Abstract
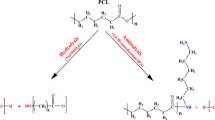
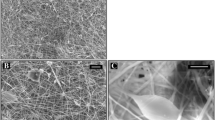
Three dimensional nanofiber materials made of poly-L-lactic acid (PLLA) and produced by electrospinning are commonly used in regenerative medicine and as a base for drug delivery systems. Surface modification of such materials allows manipulating their chemical, physical, and biological properties. Previously, our group reported a number of modification strategies for thin PLLA films, based on the “solvent/non-solvent” technique. Most biologically active agents may not be adsorbed on the surface of PLLA. Proposed treatment allows partially dissolving the polymer surface in order to adsorb biologically active molecules or linkers. The aim of this work was to investigate the influence of solvent/non-solvent mixture composition on the morphology and crystal structure of the electrospun PLLA scaffolds and to select the solvent system for further scaffolds modification in order to impart them biological activity. PLLA scaffolds were treated with mixtures of toluene and ethanol in different compositions. By means of scanning electron microscopy, it was shown that solvent/non-solvent treatment had no critical effect on the morphology of the scaffolds. The results of X-ray diffraction analysis revealed that treatment of the scaffolds with investigated solvent systems did not lead to the formation of the additional phases and the size of the polymer crystallites as well. Thus, selected solvent system will be used for modification of the PLLA electrospun nanofiber material for biomedical application.




Similar content being viewed by others
References
Costa, R. G. F., Brichi, G. S., Ribeiro, C., & Mattoso, L. H. C. (2016). Nanocomposite fibers of poly(lactic acid)/titanium dioxide prepared by solution blow spinning. Polymer Bulletin, 73, 2973–2985 1–13. doi:10.1007/s00289-016-1635-1.
Karchin, A., Simonovsky, F. I., Ratner, B. D., & Sanders, J. E. (2011). Melt electrospinning of biodegradable polyurethane scaffolds. Acta Biomaterialia, 7(9), 3277–3284. doi:10.1016/j.actbio.2011.05.017.
Wiebe, J., Dörr, O., Bauer, T., Liebetrau, C., Boeder, N., Möllmann, H., … Nef, H. M. (2016). Everolimus-eluting bioresorbable scaffold implantation for the treatment of bifurcation lesions—implications from early clinical experience during daily practice. Cardiovascular Revascularization Medicine doi:10.1016/j.carrev.2016.03.011.
Francois, E., Dorcemus, D., & Nukavarapu, S. (2015). Biomaterials and scaffolds for musculoskeletal tissue engineering. Regenerative engineering of musculoskeletal tissues and interfaces. Elsevier Ltd. doi:10.1016/B978-1-78242-301-0.00001-X.
Barbarash, L. S., Bolbasov, E. N., Antonova, L. V., Matveeva, V. G., Velikanova, E. a., Shesterikov, E. V., … Tverdokhlebov, S. I. (2016). Surface modification of poly-ε-caprolactone electrospun fibrous scaffolds using plasma discharge with sputter deposition of a titanium target. Materials Letters, 171, 87–90. doi:10.1016/j.matlet.2016.02.062.
Yang, F., Wolke, J. G. C., & Jansen, J. A. (2008). Biomimetic calcium phosphate coating on electrospun poly(ε-caprolactone) scaffolds for bone tissue engineering. Chemical Engineering Journal, 137(1), 154–161. doi:10.1016/j.cej.2007.07.076.
García-García, J. M., Quijada-Garrido, I., López, L., París, R., Núñez-López, M. T., De La Peña Zarzuelo, E., & Garrido, L. (2013). The surface modification of poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) copolymers to improve the attachment of urothelial cells. Materials Science and Engineering C, 33(1), 362–369. doi:10.1016/j.msec.2012.08.052.
Ghasemi-Mobarakeh, L., Prabhakaran, M. P., Morshed, M., Nasr-Esfahani, M. H., & Ramakrishna, S. (2010). Bio-functionalized PCL nanofibrous scaffolds for nerve tissue engineering. Materials Science and Engineering C, 30(8), 1129–1136. doi:10.1016/j.msec.2010.06.004.
Rasal, R. M., Janorkar, A. V., & Hirt, D. E. (2010). Poly(lactic acid) modifications. Progress in Polymer Science, 35(3), 338–356. doi:10.1016/j.progpolymsci.2009.12.003.
Gradus-Pizlo, I., Wilensky, R. L., March, K. L., Fineberg, N., Michaels, M., Sandusky, G. E., & Hathaway, D. R. (1995). Local delivery of biodegradable microparticles containing colchicine or a colchicine analogue: effects on restenosis and implications for catheter-based drug delivery. Journal of the American College of Cardiology, 26(6), 1549–1557. doi:10.1016/0735-1097(95)00345-2.
Michael Bünger, C., Grabow, N., Sternberg, K., Kröger, C., Ketner, L., Schmitz, K. P., … Schareck, W. (2007). Sirolimus-eluting biodegradable poly-l-lactide stent for peripheral vascular application: a preliminary study in porcine carotid arteries. Journal of Surgical Research, 139(1), 77–82. doi:10.1016/j.jss.2006.07.035.
Uhrich, K. E., & Abdelhamid, D. (2015). Biodegradable and bioerodible polymers for medical applications. Biosynthetic Polymers for Medical Applications. Elsevier Ltd. doi:10.1016/B978-1-78242-105-4.00003-1.
Alexander, H. (n.d.). Biological response of intramedullary bone to poly-L-lactic acid.
Stankevich, K. S., Gudima, A., Filimonov, V. D., Klüter, H., Mamontova, E. M., Tverdokhlebov, S. I., & Kzhyshkowska, J. (2015). Surface modification of biomaterials based on high-molecular polylactic acid and their effect on inflammatory reactions of primary human monocyte-derived macrophages: Perspective for personalized therapy. Materials Science and Engineering C, 51, 117–126. doi:10.1016/j.msec.2015.02.047.
He, L., Zhang, Y., Zeng, X., Quan, D., Liao, S., Zeng, Y., … Ramakrishna, S. (2009). Fabrication and characterization of poly(l-lactic acid) 3D nanofibrous scaffolds with controlled architecture by liquid-liquid phase separation from a ternary polymer-solvent system. Polymer, 50(16), 4128–4138. doi:10.1016/j.polymer.2009.06.025.
Gualandi, C., Govoni, M., Foroni, L., Valente, S., Bianchi, M., Giordano, E., … Focarete, M. L. (2012). Ethanol disinfection affects physical properties and cell response of electrospun poly(l-lactic acid) scaffolds. European Polymer Journal, 48(12), 2008–2018. doi:10.1016/j.eurpolymj.2012.09.016.
Zhang, K., Zheng, H., Liang, S., & Gao, C. (2016). Aligned PLLA nanofibrous scaffolds coated with graphene oxide for promoting neural cell growth. Acta Biomaterialia, 37, 131–142. doi:10.1016/j.actbio.2016.04.008.
Park, H., Lee, K. Y., Lee, S. J., Park, K. E., & Park, W. H. (2007). Plasma-treated poly(lactic-co-glycolic acid) nanofibers for tissue engineering. Macromolecular Research, 15(3), 238–243. doi:10.1007/BF03218782.
Acknowledgements
This research was funded by Russian Science Foundation (project No 16-13-10239) and performed in Tomsk Polytechnic University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goreninskii, S.I., Stankevich, K.S., Bolbasov, E.N. et al. Surface Modification of PLLA Electrospun Nanofiber Materials for Biomedical Applications. BioNanoSci. 8, 67–71 (2018). https://doi.org/10.1007/s12668-017-0422-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-017-0422-2