiveness study from 2011 [11], basic treatment with metformin was compared with different second-line treatments added on top of metformin. The average lifetime cost (direct healthcare cost) was reported to be $39,924 for the basic treatment with metformin. The corresponding cost was $40,669 for metformin plus SU, $47,191 for metformin plus DPP-4 inhibitor, $47,348 for metformin plus basal insulin, and $52,367 for metformin plus biphasic insulin. Hence, the incremental cost of adding basal insulin or biphasic insulin to the metformin treatment was $7,424 and $12,443, respectively.
The results in our study demonstrate that increased medical healthcare costs the year before and after initiation of insulin are comparable with the results of previous studies [16–19]. Together these data concur that the initiation of insulin treatment in type 2 diabetic patients increases medical costs, both in terms of increased costs due to filled prescriptions of medications and of devices, but also due to increased costs due to health care visits. Similar to the results in the study by Costi et al., our study demonstrated that the highest proportion of costs the year after the index date were due to filled prescriptions (given that our study did not include information on hospitalizations).
Studies have also demonstrated the relationship between costs and HbA1c level. In a study by Aagren et al. [20], from 2011, the relationship between glycemic control, measured by HbA1c-level, and short-term healthcare costs was assessed. The population consisted of commercially insured diabetic patients (HbA1c level ≥6%) in the United States; 34,469 patients with type 2 diabetes and 1,837 with type 1 diabetes. The study concluded that the HbA1c-level (and other factors) significantly correlated with diabetes-related short-term medical costs for both patients with type 1 and type 2 diabetes. Specifically, a 1%-point increase in HbA1c will, on average, lead to a 4.4% increase in diabetes-related medical costs for type 2 diabetes. These results were not comparable with the results in our study, which is probably explained by the higher major cardiovascular co-morbidities in this group. This difference might be more evident after a longer follow-up period. One reason for the difference in results compared to our study might be the selected study population. In our study, costs were calculated for patients who had at least 365 days follow-up both before and after the index date. By using such an approach, patients who had <365 days usage of metformin or SU before the index date, and patients who died before 365 days after the index date, were excluded from the analysis. Exclusion of these patients might therefore have biased the study population by allowing only patients with less severe disease to be included in the analysis.
Our study has a number of limitations. First, the study sample is very small and limited to one county council and the results might therefore not be generalizable to other parts of Sweden. This is probably especially evident in terms of the sub-group analysis. Secondly, healthcare utilization is limited to procedures, outpatient visits at medical wards, and primary care visits, and does not account for inpatient and other outpatient care or emergency care. There was also limited information on background data for co-morbidities and body mass index, limiting the possibilities to control for confounders. Also, when combining the two data sources, there were some differences between the different registers that led to some uncertainties in the data. Furthermore, it is important to recognize that the full clinical and economic benefits of an effective diabetes treatment, such as insulin, in the long run are not fully accounted for in our study.
Conclusion
In summary, despite the small sample size, this study demonstrates that mean annual medical costs almost double the year after patients are initiated on insulin. This increase in costs is mainly due to increased visits to primary care and increased drug prescriptions. This study also demonstrates that costs increase the year after initiation of insulin regardless of the HbA1c level at initiation of insulin, which could be a rational for other treatment options when HbA1c levels are still below the recommended threshold for initiation of insulin.
Key Summary Points
-
This register-based, retrospective cohort study was designed to evaluate the healthcare costs of patients with type 2 diabetes initiating insulin on top of metformin and/or sulfonylurea (SU) in Sweden, determine the glycosylated hemoglobin (HbA1c)-level at initiation of insulin, and stratify healthcare costs by this HbA1c-level.
-
Patients were identified from the Sörmland county council diabetes register; 100 patients being prescribed at least one prescription of metformin and/or SU from 2003-2010, and later prescribed insulin, were included.
-
The mean age was 61 years, 59% of patients were male. Mean time since diagnosis was 4.1 years and since initiation of insulin was 2.2 years, and the mean HbA1c level at index date was 8.0%.
-
Total mean costs for the whole cohort the year before initiation of insulin was SEK 17,230 (17,228) and the year after was SEK 31,656 (24,331) (p < 0.0001).
-
Despite the small study sample, this study demonstrates that mean annual medical costs almost double the year after patients are initiated on insulin; the costs increased regardless of the HbA1c level at initiation of insulin, with the largest increase in costs due to increased filled prescriptions.
References
Wirehn AB, Karlsson HM, Carstensen JM. Estimating disease prevalence using a population-based administrative healthcare database. Scand J Public Health. 2007;35(4):424–31.
Kanavos P, van den Aardweg S, Schurer W. Diabetes expenditure, burden of disease and management in 5 EU countries. London School of Economics; 2012. http://www.lse.ac.uk/lsehealthandsocialcare/research/lsehealth/mtrg/lsediabetesreport26jan2012.pdf (Accessed 29 July 2013).
Wandell PE. Quality of life of patients with diabetes mellitus. An overview of research in primary health care in the Nordic countries. Scand J Prim Health Care. 2005;23(2):68–74.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53.
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2009;52(1):17–30.
National Guidelines for Diabetes Care. Swedish National Board of Health and Welfare; 2012. http://www.socialstyrelsen.se/nationellariktlinjerfordiabetesvarden (Accessed 29 July 2013).
Srinivasan BT, Jarvis J, Khunti K, Davies MJ. Recent advances in the management of type 2 diabetes mellitus: a review. Postgrad Med J. 2008;84(996):524–31.
Gherman A, Veresiu IA, Sassu RA, Schnur JB, Scheckner BL, Montgomery GH. Psychological insulin resistance: a critical review of the literature. Pract Diab Int. 2011;28(3):125–28d.
Ringborg A, Martinell M, Stalhammar J, Yin DD, Lindgren P. Resource use and costs of type 2 diabetes in Sweden—estimates from population-based register data. Int J Clin Pract. 2008;62(5):708–16.
Jonsson B. Revealing the cost of Type II diabetes in Europe. Diabetologia. 2002;45(7):S5–12.
Henriksson F, Agardh CD, Berne C, et al. Direct medical costs for patients with type 2 diabetes in Sweden. J Intern Med. 2000;248(5):387–96.
Koskinen LK. Specificity of hemoglobin A1c measurement by cation exchange liquid chromatography. Evaluation of a Mono S column method. Clin Chim Acta. 1996;253(1–2):159–69.
Region Skane; 2012. http://www.skane.se/sv/ (Accessed 29 July 2013).
Vastragotaland region county council; 2012. http://www.vregion.se/ (Accessed 29 July 2013).
Norrlands lans county council; 2012. http://www.norrlandstingen.se/ (Accessed 29 July 2013).
Liebl A, Breitscheidel L, Nicolay C, Happich M. Direct costs and health-related resource utilisation in the 6 months after insulin initiation in German patients with type 2 diabetes mellitus in 2006: INSTIGATE study. Curr Med Res Opin. 2008;24(8):2349–58.
Costi M, Smith H, Reviriego J, Castell C, Goday A, Dilla T. Direct health care costs in patients with type 2 diabetes mellitus six months after starting insulin treatment in Spain: the INSTIGATE study. Endocrinol Nutr. 2011;58(6):274–82.
von Ferber L, Koster I, Hauner H. A cost of illness study of diabetes mellitus. Gesundheitswesen. 1997;59(1):17–22.
Klarenbach S, Cameron C, Singh S, Ur E. Cost-effectiveness of second-line antihyperglycemic therapy in patients with type 2 diabetes mellitus inadequately controlled on metformin. CMAJ. 2011;183(16):E1213–20.
Aagren M, Luo W. Association between glycemic control and short-term healthcare costs among commercially insured diabetes patients in the United States. J Med Econ. 2011;14(1):108–14.
Acknowledgments
Sponsorship and article processing charges for this study was funded by Merck Sharp & Dohme.
Conflict of interest
Christin Bexelius has received research grants from Merck Sharp & Dohme. Xuan Wang has received research grants from Merck Sharp & Dohme. Jenny Berg has received research grants from Merck Sharp & Dohme. Johan Lundberg is an employee of Merck Sharp & Dohme, a subsidiary of Merck & Co., Inc., owns stock options and stock in Merck & Co., Inc. Hans Hjelm declares that he has no conflict of interest.
Compliance with ethics guidelines
The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bexelius, C., Lundberg, J., Wang, X. et al. Annual Medical Costs of Swedish Patients with Type 2 Diabetes Before and After Insulin Initiation. Diabetes Ther 4, 363–374 (2013). https://doi.org/10.1007/s13300-013-0035-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-013-0035-x