Abstract
Introduction
People with diabetes are at a higher risk of developing a variety of medical conditions relative to those without diabetes, resulting in increased healthcare costs. Self-monitoring of blood glucose (SMBG) is accepted as a recommended element of effective diabetes self-management. However, little is known about the real-world frequency and actual expenditures associated with SMBG, as well as the impact of SMBG costs relative to the cost of diabetes treatments. The primary objective is to evaluate the real-world utilization and costs of SMBG tests in Canada among insulin-treated diabetes patients during a 12-month follow-up period.
Methods
A retrospective cohort study was conducted using the IMS Brogan Inc. Drug Plan database from July 1, 2006 through June 30, 2010. Total costs during the 12-month follow-up period were assessed, focusing on blood glucose (BG) testing strip costs, insulin therapy costs, and costs associated with oral antidiabetics medications. All prevalent patients with two or more prescriptions for insulin between January 1, 2007 and December 31, 2009 were initially included in the analysis, the first prescription serving as their index date. Depending on the insulin type(s) used, patients were subcategorized into one of four insulin regimen groups (basal, bolus, premix, or basal–bolus).
Results
Among an initial sample of patients with two or more claims for insulin between January 1, 2007 and December 31, 2009, 142,551 met the aforementioned inclusion and exclusion criteria. An overall mean utilization of pharmacy-based blood glucose testing of approximately 1,094 strips per person per year was observed, with an average cost per testing strip of Canadian $0.79. SMBG treatment costs for insulin users ($860), specifically those associated with prescription testing strips, totaled 41.6% of the average annual pharmacy costs of diabetes-related prescriptions ($2,068).
Conclusion
This study shows that SMBG accounts for approximately 40% of the total diabetes-related pharmacy costs for insulin users.
Similar content being viewed by others
Introduction
For both type 1 and type 2 diabetes, an essential component of ongoing clinical and self-care management of diabetes is sufficient and accurate glycemic control, which is critical in preventing or postponing complications resulting from diabetes, such as heart disease, kidney disease, nerve damage, and peripheral vascular disease [1, 2]. The most common means for measuring glycemic control is by monitoring glycated hemoglobin (HbA1c), which gives an average of the blood glucose over 3 months. A limitation of this method is that measuring HbA1c levels does not tell patients what their blood glucose levels are on a regular, daily basis. Self-monitoring by testing for urinary glucose is one method of checking if blood glucose is high, but the limitation of this test is that it lacks the proven accuracy of other methods. A more precise reading can be captured by blood testing, which is performed by pricking the skin to obtain a drop of blood, placing that sample on a testing strip, and gauging the result with a discrete meter. This method, called self-monitoring of blood glucose (SMBG), is quite flexible and convenient in that it can be done at various points throughout the day, prior to or following meals, or before or after physical activity, allowing patients to be constantly informed of their insulin levels [2].
SMBG in patients with diabetes who use insulin may contribute to improved glycemic control and reduced hypoglycemia by allowing self-adjustments of insulin dose to be made based on meter readings. SMBG is recognized as a core component of effective diabetes self-management for insulin users throughout the world by major international organizations such as the American Diabetes Association (ADA) and the International Diabetes Federation (IDF) [3–6]. SMBG is recommended by the Canadian Diabetes Association. The Canadian guidelines, while stating that the frequency of SMBG should be determined on an individual level, conclude that SMBG is an essential part of diabetes management for patients with type 1 diabetes and state that the benefits and optimal frequency are less clear for type 2 [7].
Patient self-management is a key element in the control of diabetes, and is one of the most challenging regimens of any chronic illness [8]. People with diabetes are asked to perform SMBG, manage multiple medications, maintain foot hygiene, adhere to diet and meal plans, and engage in exercise programs [9]. While for some insulin users SMBG is an important component of diabetes care, it poses a significant inconvenience/burden on the patient, in addition to the significant and well-documented economic costs [10–13].
In Canada, annual diabetes costs in 2006 ranged from a low of Canadian $5.7 million in Newfoundland and Labrador to a high of $109.4 million in Ontario. During that same year, the typical cost per blood glucose test strip ranged from $0.72 in Ontario to $0.89 in Newfoundland and Labrador [13]. As SMBG has gained acceptance as a key component of diabetes care around the world for specific insulin users, other country-specific studies have addressed cost and utilization [14–18]. Currently, information is sparse regarding the real-world frequency and actual expenditures associated with SMBG, as well as the impact of SMBG costs relative to the cost of insulin-related therapy. This analysis represents a novel examination of the real-world frequency of use and costs associated with SMBG as a part of insulin-based treatment costs in Canada.
The primary objective of this analysis is to evaluate the real-world utilization and costs of SMBG tests in Canada among insulin-treated diabetes patients during a 12-month follow-up period. A secondary objective is to investigate SMBG-test-related costs as a proportion of total diabetes-related pharmacy costs.
Methods
A retrospective database analysis was conducted using the IMS Brogan Inc. Drug Plan database to collect information on the real-world utilization and expenses attributed to SMBG in relation to a specific insulin regimen, and what the costs for SMBG specifically are when compared to other treatment costs.
The IMS Brogan Inc. Drug Plan database, based in Ottawa, Canada, is comprised of drug claims paid by a variety of private insurers. The database collects information on over 10 million Canadians with more than 100 million prescriptions annually from the private sector. About 34% of records come from Ontario, 28% from Quebec, 29% from Western Canada, and 9% from Atlantic Canada. Nationally, it is estimated that this database captures approximately 70% of private drug plan prescription activity.
There are two provincial drug plans that provide IMS Brogan with patient-level data, including insulin-treatment-related costs: Ontario and Quebec. All cost calculations consist of the acquisition cost (ingredient cost) as well as allowable mark-ups, dependent upon province and public/private plans. Dispensing fees are not included in the costs.
The Ontario Public Drug Plan (OPDP) covers approximately 2.5 million active claimants and pays for 115 million prescriptions annually. The OPDP claimant population is approximately 66% seniors (over age 65). About 33% of claimants receive benefits through social assistance (welfare), disability, or catastrophic illness programs. All of these claims are adjudicated online and transmitted monthly to IMS Brogan under a data services agreement with the Ontario government.
The Quebec Public Drug Plan, Régie de l’Assurance-Maladie de Québec (RAMQ), data is received directly from the plan administrator and includes all claims paid by the provincial plan in Quebec. All of the people of Quebec are eligible to enroll in this government-based universal healthcare plan regardless of their financial situation, although it is intended for people 65 years of age or older, welfare recipients, persons without a private healthcare plan, and children of persons covered by the public plan. This plan covers approximately 3.3 million beneficiaries or 2 million active claimants.
Inclusion Criteria
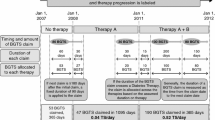
To be selected into the study population, subjects met each of the following inclusion criteria: they had at least two claims for insulin (any type, see Appendix Table 4) during the period from January 1, 2007 through December 31, 2009 (the index window or case-selection window). The date of the first such claim for a patient during the index window was considered his/her index date and set the patient’s insulin therapy subgroup. Patients were categorized into the following four, mutually exclusive, specific insulin therapy groups based on their index prescription: basal, bolus, premixed, basal–bolus. Basal and bolus patients were categorized as combination basal–bolus patients based on the presence of a second insulin type within 30 days of their initial (index) prescription.
Patients were continuously enrolled in their health plan for at least the most recent 6 months preceding their index date (their pre-index period) through at least 12 months following their index date (the follow-up period). The pre-index period was used for describing baseline characteristics, while the follow-up period was used for outcomes measurement. Study patients had to be persistent with insulin therapy throughout the 12-month follow-up period. Specifically, patients were considered persistent if they did not have a gap exceeding 90 days between two consecutive insulin claims at any time during the follow-up period. The patients also had to have at least one pharmacy claim for blood glucose testing strips during the 12-month follow-up period, to ensure SMBG utilization in the final cohort for analysis.
The selection of only those patients with evidence of SMBG testing, as well as the requirement of a 12-month follow-up period, were intended to ensure consistency with previous studies for comparative purposes, most notably that by Cameron et al. [17].
Exclusion Criteria
Patients were excluded from the study population if they met any of the following exclusion criteria: they were aged less than 4 years on their index date; they had prescriptions for more than one category of insulin (excluding basal–bolus combination as described above, see Appendix Table 4) within the first 30 days immediately following their index date (including the index date). Patients who had two different types of insulin at baseline (with the exception of basal–bolus combination) were also excluded, in order to avoid incorrectly attributing outcome behaviors to specific insulin groups (misclassification).
Measurements
All of the following measures were provided for the overall patient cohort, as well as the four specific subsets of insulin therapy type (basal, bolus, premixed, basal–bolus; see Appendix Table 4): demographic and clinical characteristics, blood glucose testing frequency and associated costs, and insulin and oral antidiabetic (OAD) medications costs (see Appendix Table 5).
Baseline Patient Demographic and Clinical Characteristics
The following patient demographic characteristics were measured as of the patient’s index date or during his/her 6-month pre-index period, except as noted.
-
Gender.
-
Age group (4–17, 18–34, 35–54, 55–64, or ≥65 years) as of their index date.
-
Type of patient, based on his/her insulin utilization.
-
Diabetes type proxy: (1) insulin only (type 1) or (2) insulin and OADs (type 2). The available data elements only allowed for differentiation based on the presence or absence of OADs.
-
Type of payer (private or public).
-
Province for private drug plans.
-
New or continuing insulin therapy, based on the presence of any insulin in the pre-index period.
-
Total drug utilization costs for all conditions, including all patient comorbidities, during the patient’s 6-month pre-index period, not including the index date, as a broad severity measure. For continuing patients, this measure includes diabetes-related costs.
Of note is that the IMS Brogan dataset does not contain diagnosis codes. Therefore, the overall burden of comorbid illnesses was inferred based on the total cost of claims for medications unrelated to diabetes.
Blood Glucose Testing
Patients’ frequency of blood glucose testing was monitored throughout their 12-month post-index follow-up period through claims for blood glucose test strips reimbursed by public or private drug plans. Visits to outpatient clinics or to laboratory/diagnostic centers for the blood glucose testing cannot be tracked using IMS Brogan data, so that utilization was not captured in this study.
Frequency of blood glucose testing is classified using descriptive statistics (mean, standard deviation, and median), and was stratified by the following variables: (1) patients’ insulin type, and (2) patients’ payer type (public or private).
SMBG and Diabetes-Related Pharmacy Costs
The total costs during the 12-month follow-up period were assessed, focusing on blood glucose testing strip costs, insulin therapy costs, and costs associated with OAD medications.
Cost of test strips and the drug costs were calculated by multiplying the number of units dispensed by the unit price. For the private drug plans, the wholesale price was used as a unit price, while for the public drug plans, the provincial formulary price was used as a unit price. The source of the unit prices is Delta PA. Delta PA is an online application that provides convenient access to current and historical drug prices. Sources of data include wholesale, Association québécoise des pharmaciens propriétaires (AQPP), and provincial formularies. All formulary prices are available on their respective websites.
Specific blood glucose testing costs were summarized to a total cost, as were costs specifically related to insulin and OAD therapy.
Statistical Analysis
The study population’s baseline demographic and clinical characteristics were described using frequency and percentage distributions for categorical variables and descriptive statistics (mean, standard deviation, and median) for continuous and categorical variables. Pearson’s χ2 test was used for statistical testing of categorical variables; Wilcoxon’s rank-sum test was used for statistical testing of continuous and ordinal variables. All data management and statistical analyses were completed using statistical analysis software (SAS Institute Inc., Cary, NC, USA; version 9.1.3).
Results
Demographics and Clinical Characteristics
Among 326,838 patients in the database with at least two claims for insulin between January 1, 2007 and December 31, 2009, 142,551 patients from both private and public payers satisfied all of the inclusion and exclusion criteria (Fig. 1). Categorization by initial insulin regimen (based on index date) resulted in the following insulin-specific subgroups for analysis: 45,003 on basal insulin, 15,525 on bolus insulin, 38,553 on premixed insulin, and 43,470 on basal–bolus combination insulin.
The largest percentage of patients in the study group fell in the 65+ age category (42.5%), followed by 35–54 (24.6%), 55–64 (22.0%), and ≤34 years of age (10.8%, Table 1). The proportion of women in the overall cohort was 48.9%, ranging from 47.0% in the basal insulin group to 50.5% in the bolus group. The majority of patients in the study group were from either Ontario (58.4%) or Quebec (30.5%), the most populous provinces in the country [19]. A higher proportion of patients on bolus only were new to insulin therapy, 60.1%, compared with patients on basal insulin (59.2%, P < 0.0001). Average total pre-index pharmacy costs ranged from $1,200 for bolus only to $1,431 for premixed, with an overall cohort average of $1,346.
Blood Glucose Testing
The overall mean number of pharmacy-based blood glucose tests in the 12-month follow-up period was 1,094 (3.0 tests per day), ranging from 890 tests in the premixed group to 1,413 in the bolus group (Fig. 2). Patients using premixed insulin had a significantly lower mean number of annual blood glucose tests (890) than did patients on a basal regimen (935, P < 0.0001). Patients on a basal regimen had significantly lower number of blood glucose tests than did patients using bolus insulin (1,413, P < 0.0001) and patients on a basal–bolus regimen (1,324, P < 0.0001).
SMBG and Diabetes-Related Pharmacy Costs
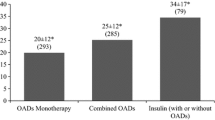
The overall cohort had an average annual pharmacy cost of $2,068 attributable to insulin treatments, blood glucose test strips, and OADs. The average cost for pharmacy-related blood glucose testing was $860 over the 1-year follow-up period (Table 2). With an overall mean utilization of pharmacy-based blood glucose testing of 1,094 strips per year, the average cost per testing strip was $0.79. Among patients in private and public drug plans, the mean utilization of pharmacy-based blood glucose testing was 899 and 1,211 strips per year, respectively, while the average cost per testing strip was $0.82 and $0.77, respectively. Annual blood glucose testing costs accounted for 37.7% of total insulin-related costs for the basal insulin group, compared with 52.8% for bolus, 41.4% for premixed, and 41.5% for basal–bolus (Table 3).
Compared with the basal insulin group, the premixed group had significantly lower average pharmacy costs over the 1-year period ($1,639 for premixed, $1,960 for basal, P < 0.0001). Both the bolus-only group ($2,106, P = 0.0001) and the basal–bolus group ($2,546, P < 0.0001) had significantly higher annual total diabetes-related pharmacy costs compared to the basal-only group.
Test Strip Utilization
Over the 1-year follow-up period, patients receiving basal–bolus insulin had 11.6 prescriptions for blood glucose testing strips, compared with 10.8 prescriptions for the bolus group, 9.0 for the basal group, and 8.0 for the premixed group (data not shown).
Discussion
SMBG constituted a large part of the treatment costs for insulin users, with testing strips ($860) totaling over 40% (41.6%) of the total diabetes-related pharmacy costs ($2,068), including insulin prescriptions. While the total costs of insulin use in a population with diabetes are well studied, as are the proportion of total costs associated with insulin, the economic aspects of SMBG for both payers and patients are not well understood, and differentially affect specific insulin subgroups. Most notably, among bolus insulin users, SMBG costs are 52.8% of the total diabetes-related costs ($1,112 of $2,106), possibly because of a higher use of insulin pumps in the category.
While this study may be unique in its focus on SMBG costs relative to diabetes-related costs, previous studies have measured outcomes with differing objectives. An economic survey to evaluate the direct costs among families of patients with type 1 diabetes found that the largest economic burden was due to SMBG expenses, which represented 53% of the total annual diabetes-related costs [20]. While the surveillance-based methodology of that study differs from this study’s approach, the similarity in the proportion of total costs attributable to SMBG is noteworthy. A 2010 study that also used the Canadian-based Brogan claims-level database found that, among insulin-only users, daily SMBG strip utilization averaged 2.76 in the Ontario Public Drug plan and 3.18 in private plans, similar to this study’s finding of 3.00 strips per patient per day [17]. Another study using the Norwegian Prescription Database found that 70% of the study’s diabetic population practiced SMBG, with an average of 1.7 strips per day [18]. One percent of patients used 10 or more strips per day, accounting for 8% of their total costs. Our analysis identified higher average strip utilization per day (3.00 strips) among all insulin type patients, though ours required a year of persistent insulin utilization, unlike the Norwegian analysis.
Limitations
A limitation of this study is that outpatient care costs, such as those for laboratory and radiology tests, and inpatient care events (such as the number and length of hospitalizations) could not be evaluated using this dataset. Diabetes-related complications were also not identified, due to the absence of diagnosis details within the database. Another limitation related to the lack of diagnosis codes is that classification by type of diabetes was not performed, other than differentiation by the presence or absence of OADs as a proxy. To the extent that insulin and OAD utilization is insufficient to accurately categorize patients by diabetes type, a degree of misclassification for the overall cohort as well as insulin-specific groups may have occurred.
Unique to the regional reimbursement structure within Canada, estimates of blood glucose test strip utilization and expenditures for special drug programs (e.g., the Nova Scotia Diabetes Assistance Program) were not included in the analysis. These special drug programs, however, represent a small proportion of publicly funded drug plans in Canada.
As this analysis was limited to an insured insulin-dependent population in Canada, the economic impact of SMBG in an uninsured population, as well as among patients using OAD medications rather than insulin, cannot be adequately assessed, and represents a suitable topic for future studies.
It should also be noted that a subset of patients in the bolus insulin regimen may have been using insulin pumps, and adjustments for pump users were not incorporated into the analysis. Additionally, to the extent that patients switch their insulin type during the follow-up period, a portion of patients in this study may potentially be misclassified according to therapy type, though such behavior is assumed to be nondifferential across subgroups.
Outpatient blood glucose testing may have been slightly underestimated as some glucose tests might have been incorporated into a claim for a test panel (e.g., comprehensive metabolic panel) and therefore not captured with codes for outpatient blood glucose test claims. Additionally, claims for blood glucose testing may have been overestimated due to the exclusion of patients with zero claims. Patients with zero claims may have been following guidelines for non-pump single-injection insulin patients, which suggest SMBG as an option rather than a requirement.
Conclusion
This study shows that SMBG constitutes over 40% of the diabetes-related pharmacy costs for insulin users, and as such warrants further study to recognize the impact on both patients and healthcare reimbursement systems.
References
Public Health Agency of Canada. Report from the National Diabetes Surveillance System: Diabetes in Canada. 2009. Available at: http://www.ndss.gc.ca. Accessed Sept 15 2011.
Canadian Diabetes Association. Clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2008;32:S1–215. Available at: http://www.diabetes.ca/files/cpg2008/cpg-2008.pdf. Accessed Dec 12 2011.
American Diabetes Association. Standards of medical care in diabetes—2007. Diabetes Care. 2007;30:s4–41.
American Diabetes Association. Standards of medical care in diabetes—2009. Diabetes Care. 2009;32:S13–61.
Jellinger PS, Davidson JA, Blonde L, et al. Road maps to achieve glycemic control in type 2 diabetes mellitus: AACE Diabetes Mellitus Clinical Practice Guidelines Task Force. Endocr Pract. 2007;13:260–8.
IDF Guideline Development Committee: Guideline for management of postmeal glucose. 2007.http://www.idf.org/webdata/docs/Guideline_PMG_Final.pdf. Accessed Dec 12 2011.
Canadian Diabetes Association. Clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32:1–215. Available at: http://www.diabetes.ca/files/cpg2008/cpg-2008.pdf. Accessed Sept 15 2011.
Delamater A. Improving patient adherence. Clin Diabetes. 2006;24:71–7.
Blonde L, Karter AJ. Current evidence regarding the value of self-monitored blood glucose testing. Am J Med. 2005;118:20s–6s.
Heinemann L, Boecker D. Lancing: quo vadis? J Diabetes Sci Technol. 2011;5:966–81.
Sandeep V, Hayward RA, Ronis DL, Hofer TP. Implications for the design of effective patient-centered treatment regimens. J Gen Intern Med. 2005;20:479–82.
Karter AJ. Role of self-monitoring of blood glucose in glycemic control. Endocr Pract. 2006;12:110–7.
Cameron C, Virani A, Dean H, Evans M, Dolovich L, Dahl M. Utilization and expenditure on blood glucose test strips in Canada. Can J Diabetes. 2010;34:34–40.
Davis WA, Bruce DG, Davis TM. Is self-monitoring of blood glucose appropriate for all type 2 diabetic patients? The Fremantle Diabetes Study. Diabetes Care. 2006;29:1764–70.
Pollack RF, Valentine WJ, Goodall G, Brandle M. Evaluating the cost-effectiveness of self-monitoring of blood glucose in type 2 diabetes on oral anti-diabetic agents. Swiss Med Weekly. 2010;25:1–10.
Kjome RL, Granas AG, Nerhus K, Roraas TH, Sandberg S. The prevalence of self-monitoring of blood glucose and costs of glucometer strips in a nationwide cohort. Diabetes Technol Ther. 2010;12:701–5.
Weber C, Kocher S, Neeser K, Bartaskova D. Impact of self-measurement of blood glucose on complications of type 2 diabetes: economic analysis from a Czech perspective. Curr Med Res Opin. 2010;26:289–96.
Neeser K, Weber C. Cost impact of self-measurement of blood glucose on complications of type 2 diabetes: the Spanish perspective. Diabetes Technol Ther. 2009;11:509–16.
Statistics Canada. Population Estimates. Population by year, province, territory. Available at: http://www40.statcan.gc.ca/l01/cst01/demo02a-eng.htm. Accessed Sept 15 2011.
Altamirano-Bustamante N, Islas-Ortega L, Robles-Valdes C, et al. Economic family burden of metabolic control in children and adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2008;21:1163–8.
Acknowledgments
IMS Consulting received consulting fees from Novo Nordisk for this study. Mr. Yeaw and Dr. Lee are employees of IMS Consulting Group; Wolden, Christensen, and Groleau are employees of Novo Nordisk. Mr. Yeaw is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. The authors thank Muhammad Mamdani, PharmD, MA, MPH, Director, Applied Health Research Center, St. Michael’s Hospital, Toronto, who assisted in the interpretation of the data and revision of the manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Yeaw, J., Lee, W.C., Wolden, M.L. et al. Cost of Self-Monitoring of Blood Glucose in Canada among Patients on an Insulin Regimen for Diabetes. Diabetes Ther 3, 7 (2012). https://doi.org/10.1007/s13300-012-0007-6
Received:
Published:
DOI: https://doi.org/10.1007/s13300-012-0007-6