Abstract
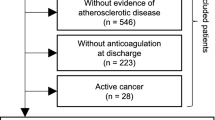
We investigated the effectiveness of adding antiplatelet (AP) to oral anticoagulant (OAC) treatment versus OAC treatment alone in patients with AIS with atrial fibrillation (AF) and significant large artery steno-occlusion (LASO). This study is a retrospective analysis of a nationwide, prospective, multicenter stroke registry between April 2008 and November 2017. Patients with acute (within 48 h of onset) and mild-to-moderate (NIHSS score ≤ 15) stroke with AF and concomitant LASO were identified. Antithrombotic regimens at discharge were categorized into OAC alone or OAC + AP. The primary outcome event was a composite of recurrent stroke, myocardial infarction, and all-cause mortality within 3 months of stroke. Among the 2553 patients (age, 73 ± 10 years; men, 50.4%), 78.8% were treated with OAC alone, and 21.2% were treated with OAC + AP. The primary outcome events were significantly more common in the OAC + AP group (6.7%) than the OAC alone group (4.3%) (p = 0.02). Weighted Cox proportional hazard analysis showed that OAC + AP increased the risk of 3-month primary outcome events compared with OAC alone (HR, 1.62 [1.06 to 2.46]). A potential interaction between the type of LASO and discharge antithrombotics was suggested (Pinteraction = 0.04); unlike in patients with complete occlusion (OAC + AP; HR, 2.00 [1.27–3.15]), OAC + AP was comparable with OAC alone for 3-month primary outcome in patients with moderate-to-severe stenosis (HR, 0.54 [0.17–1.70]). In conclusion, OAC + AP might increase the risk of 3-month outcome events compared with OAC alone in patients with AIS with AF and concomitant LASO. However, the effect of additional AP to OAC might differ according to LASO type.

Similar content being viewed by others
Availability of Data and Material
Data used in this study are available upon reasonable request following submission of a legitimate academic research proposal to be assessed by the CRCS-K steering committee.
References
Cardiogenic brain embolism. The second report of the cerebral embolism task force. Arch Neurol. 1989;46(7):727–43.
Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke. 2019;21(1):42–59. https://doi.org/10.5853/jos.2018.03125.
Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham heart study: a cohort study. Lancet. 2015;386(9989):154–62. https://doi.org/10.1016/S0140-6736(14)61774-8.
Wang JC, Bennett M. Aging and atherosclerosis: mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ Res. 2012;111(2):245–59. https://doi.org/10.1161/CIRCRESAHA.111.261388.
Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, Nam CM, et al. Increases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. 2011;42(4):930–4. https://doi.org/10.1161/STROKEAHA.110.602987.
Kamel H, Okin PM, Elkind MS, Iadecola C. Atrial fibrillation and mechanisms of stroke: time for a new model. Stroke. 2016;47(3):895–900. https://doi.org/10.1161/STROKEAHA.115.012004.
Lehtola H, Airaksinen KEJ, Hartikainen P, Hartikainen JEK, Palomaki A, Nuotio I, et al. Stroke recurrence in patients with atrial fibrillation: concomitant carotid artery stenosis doubles the risk. Eur J Neurol. 2017;24(5):719–25. https://doi.org/10.1111/ene.13280.
Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet. 1993;342(8882):1255–62.
Saxena R, Koudstaal P. Anticoagulants versus antiplatelet therapy for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischemic attack. Cochrane Database Syst Rev. 2004;4:CD000187. https://doi.org/10.1002/14651858.CD000187.pub2.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236. https://doi.org/10.1161/STR.0000000000000024.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962. https://doi.org/10.1093/eurheartj/ehw210.
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319–30. https://doi.org/10.1056/NEJMoa1709118.
Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015;17(1):38–53. https://doi.org/10.5853/jos.2015.17.1.38.
Kim BJ, Han MK, Park TH, Park SS, Lee KB, Lee BC, et al. Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. Int J Stroke. 2014;9(4):514–8. https://doi.org/10.1111/ijs.12199.
Rassen JA, Glynn RJ, Rothman KJ, Setoguchi S, Schneeweiss S. Applying propensity scores estimated in a full cohort to adjust for confounding in subgroup analyses. Pharmacoepidemiol Drug Saf. 2012;21(7):697–709. https://doi.org/10.1002/pds.2256.
Wein T, Lindsay MP, Cote R, Foley N, Berlingieri J, Bhogal S, et al. Canadian stroke best practice recommendations: secondary prevention of stroke, sixth edition practice guidelines, update 2017. Int J Stroke. 2018;13(4):420–43. https://doi.org/10.1177/1747493017743062.
Shah R, Hellkamp A, Lokhnygina Y, Becker RC, Berkowitz SD, Breithardt G, et al. Use of concomitant aspirin in patients with atrial fibrillation: findings from the ROCKET AF trial. Am Heart J. 2016;179:77–86. https://doi.org/10.1016/j.ahj.2016.05.019.
So CH, Eckman MH. Combined aspirin and anticoagulant therapy in patients with atrial fibrillation. J Thromb Thrombolysis. 2017;43(1):7–17. https://doi.org/10.1007/s11239-016-1425-5.
Hansen ML, Sorensen R, Clausen MT, Fog-Petersen ML, Raunso J, Gadsboll N, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170(16):1433–41. https://doi.org/10.1001/archinternmed.2010.271.
Kanter MC, Tegeler CH, Pearce LA, Weinberger J, Feinberg WM, Anderson DC, et al. Carotid stenosis in patients with atrial fibrillation. Prevalence, risk factors, and relationship to stroke in the stroke prevention in atrial fibrillation study. Arch Intern Med. 1994;154(12):1372–7.
Gibson CM, Mehran R, Bode C, Halperin J, Verheugt FW, Wildgoose P, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016;375(25):2423–34. https://doi.org/10.1056/NEJMoa1611594.
Cannon CP, Bhatt DL, Oldgren J, Lip GYH, Ellis SG, Kimura T, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017;377(16):1513–24. https://doi.org/10.1056/NEJMoa1708454.
Lopes RD, Heizer G, Aronson R, Vora AN, Massaro T, Mehran R, et al. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019;380(16):1509–24. https://doi.org/10.1056/NEJMoa1817083.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0.
Lee SR, Choi EK, Kwon S, Han KD, Jung JH, Cha MJ, et al. Effectiveness and safety of contemporary oral anticoagulants among Asians with nonvalvular atrial fibrillation. Stroke. 2019;50(8):2245–9. https://doi.org/10.1161/STROKEAHA.119.025536.
van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest. 2006;129(5):1155–66. https://doi.org/10.1378/chest.129.5.1155.
Funding
This was supported by a grant (2017ER620101#) by the Research of Korea Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Disclosures
H.-J.B is involved in the principal investigation, a member of the steering committee, and/or a site investigator of multicenter clinical trials or clinical studies sponsored by Otsuka Korea, Bayer, Boehringer Ingelheim, Handok Pharmaceutical Company, SK Chemicals, Pfizer, ESAI-Korea, Daewoong Pharmaceutical Co. Ltd., Daiichi Sankyo, AstraZeneca Korea, Dong-A Pharmaceutical, Yuhan Corporation, BMS Korea, Korean Drug Co., Ltd., Servier, Shire Korea Ltd., and Shin Poong Pharm. Co. Ltd.; served on the scientific advisory board for Amgen Asia Holding Limited; served as the consultant for Celltrion, Inc. and Korean Drug Co., Ltd.; and received lecture honoraria from Daiichi Sankyo Korea, Otsuka Korea, Esai Korea, Korean Drug Co., Ltd., and Shire Korea Ltd. (modest). PBG serves as a member of the ARRIVE Steering Committee for Bayer (modest).
Ethics Approval
The current study was approved by the local institutional review boards at all participating centers, including the Chonnam National University Hospital.
Consent to Participate
The requirement for a written informed consent from the study subjects was waived based on maintenance of study subject anonymity and minimal risk to the participants.
Consent to Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 439 kb)
Rights and permissions
About this article
Cite this article
Kim, JT., Lee, J.S., Kim, B.J. et al. Effectiveness of Adding Antiplatelets to Oral Anticoagulants in Patients with Acute Ischemic Stroke with Atrial Fibrillation and Concomitant Large Artery Steno-Occlusion. Transl. Stroke Res. 11, 1322–1331 (2020). https://doi.org/10.1007/s12975-020-00822-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-020-00822-z