Abstract
Background
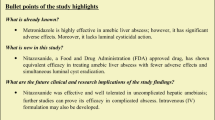
Metronidazole is a drug of choice for amebic liver abscess (ALA), but has long course and significant side effects. Thus, drugs like tinidazole with a better tolerability record need evaluation.
Methods
We conducted a randomized controlled trial at the Department of Gastroenterology, SMS Hospital, Jaipur, India. One hundred and fifty admitted patients were randomized into two treatment groups, metronidazole (group M, n = 75) and tinidazole (group T, n = 75). Patients were observed for clinical response, laboratory parameters, imaging, and side effects. Early clinical response (ECR) was defined as the absence of fever and abdominal pain within 72 h of treatment. Symptomatic clinical response (SCR) was defined as the absence of fever and abdominal pain irrespective of duration of treatment required. Follow up was done at 1, 3, and 6 months.
Results
ECR was 62.3% in group T vs. 37.7% in group M (p = 0.02). SCR was shorter in group T than group M (3.29 ± 1.61 days vs. 5.67 ± 2.93, p ≤ 0.001). Mean residual volume at the end of 1 month was lower in group T (130.7 ± 108.1 vs. 184.7 ± 143.3 mL, p = 0.01) and no significant difference was seen at 3 and 6 months. Tinidazole was better tolerated with fewer side effects. Low socioeconomic status, baseline abscess volume > 500 mL, hypoalbuminemia, pleural effusion, and history of ethanol use were associated with a late clinical response on univariate analysis of which low socioeconomic status was the only associated factor.
Conclusion
Tinidazole, as compared to metronidazole, has early clinical response, shorter treatment course, favorable rate of recovery, and high tolerability; thus, tinidazole can be preferred over metronidazole in ALA.

Similar content being viewed by others
References
Rajagopalan S, Langer V. Symposium hepatic abscesses. Med J Armed Forces India. 2012;68:271–5.
Sharma MP, Ahuja V. Amoebic liver abscess. JIACM. 2003;4:107–11.
Monro AM. Blood levels of chemotherapeutic drugs and the pharmacokinetics of tinidazole and metronidazole. Curr Med Res Opin. 1974;2:130–7.
Mathur SN, Itigi A, Knshnaveni, Rai V. Tinidazole and metronidazole in the treatment of amoebic liver abscess. J Int Med Res. 1973;1:429–33.
Siddiqui MNA, Ahad MA, Ekram ARMS, Islam QT, Hoque MA, Masum QAAI. Clinico-pathological profile of liver abscess in a teaching hospital. TAJ. 2008;21:44–9.
Stanley SL Jr. Amoebiasis. Lancet. 2003;361:1025–34.
Li E, Stanley SL Jr. Amebiasis. Gastroenterol Clin N Am. 1996;25:471–92.
Chan RT, Friedman LS. Amebic liver abscess. In: Feldman M, Friedman LS, Brandt LJ, Eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 8th ed. Philadelphia: Saunders; 2006. p. 1749–53.
Dias Granado’s CA, Duffus WA, Duffin S, Albrecht H. Parasitic diseases of the liver. In: David Zakim D, Boyer TD, Eds. Hepatology: A Textbook of Liver Disease. 4th ed. Philadelphia: Saunders; 2003. p. 1073–82.
Seeto RK, Rockey D. Amebic liver abscess: epidemiology, clinical features, and outcome. West J Med. 1999;170:104–9.
Sharma MP, Ahuja V. Amoebic liver abscess: clinician’s perspective. Bombay Hosp J. 1997;39:615–9.
Bakshi JS, Ghaira JN, Nanivedekar AS. How does tinidazole compare with metronidazole? A summary report of Indian trials in amoebiasis and giardiasis. Drugs. 1978;15 Suppl 1:33–42.
Scragg JN, Proctor EM. Tinidazole in treatment of amoebic liver abscess in children. Arch Dis Child. 1977;52:408–10.
Hatchuel W. Tinidazole for the treatment of amoebic liver abscess. S Afr Med J. 1975;49:1879–81.
Sharma MP, Dasarathy S, Sushma S, Verma N. Long term follow-up of amebic liver abscess: clinical and ultrasound patterns of resolution. Trop Gastroenterol. 1995;16:24–8.
Sheen IS, Chien CS, Lin DY, Liaw YF. Resolution of liver abscesses: comparison of pyogenic and amebic liver abscesses. Am J Trop Med Hyg. 1989;40:384–9.
Sharma MP, Dasarathy S, Verma N, Sushma S, Shukla DK. Prognostic markers in amebic liver abscess: a prospective study. Am J Gastroenterol. 1996;91:2584–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SP, GKG, SJW, and SN declare that they have no conflict of interest.
Ethics statement
The study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com. The study protocol was approved by the institutional review board and ethics committee.
Rights and permissions
About this article
Cite this article
Pandey, S., Gupta, G.K., Wanjari, S.J. et al. Comparative study of tinidazole versus metronidazole in treatment of amebic liver abscess: A randomized control trial. Indian J Gastroenterol 37, 196–201 (2018). https://doi.org/10.1007/s12664-018-0848-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-018-0848-7