Abstract
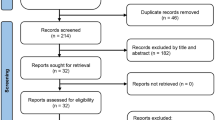
Post-operative delirium (POD) has been recognized as an independent risk factor for mortality. Recent studies suggest that POD is associated with higher mortality rates in patients undergoing transcatheter aortic valve replacement (TAVR). However, a systematic review and meta-analysis of the literature has not been performed. This study assessed the association between POD and TAVR by performing a systematic review and meta-analysis of the literature. We comprehensively searched the databases of MEDLINE and EMBASE from inception to April 2018. Included studies were prospective or retrospective cohort studies that compared mortality among patients undergoing TAVR both with and without POD. Data from each study were combined using the random-effects, generic inverse variance method of DerSimonian and Laird to calculate risk ratios and 95% confidence intervals. Seven studies consisting of 20,086 subjects undergoing TAVR (1517 with POD and 18,569 without POD) were included in this meta-analysis. POD demonstrated a trend towards higher all-cause mortality (pooled odd ratio 1.52, 95% confidence interval 0.98–2.37, p = 0.062, I2 = 72%). POD was associated with a significant increased long-term mortality (pooled odd ratio 2.11, 95% confidence interval 1.21–3.68, p = 0.009, I2 = 62.5%). POD was associated with an increased risk of long-term all-cause mortality in patients undergoing TAVR. Our study suggests POD could be a potential risk factor of mortality among patients undergoing TAVR. Further studies implementing preventative and treatment strategies against delirium and its effect on POD and its associated mortality are needed.




Similar content being viewed by others
Abbreviations
- AS:
-
Aortic stenosis
- CAM-ICU:
-
Confusion assessment method for the ICU
- CHART-DEL:
-
Chart abstraction for delirium during hospitalization
- CI:
-
Confidence interval
- DSM-IV:
-
Diagnostic and statistical manual of mental disorder IV
- EuroSCORE:
-
European system for cardiac operative risk evaluation
- ICD:
-
International statistical classification of disease and related health problem
- GA:
-
Generalized anesthesia
- LA:
-
Localized anesthesia
- NA:
-
Not available
- OR:
-
Odds ratio
- POD:
-
Post-operative delirium
- SAVR:
-
Surgical aortic valvular replacement
- STS:
-
Society of thoracic surgery
- TAVR:
-
Transcatheter aortic valvular replacement
References
Rodes-Cabau J. Transcatheter aortic valve implantation: current and future approaches. Nat Rev Cardiol. 2011;9(1):15–29.
Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597–607.
Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366(18):1686–95.
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98.
Mack MJ, Leon MB, Smith CR, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385(9986):2477–84.
Deeb GM, Reardon MJ, Chetcuti S, et al. 3-year outcomes in high-risk patients who underwent surgical or transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;67(22):2565–74.
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22.
Vijayakumar B, Elango P, Ganessan R. Post-operative delirium in elderly patients. Indian J Anaesth. 2014;58(3):251–6.
Smulter N, Lingehall HC, Gustafson Y, et al. Delirium after cardiac surgery: incidence and risk factors. Interact Cardiovasc Thorac Surg. 2013;17(5):790–6.
European Delirium A, American Delirium S. The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. 2014;12:141.
Martin BJ, Buth KJ, Arora RC, et al. Delirium: a cause for concern beyond the immediate postoperative period. Ann Thorac Surg. 2012;93(4):1114–20.
Kazmierski J, Kowman M, Banach M, et al. Incidence and predictors of delirium after cardiac surgery: results from The IPDACS Study. J Psychosom Res. 2010;69(2):179–85.
Martin BJ, Buth KJ, Arora RC, et al. Delirium as a predictor of sepsis in post-coronary artery bypass grafting patients: a retrospective cohort study. Crit Care. 2010;14(5):R171.
Bakker RC, Osse RJ, Tulen JH, et al. Preoperative and operative predictors of delirium after cardiac surgery in elderly patients. Eur J Cardio Thorac Surg. 2012;41(3):544–9.
Gottesman RF, Grega MA, Bailey MM, et al. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010;67(3):338–44.
Stroup DF, Berlin JA, Morton SC, Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Group, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–55.
Chizner MA, Pearle DL, deLeon AC Jr. The natural history of aortic stenosis in adults. Am Heart J. 1980;99(4):419–24.
Terre JA, George I, Smith CR. Pros and cons of transcatheter aortic valve implantation (TAVI). Ann Cardiothorac Surg. 2017;6(5):444–52.
Robinson TN, Eiseman B. Postoperative delirium in the elderly: diagnosis and management. Clin Interv Aging. 2008;3(2):351–5.
Schenning KJ, Deiner SG. Postoperative delirium in the geriatric patient. Anesthesiol Clin. 2015;33(3):505–16.
Plaschke K, Fichtenkamm P, Schramm C, et al. Early postoperative delirium after open-heart cardiac surgery is associated with decreased bispectral EEG and increased cortisol and interleukin-6. Intensive Care Med. 2010;36(12):2081–9.
Schoen J, Meyerrose J, Paarmann H, et al. Preoperative regional cerebral oxygen saturation is a predictor of postoperative delirium in on-pump cardiac surgery patients: a prospective observational trial. Crit Care. 2011;15(5):R218.
Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119(2):229–36.
Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58(4):643–9.
Abawi M, Pagnesi M, Agostoni P, et al. Postoperative delirium in individuals undergoing transcatheter aortic valve replacement: a systematic review and meta-analysis. J Am Geriatr Soc. 2018;66(12):2417–24.
Stachon P, Kaier K, Zirlik A, et al. Risk factors and outcome of postoperative delirium after transcatheter aortic valve replacement. Clin Res Cardiol. 2018;107(9):756–62.
Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64(5):402–6.
Genereux P, Cohen DJ, Williams MR, et al. Bleeding complications after surgical aortic valve replacement compared with transcatheter aortic valve replacement: insights from the PARTNER I trial (placement of aortic transcatheter valve). J Am Coll Cardiol. 2014;63(11):1100–9.
Athappan G, Patvardhan E, Tuzcu EM, et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol. 2013;61(15):1585–95.
Davis DH, Muniz-Terrera G, Keage HA, et al. Association of delirium with cognitive decline in late life: a neuropathologic study of 3 population-based cohort studies. JAMA Psychiatry. 2017;74(3):244–51.
An J, Li H, Tang Z, et al. cognitive impairment and risk of all-cause and cardiovascular disease mortality over 20-year follow-up: results from the BLSA. J Am Heart Assoc. 2018;7(15):e008252.
Perna L, Wahl HW, Mons U, et al. Cognitive impairment, all-cause and cause-specific mortality among non-demented older adults. Age Ageing. 2015;44(3):445–51.
Chandrasekhar J, Hibbert B, Ruel M, et al. Transfemoral vs non-transfemoral access for transcatheter aortic valve implantation: a systematic review and meta-analysis. Can J Cardiol. 2015;31(12):1427–38.
Sanders TB, Bowens FM, Pierce W, et al. The road to ICD-10-CM/PCS implementation: forecasting the transition for providers, payers, and other healthcare organizations. Perspect Health Inf Manag. 2012;9:1f.
Kurbasic I, Pandza H, Masic I, et al. The advantages and limitations of international classification of diseases, injuries and causes of death from aspect of existing health care system of bosnia and herzegovina. Acta Inf Med AIM. 2008;16(3):159–61.
Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312–8.
Bui LN, Pham VP, Shirkey BA, et al. Effect of delirium motoric subtypes on administrative documentation of delirium in the surgical intensive care unit. J Clin Monit Comput. 2017;31(3):631–40.
Thomas C, Kreisel SH, Oster P, et al. Diagnosing delirium in older hospitalized adults with dementia: adapting the confusion assessment method to international classification of diseases, tenth revision, diagnostic criteria. J Am Geriatr Soc. 2012;60(8):1471–7.
Villablanca PA, Mohananey D, Nikolic K, et al. Comparison of local versus general anesthesia in patients undergoing transcatheter aortic valve replacement: a meta-analysis. Catheter Cardiovasc Interv. 2018;91(2):330–42.
Attizzani GF, Patel SM, Dangas GD, et al. Comparison of local versus general anesthesia following transfemoral transcatheter self-expanding aortic valve implantation (from the transcatheter valve therapeutics registry). Am J Cardiol. 2019;123(3):419–25.
Bilotta F, Lauretta MP, Borozdina A, et al. Postoperative delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol. 2013;79(9):1066–76.
Chaput AJ, Bryson GL. Postoperative delirium: risk factors and management: continuing professional development. Can J Anaesth Journal canadien d’anesthesie. 2012;59(3):304–20.
Samim M, Hendrikse J, van der Worp HB, et al. Silent ischemic brain lesions after transcatheter aortic valve replacement: lesion distribution and predictors. Clin Res Cardiol. 2015;104(5):430–8.
Bokeriia LA, Golukhova EZ, Polunina AG. Postoperative delirium in cardiac operations: microembolic load is an important factor. Ann Thorac Surg. 2009;88(1):349–50 (author reply 350–341).
Reinsfelt B, Westerlind A, Ioanes D, et al. Transcranial Doppler microembolic signals and serum marker evidence of brain injury during transcatheter aortic valve implantation. Acta Anaesthesiol Scand. 2012;56(2):240–7.
Mach JR Jr, Dysken MW, Kuskowski M, et al. Serum anticholinergic activity in hospitalized older persons with delirium: a preliminary study. J Am Geriatr Soc. 1995;43(5):491–5.
Krzych LJ, Wybraniec MT, Krupka-Matuszczyk I, et al. Complex assessment of the incidence and risk factors of delirium in a large cohort of cardiac surgery patients: a single-center 6-year experience. Biomed Res Int. 2013;2013:835850.
Hshieh TT, Fong TG, Marcantonio ER, et al. Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol SerA Biol Sci Med Sci. 2008;63(7):764–72.
Van Mieghem NM, van Gils L, Ahmad H, et al. Filter-based cerebral embolic protection with transcatheter aortic valve implantation: the randomised MISTRAL-C trial. EuroIntervention. 2016;12(4):499–507.
Lansky AJ, Schofer J, Tchetche D, et al. A prospective randomized evaluation of the TriGuard HDH embolic DEFLECTion device during transcatheter aortic valve implantation: results from the DEFLECT III trial. Eur Heart J. 2015;36(31):2070–8.
Elie M, Cole MG, Primeau FJ, et al. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998;13(3):204–12.
Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852–7.
Funding
None.
Author information
Authors and Affiliations
Contributions
NP: conception design, data interpretation, and draft manuscript, corresponding. RM: data acquisition and draft manuscript. JK: data acquisition and draft manuscript. CK: data acquisition and data interpretation. MAM: data interpretation and manuscript revision. WC: data interpretation and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prasitlumkum, N., Mekritthikrai, R., Kewcharoen, J. et al. Delirium is associated with higher mortality in transcatheter aortic valve replacement: systemic review and meta-analysis. Cardiovasc Interv and Ther 35, 168–176 (2020). https://doi.org/10.1007/s12928-019-00592-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-019-00592-y