Abstract
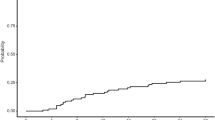
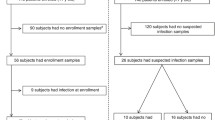
HLA-DR is a key marker of leukocyte activation, which suppression determines the effectiveness of immune response and prognosis in neonatal sepsis (NS). The aim of this study was to evaluate the HLA-DR expression on lymphocytes and monocytes in the peripheral blood of neonates with sepsis. The study involved 21 neonates with sepsis and 10 healthy neonates born during the study period. Bacteremia was detected in five cases (24%). The most frequent pathogens found were Klebsiella pneumoniae (n = 2) and Staphylococcus aureus (n = 2) followed by Streptococcus agalactae (n = 1). NS was associated with pneumonia (n = 17), meningitis (n = 3), and necrotizing enterocolitis (n = 1). The onset of NS was accompanied with high blood monocyte activity which ranged from 96 to 100%. Blood CD3+ lymphocyte population and CD4+ and CD8+ lymphocyte subset levels were decreased, with their median values being 1.7, 2.2, and 2.4 times lower than those in the control group, respectively (р = 0.005, р = 0.0002, р = 0.003). The HLA-DR expression on CD3+ lymphocytes, as well as on CD4+ and CD8+ lymphocyte subsets, was extremely low ranging from 0.1 to 7% both in the onset of the disease and in a week after admission to a hospital. Absolute counts of activated CD4+ and CD8+ lymphocyte subsets were significantly lower on the disease first days as compared to the control group (р = 0.02 and р = 0.003, respectively). These results demonstrate adaptive immunity to be non-effective in neonates with sepsis. Low expression of HLA-DR on CD3 lymphocytes as well as on CD4 and CD8 lymphocyte subsets is a reason for immunostimulating therapy.
Similar content being viewed by others
References
Liu, L., Oza, S., Hogan, D., et al. (2016). Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet, 388(10063), 3027–3035.
Camacho-Gonzales, A., Spearman, P. W., & Stoll, B. J. (2013). Neonatal infectious diseases: evaluation of neonatal sepsis. Pediatric Clinics of North America, 60, 367–389.
Wynn, J. L. (2016). Defining neonatal sepsis. Current Opinion in Pediatrics, 28, 135–140.
Hotchkiss, R. S., Coopersmith, G. M., McDunn, J. E., & Ferguson, T. A. (2009). Nature Medicine, 15(5), 496–497.
Boomer, J. S., Green, J. M., & Hotchkiss, R. S. (2014). The changing immune system in sepsis: is individualized immune-modulatory therapy the answer? Virulence, 5(1), 45–56.
Reinhart, K., Bauer, M., Riedemann, N. C., et al. (2012). New approaches to sepsis: molecular diagnostics and biomarkers. Clinical Microbiology Reviews, 25(4), 609–634.
Bhandari, V. (2014). Effective biomarkers for diagnosis of neonatal Sepsis. Journal of the Pediatric Infectious Diseases Society, 3(3), 234–245.
Shah, B. A., & Padbury, J. F. (2014). Neonatal sepsis: an old problem with new insights. Virulence, 54, 449–457.
Venet, F., Lepape, A., & Monneret, G. (2011). Clinical review: flow cytometry perspectives in the ICU—from diagnosis of infection to monitoring of injury-induced immune dysfunctions. Critical Care, 15, 231.
Gille, C., & Orlikowsky, T. W. (2007). Flow cytometric methods in the detection of neonatal infection. Transfusion Medicine and Hemotherapy, 34, 157–163.
Monneret, G., & Venet, F. (2014). Monocyte HLA-DR in sepsis: shall we stop following the flow? Critical Care, 18, 102. https://doi.org/10.1186/cc13179.
Zhuang, Y., Peng, H., Chen, Y., et al. (2017). Dynamic monitoring of monocyte HLA-DR expression for the diagnosis, prognosis, and prediction of sepsis. Frontiers in Bioscience Landmark, 22, 1344–1354.
Monneret, G. (2005). How to identify systemic sepsis-induced immunoparalysis. Advances in Sepsis, 4(2), 42–49.
Wu, J.-F., Ma, J., Chen, J., et al. (2011). Changes of monocyte human leukocyte antigen-DR expression as a reliable predictor of mortality in severe sepsis. Critical Care, 15, R220.
Rimmele, T., Payen, D., Cantaluppi, V., et al. (2016). Immune cell phenotype and function in sepsis. Shock, 45(3), 282–291.
Litvinova, L. S., Gutsol, A. A., Sokhonevich, N. A., et al. (2014). Basic surface markers of functional activity T-lymphocytes. Medical Immunology (Russia), 16(1), 7–26.
Rossi, P., Botgros, R., Tibby S. et al. (2010). Report on the Expert Meeting on Neonatal and Paediatric Sepsis. London: European Medicines Agency, http://www.ema.europa.eu/docs/enGB/documentlibrary/Report/2010/12/WC500100199.pdf.
Rundolph, A. G., & Mc Culloh, R. J. (2014). Pediatric sepsis. Virulence, 5(1), 179–189.
Hotchkiss, R. S., & Karl, I. E. (2003). The pathophysiology and treatment of sepsis. The New England Journal of Medicine, 348(2), 138–150.
Perez, A., Bellon, J. M., Gurbindo, M. D., et al. (2010). Impairment of stimulation ability of very-preterm neonatal monocytes in response to lipopolysaccharide. Human Immunology, 71, 151–157.
Frazier, W. J., & Hall, M. W. (2008). Immunoparalysis and adverse outcomes from critical illness. Pediatric Clinics of North America, 55, 647–668.
Monneret, G., Elmenkouri, N., Bohe, J., et al. (2002). Analytical requirements for measuring monocytic HLA-DR by flow cytometry. Clinical Chemistry, 48, 1589–1592.
Wolk, K., Kunz, S., Crompton, N. E., et al. (2003). Multiple mechanisms of reduced major histocompatibility complex class II expression in endotoxin tolerance. The Journal of Biological Chemistry, 278(20), 18030–18036.
Monneret, G., Lepape, A., Voirin, N., et al. (2006). Persisting low monocyte human leukocyte antigen-DR expression predicts mortality in septic shock. Intensive Care Medicine, 32(8), 1175–1183.
Drewry, A. M., Ablordeppey, E. A., Murray, E. T., et al. (2016). Comparison of monocyte human leukocyte antigen-DR expression and stimulated tumor necrosis factor alpha production as outcome predictors in severe sepsis: a prospective observational study. Critical Care, 20, 334.
Monserrat, J., de Pablo, R., Diaz-Martín, D., et al. (2013). Early alterations of B cells in patients with septic shock. Critical Care, 17(3), R105.
Capasso, L., Borrelli, A. C., Cerullo, J., et al. (2015). Role of immunoglobulins in neonatal sepsis. Translational Medicine, 11(5), 28–33.
Hotchkiss, R. S., Osmon, S. B., Chang, K. C., et al. (2005). Accelerated lymphocyte death in sepsis occurs by both the death receptor and mitochondrial pathways. The Journal of Immunology, 174, 5110–5118.
Khaertynov Kh., S., Boichuk, S. V., Anohin, V. A., et al. (2014). Activity rates of apoptosis of lymphocytes in children with neonatal sepsis. Geny i kletki, 9(3), 267–271.
Khaertynov Kh., S., Anohin, V. A., Mustafin, I. G., et al. (2015). Specific features of immunity in neonatal infants with localized and generalized bacterial infections. Russian Bulletin of Perinatology and Pediatrics, 5, 168–173.
Boomer, J. S., To, K., Chang, K. C., et al. (2011). Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA, 306, 2594–2605.
Toti, P., De Felice, C., Occhini, R., et al. (2004). Spleen depletion in neonatal sepsis and chorioamnionitis. American Journal of Clinical Pathology, 122, 765–771.
Felmet, K. A., Hall, M. W., Clark, R. S., et al. (2005). Prolonged lymphopenia, lymphoid depletion, and hypoprolactinemia in children with nosocomial sepsis and multiple organ failure. Journal of Immunology, 174, 3765–3772.
Cabrera-Perez, J., Condotta, S. A., Badovinac, V. P., et al. (2014). Impact of sepsis on CD4 T cell immunity. Journal of Leukocyte Biology, 96(5), 767–777.
Wilson, C. B., Rowell, E., & Sekimata, M. (2009). Epigenetic control of T-helper cell differentiation. Nature Reviews Immunology, 9, 91–105.
Boomer, J. C., Shuherk-Shaffer, J., Hotchkiss, R. S., et al. (2012). A prospective analysis of lymphocytes phenotype and function over the course of acute sepsis. Critical Care, 16, R112.
Wesche, D. E., Lomas-Neira, J. L., Perl, M., et al. (2005). Leukocyte apoptosis and its significance in sepsis and shock. Journal of Leukocyte Biology, 78, 325–337.
Venet, F., Foray, A.-P., Villars-Mechin, A., et al. (2012). IL-7 restores lymphocytes function in septic patients. Journal of Immunology, 189(10), 5073–5081.
Holub, M., Kluckova, Z., Beneda, B., et al. (2000). Changes in lymphocyte subpopulations and CD3+/DR+ expression in sepsis. Clinical Microbiology and Infection, 6, 657–660.
Delano, M. J., & Ward, P. A. (2016). Sepsis-induced immune dysfunction: can immune therapies reduce mortality? The Journal of Clinical Investigation, 126(1), 23–31.
Walker, J. C., Smolders, M. A., Gemen, E. F., et al. (2011). Development of lymphocyte subpopulations in preterm infants. Scandinavian Journal of Immunology, 73, 53–58.
Correa-Rocha, R., Perez, A., Lorente, R., et al. (2012). Preterm neonates show marked leukopenia and lymphopenia that are associated with increased regulatory T-cell values and diminished IL-7. Pediatric Research, 71(5), 590–597.
Funding
This study was supported by the Russian Government Program of Competitive Growth of the Kazan Federal University. Albert A. Rizvanov was supported by the state assignment 20.5175.2017/6.7 of the Ministry of Education and Science of the Russian Federation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Ethics Committee of the City Children’s Hospital approved this study, and a written informed consent was obtained from the parents in accordance with the principles authorized under this protocol (the Federal Law N323-FL dated on 21.11. 2011 “On Protection of Health of the Citizens in the Russian Federation”).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Khaertynov, K.S., Anokhin, V.A., Mustafin, I.G. et al. Changes in HLA-DR Expression on Monocytes and Lymphocytes in Neonatal Sepsis. BioNanoSci. 8, 647–653 (2018). https://doi.org/10.1007/s12668-018-0519-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-018-0519-2