Abstract
Background
Increasing rate of Caesarean sections and inadequate pain relief following Caesarean section is seen in almost all parts of the world. Transversus abdominis plane block is gaining popularity as a part of multimodal analgesia for post-operative pain relief following abdominal surgeries.
Aim
To compare bupivacaine and bupivacaine with dexmedetomidine in transversus abdominis plane block for pain relief after Caesarean section.
Method
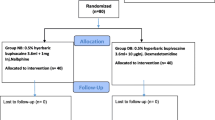
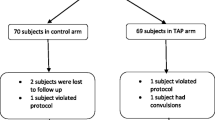
American Society of Anaesthesiologists I and II parturients with no comorbidities admitted for elective Caesarean section were included in the study. Thirty-five patients were in each study (with dex) and control (without dex) groups. At the end of Caesarean section done under spinal anaesthesia, transversus abdominis plane block was done bilaterally under ultrasound guidance using in-plane technique of needle insertion. 20 ml of 0.25% bupivacaine with 0.5 mcg/kg of dexmedetomidine in the study group and 20 ml of 0.25% bupivacaine in the control group were injected in the neurovascular plane.
Results
Eight patients from the study group and 15 from the control group were given opioids as rescue analgesia. The average time at which rescue analgesia was first sought was 14.25 and 7.73 h in the study and control groups, respectively. The P value of this difference was 0.0136 and was found to be statistically significant.
Conclusion
The addition of dexmedetomidine to bupivacaine in TAP block prolonged the duration of time at which first dose of rescue analgesia was sought and also reduced the total dose of opioid requirement in the first 24-h post-Caesarean section.


Similar content being viewed by others
References
Gibbons L, Belizán JM, Lauer JA, et al. World Health Report. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a Barrier to Universal Coverage (2010).
Vaishnavi S (vaishnavi.s.d@gmail.com)1, Chitra Grace A (chitragrace@yahoo.co.uk)2 and Muraleedharan VR (vrm@iitm.ac.in) 3 1. & 2. ICMR School of Public Health, National Institute of Epidemiology, Chennai, India 3. Indian Institute of Technology Madras, Chennai, India.Analysis of the extent and cost of caesarean section deliveries in Kerala and Tamil Nadu, India: Evidence from DLHS-3 survey.
Chou R, Gordon DB, de Leon-Casasola OA. Guidelines on the Management of Postoperative Pain Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–57.
Shahraki AD, Jabalameli M, Ghaedi S. Pain relief after cesarean section: oral methadone vs. intramuscular pethidine. J Res Med Sci. 2012;17(2):143–7.
Naaz S, Ozair E. Dexmedetomidine in current anaesthesia practice- a review. J Clin Diagn Res. 2014;8(10):GE01–4.
Kaur M, Singh PM. Current role of dexmedetomidine in clinical anesthesia and intensive care. Anesth Essays Res. 2011;5(2):128–33.
Siddiqui MR, Sajid MS, Uncles DR, et al. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth. 2011;23(1):7–14.
McDonnell JG, Curley G, Carney J, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106(1):186–91.
McDonnell JG, O’Donnell B, Curley G, et al. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104(1):193–7.
Aveline C, Le HH, Le RA, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106(3):380–6.
Almarakbi WA, Kaki AM. Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates post-operative pain relief among abdominal hysterectomy patients: a prospective randomized controlled trial. Saudi J Anaesth. 2014;8(2):161–6.
Lee AJ, Palte HD, Chehade JM, et al. Ultrasound-guided bilateral transversus abdominis plane blocks in conjunction with intrathecal morphine for postcesarean analgesia. J Clin Anesth. 2013;25(6):475–82.
Onishi Y, Kato R. Transverses abdominis plane block provides postoperative analgesic effects after cesarean section: additional analgesia to epidural morphine alone. J Obstet Gynaecol Res. 2013;39(9):1397–405.
Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesth. 2012;59(8):766–78.
Yu N, Long X, Lujan-Hernandez JR, et al. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014;15(14):121.
Jankovic Z. Transversus abdominis plane block: The Holy Grail of anaesthesia for (lower) abdominal surgery.Periodicum Biologorum Udc 57:61. 2009;111(2):203–8.
Singh R, Kumar N, Jain A, et al. Addition of clonidine to bupivacaine in transversus abdominis plane block prolongs postoperative analgesia after cesarean section. J Anaesthesiol Clin Pharmacol. 2016;32(4):501–4.
Toshniwal G, Soskin V. Ultrasound-guided transversus abdominis plane block in obese patients. Indian J Anaesth. 2012;56(1):104–5.
Tan TT, Teoh WH, Woo DC, et al. Sia ATA randomised trial of the analgesic efficacy of ultrasound-guided transversus abdominis plane block after caesarean delivery under general anaesthesia. Eur J Anaesthesiol. 2012;29(2):88–94.
Kanazi GE, Aouad MT, Abdallah FW, et al. The analgesic efficacy of subarachnoid morphine in comparison with ultrasound-guided transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2010;111(2):475–81.
Loane H, Preston R, Douglas MJ, et al. A randomized controlled trial comparing intrathecal morphine with transversus abdominis plane block for post-cesarean delivery analgesia. Int J Obstet Anesth. 2012;21(2):112–8.
Costello JF, Moore AR, Wieczorek PM, et al. The transversus abdominis plane block, when used as part of a multimodal regimen inclusive of intrathecal morphine, does not improve analgesia after cesarean delivery. Reg Anesth Pain Med. 2009;34(6):586–9.
Abdallah FW, Laffey JG, Halpern SH, et al. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111(5):721–35.
Rancourt MP, Albert NT, Côté M, et al. Posterior tibial nerve sensory blockade duration prolonged by adding dexmedetomidine to ropivacaine. Anesth Analg. 2012;115:958–62.
Esmaoglu A, Yegenoglu F, Akin A, et al. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111:1548–51.
Marhofer D, Kettner SC, Marhofer S, et al. Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: A volunteer study. Br J Anaesth. 2012;15:438–42.
Ammar AS, Mahmoud KM. Ultrasound-guided single injection infraclavicular brachial plexus block using bupivacaine alone or combined with dexmedetomidine for pain control in upper limb surgery: a prospective randomized controlled trial. Saudi J Anaesth. 2012;6:109–14.
Frassanito L, Pitoni S, Gonnella G, et al. Utility of ultrasound-guided transversus abdominis plane block for day-case inguinal hernia repair. Korean J Anesthesiol. 2017;70(1):46–51.
Erdoğan AD, Yıldırım AA, Karadoğan F, et al. Ultrasound-guided transversus abdominis plane block in patients undergoing open inguinal hernia repair: 0.125% bupivacaine provides similar analgesic effect compared to 0.25% bupivacaine. J Clin Anesth. 2016;28:41–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Ethical approval
Institutional ethical committee clearance was obtained. None of the patients in the study group had any adverse effect due to the addition of dexmedetomidine.
Additional information
Dr. A. Ramya Parameswari is a Consultant Anaesthesiologist at Sri Ramakrishna Hospital, Coimbatore.
Dr. Prabha Udayakumar is the Head of Department of Anaesthesia, Sri Ramakrishna Hospital, Coimbatore.
Rights and permissions
About this article
Cite this article
Ramya Parameswari, A., Udayakumar, P. Comparison of Efficacy of Bupivacaine with Dexmedetomidine Versus Bupivacaine Alone for Transversus Abdominis Plane Block for Post-operative Analgesia in Patients Undergoing Elective Caesarean Section. J Obstet Gynecol India 68, 98–103 (2018). https://doi.org/10.1007/s13224-017-0990-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-017-0990-7