Abstract
Purpose
Periprosthetic joint infection is a serious complication of total knee arthroplasty. Though there are many factors that might increase its risk, the use of propofol for maintaining general anesthesia could theoretically increase the incidence of infection because of its lipid component that supports bacterial growth. Nevertheless, the relationship between anesthetic maintenance agents and the occurrence of periprosthetic joint infection remains uncertain. The purpose of this study was to compare the incidence of suspected early-onset periprosthetic joint infection between patients undergoing total knee arthroplasty under propofol vs sevoflurane anesthesia.
Methods
We conducted a retrospective cohort study of patients in the national inpatient Diagnosis Procedure Combination database in Japan who underwent total knee arthroplasty. Suspected periprosthetic joint infection was surrogately defined as the need for arthrocentesis or debridement within 30 days of surgery. Propensity score matching was performed between patients who received either propofol or sevoflurane for anesthetic maintenance to determine the proportion of those with infection.
Results
Eligible patients (n = 21,899) were categorized into either the propofol (n = 7,439) or sevoflurane (n = 14,460) groups. In the 5,140 propensity-matched patient pairs, there was no significant difference in the proportion of arthrocentesis or debridement [1.3% propofol vs 1.7% sevoflurane; respectively (relative risk, 0.76; 95% CI, 0.55 to 1.04; P = 0.10)] between the groups. The mean (SD) length of stay in the propofol group was significantly longer than in the sevoflurane group [32.5 (18.4) days vs 31.4 (14.4) days, respectively; mean difference, 1.1; 95% CI, 0.5 to 1.8; P < 0.001].
Conclusion
Propensity score analysis suggested no significant association between the choice of anesthetic maintenance agent and the occurrence of suspected early-onset periprosthetic joint infection in patients undergoing total knee arthroplasty.
Résumé
Objectif
L’infection articulaire périprothétique est une complication grave de l’arthroplastie totale de genou. De nombreux facteurs peuvent accroître le risque, mais l’utilisation de propofol pour l’entretien de l’anesthésie générale pourrait, en théorie, augmenter l’incidence des infections en raison de sa composante lipidique qui pourrait favoriser la croissance bactérienne. Néanmoins, l’association entre les agents de maintien de l’anesthésie et la survenue d’une infection articulaire périprothétique est incertaine. L’objectif de cette étude était de comparer l’incidence d’une infection articulaire périprothétique précoce suspectée après arthroplastie totale de genou chez des patients ayant reçu une anesthésie par propofol ou sévoflurane.
Méthodes
Nous avons étudié une cohorte rétrospective de patients tirés de la base de données combinée des procédures diagnostiques chez des patients hospitalisés au Japon après arthroplastie totale de genou. Une infection articulaire périprothétique suspectée était définie par le besoin d’une arthrocentèse ou d’un débridement dans les 30 jours suivant l’intervention initiale. Le score de propension correspondant a été calculé entre les patients qui avaient reçu du propofol ou du sévoflurane pour l’entretien de l’anesthésie afin de déterminer le pourcentage de patients ayant une infection.
Résultats
Les patients admissibles (n = 21 899) ont été classés dans le groupe propofol (n = 7 439) ou dans le groupe sévoflurane (n = 14 460). Parmi les 5 140 paires de patients appariés par propension, il n’y a pas eu de différence significative entre les proportions d’arthrocentèses ou de débridement (propofol 1,3 % contre sévoflurane 1,7 %; [risque relatif, 0,76; IC à 95 %, 0,55 à 1,04; P = 0,10]) entre les groupes. La durée moyenne (ET) de l’hospitalisation (incluant la physiothérapie) dans le groupe propofol a été significativement supérieure à celle du groupe sévoflurane (respectivement, 32,5 [18,4] jours contre 31,4 [14,4] jours; différence des moyennes, 1,1; IC à 95 %, 00,5 à 01,8; P < 0,001).
Conclusion
L’analyse du score de propension porte à croire qu’il n’existe pas d’association significative entre l’anesthésique choisi pour l’entretien de l’anesthésie et la survenue d’une infection articulaire périprothétique suspectée, d’apparition précoce, chez les patients ayant subi une arthroplastie totale de genou.
Similar content being viewed by others
Periprosthetic joint infection, which occurs in approximately 0.5-2% of patients after total knee arthroplasty (TKA),1,2,3 is a serious postoperative complication associated with increased prolonged hospitalization, economic cost, and mortality.4,5 Many risk factors are involved in periprosthetic joint infection, including patient characteristics (e.g., diabetes and smoking history), hospital function,6 and potentially even anesthetic management.7 Treatment of periprosthetic joint infection is challenging as it can recur despite antibiotic therapy and, in some cases, requires removal of the prosthesis.8
The association between the anesthetic maintenance agent and the occurrence of surgical site infection (SSI) remains uncertain. A previous nationwide study in Taiwan showed that TKA and total hip arthroplasty (THA) under general anesthesia were both associated with a higher occurrence of SSI than those under regional anesthesia.9 Propofol and sevoflurane are commonly used for the maintenance of general anesthesia; however, propofol may increase the risk of infection because of its lipid component, which can support bacterial growth when contaminated.10,11 Although propofol can be used safely in a clean area with appropriate hand hygiene and a clean syringe,12 the risk of bacterial contamination still exists in clinical situations.11 On the other hand, propofol is known to have anti-inflammatory and antioxidant effects.13
Several studies have compared SSI occurrence rates between patients who received anesthesia maintenance with total intravenous anesthesia (TIVA) vs volatile anesthetics. A study on patients undergoing gastrointestinal surgery showed a higher proportion of early SSI in the propofol-based TIVA group compared with the sevoflurane group.14 Nevertheless, another study showed a lower rate of early SSI in the propofol group than in the sevoflurane group.15 Furthermore, a meta-analysis that included eight randomized trials on ventilated critical care patients did not show any significant difference in length of stay or in-hospital mortality between patients that received intravenous midazolam/propofol vs volatile agents.16 As such, the impact of propofol and volatile anesthetics on the occurrence of SSI remains uncertain.
We conducted the present study using a nationwide inpatient database in Japan to compare the occurrence of suspected early-onset periprosthetic joint infection in patients who underwent TKA under general anesthesia with either propofol or sevoflurane as the maintenance anesthetic agent.
Methods
The present study was approved (20 October 2011) by the Institutional Review Board of the University of Tokyo. Owing to the retrospective design of this study and the anonymous nature of the data, the requirement for obtaining informed patient consent was waived.
Data source
The Diagnosis Procedure Combination (DPC) is a national administrative database of claims data and discharge abstracts of acute-care inpatients in Japan.17 The database includes approximately seven million inpatients annually from more than 1,000 participating hospitals, which accounts for approximately 50% of acute-care hospitalizations in Japan. The following data are included in the database: primary diagnosis, comorbidities at admission, complications after admission, medical procedures (including surgery, which is coded with original Japanese codes), daily records of drug administration and treatments, dates of admission and discharge, and clinical information, including patient age, sex, body weight, height, and Brinkman index (the number of cigarettes smoked per day multiplied by the number of years of smoking).18,19 The database also includes anesthetic information related to surgery including anesthetic methods (general anesthesia, epidural anesthesia, spinal anesthesia, and peripheral nerve block), duration of anesthesia, and anesthetic drugs used. Each diagnosis is classified according to the International Classification of Diseases, 10th Revision.20 Physicians are responsible for accurately recording patient data in the medical records at discharge because these records are linked to the payment and reimbursement system.19 In addition to the DPC database, we obtained hospital characteristics (including academic hospital or not and number of hospital beds) from the Annual Report for Functions of Medical Institutions.21
Patient selection
Using the DPC database, we retrospectively identified patients who underwent TKA between 1 April 2012 and 31 March 2015 with general anesthesia using either propofol or sevoflurane for the maintenance of anesthesia. Patients who received general anesthesia were allocated to the propofol group when anesthesia was maintained with propofol-based TIVA. For the sevoflurane group, anesthesia was primarily maintained with sevoflurane, regardless of what drugs were used for induction. We included surgeries performed within seven days of hospital admission, with cefazolin for antibiotic prophylaxis beginning on the day of surgery. The usual dosing regimen of cefazolin is 1.0 gm before surgical incision, every three hours during surgery, and every eight hours postoperatively until 48 hr.
The following exclusion criteria were considered: 1) a history of a prior THA or contralateral TKA within 30 days of surgery, 2) age < 40 yr, 3) SSI treatment during the hospitalization with antibiotics other than anti-methicillin-resistant Staphylococcus aureus (MRSA) drugs and aminoglycosides, 4) missing data on hospital characteristics, duration of anesthesia, or type of intraoperative analgesia, 5) use of ketamine for anesthesia induction, and 6) diagnosis of gout or pseudogout.
Outcomes
The main outcome of the study was suspected periprosthetic joint injection, which was defined by the need for arthrocentesis and/or debridement (i.e., suppurative arthritis curettage and curettage of joint synovectomy) occurring within 30 days of surgery. Data on first readmissions were also included in the analysis. The secondary outcome was length of stay during the perioperative hospitalization.
Statistical analysis
Categorical variables are presented as percentages, and continuous data are presented as mean (SD). We estimated propensity scores using a logistic regression model with the anesthetic maintenance agent (propofol or sevoflurane) as the dependent variable. Independent variables included the following factors: age, sex, hospital characteristics (academic or non-academic hospitals and the number of beds), body mass index, Brinkman index, comorbidities (hypertension, diabetes, asthma, rheumatism, ischemic heart diseases, cerebral stroke, chronic kidney disease, and hepatic dysfunction), drugs administered on the day of surgery (anti-MRSA drugs, aminoglycoside, steroids, opioids, and muscle relaxants), use of regional analgesia (epidural analgesia or peripheral nerve block), duration of anesthesia, revision surgery, and blood transfusion on the day of surgery (red blood cells, fresh frozen plasma, or autologous blood). Patients with missing data were excluded from the analysis. A c-statistic was calculated to evaluate the goodness of fit.
Using the estimated propensity scores, we conducted a nearest neighbor one-to-one matching without replacement between the propofol and sevoflurane groups. To achieve a good balance of patient background between the groups, a cut-off was set at 0.25 multiplied by the standard deviation of the estimated propensity scores. We defined absolute values of the standardized difference of more than 10% as out of balance.22 In the matched patients, we compared the proportions of the main outcomes between the propofol and sevoflurane groups using a McNemar test; a pairwise t test was used to compare the mean length of stay. The relative risk (RR), risk difference, and their 95% confidence intervals (CI) were then calculated.
Statistical analysis was performed with IBM SPSS for Windows, version 22.0 (IBM, Armonk, NY, USA), and P < 0.05 was considered statistically significant.
Results
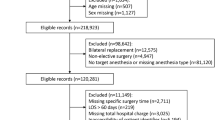
The patient flow diagram is shown in the Figure. Enrolled in the study were 33,520 patients who underwent TKA between 1 April 2012 and 31 March 2015. After excluding 11,616 patients according to the criteria, 21,899 patients were identified as eligible. Propensity score matching yielded 5,140 pairs of patients who received propofol or sevoflurane.
Table 1 shows the baseline characteristics of all eligible patients and propensity score-matched patients (n = 10,280). Before propensity score matching, patients in the propofol group were more likely to be hospitalized in low-capacity hospitals and receive anti-MRSA drugs and regional analgesia than those in the sevoflurane group. Patients in the propofol group were also less likely to receive opioids and muscle relaxants. After propensity score matching, the baseline characteristics were well balanced between the groups, with a c-statistic of 0.707.
In the propensity-matched patients, the number of patients who received both arthrocentesis and debridement were two in the propofol group and zero in the sevoflurane group. Table 2 shows the comparison of the proportion of patients who underwent arthrocentesis or debridement and the length of stay between the two groups. Before matching, there were no significant differences between the propofol and sevoflurane groups in the proportions of patients who underwent arthrocentesis or debridement (propofol vs sevoflurane: 1.2% vs 1.4%, P = 0.17). After propensity score matching, there were no significant differences in the proportions of patients who underwent arthrocentesis or debridement under propofol or sevoflurane anesthesia (1.3% vs 1.7%, respectively; RR, 0.76; 95% CI, 0.55 to 1.04; P = 0.10). Risk difference of the proportions of propensity-matched patients who underwent arthrocentesis or debridement was 0.4% (95% CI, −0.9% to 0.1%). Both before and after propensity score matching, there was a significant difference in the mean length of stay between the propofol and sevoflurane group.
Discussion
In this study, using a nationwide inpatient database in Japan, there was no significant association between the anesthetic maintenance agent (propofol or sevoflurane) and the suspected early-onset periprosthetic joint infection after TKA.
Patients in the propofol group were more likely to be admitted to low-capacity hospitals and receive anti-MRSA drugs. Although the anesthetic methods differed, patient backgrounds were similar, and there was no significant difference in comorbidities between the groups. Our results suggest that anesthetic methods for general anesthesia varied more according to hospital than patient characteristics.
The present study differs from previous studies in several respects. First, we used a nationwide database with a large population. Furthermore, the database enabled us to adjust for patient characteristics. Second, we only included patients who underwent TKA with a clean surgical wound,23 whereas previous studies14,15 included patients who underwent gastrointestinal surgery with wounds classified as clean-contaminated. Third, unlike previous single-center studies, our study included more than 1,000 Japanese hospitals.17
We used the following methods to minimize the influence of antibiotics on the results. First, we only included patients who were prescribed cefazolin for antibiotic prophylaxis, because cefazolin is the most widely used and suitable antibiotic for TKA. Second, we excluded patients who were treated with antibiotics other than anti-MRSA drugs or aminoglycosides, which are the most common antibiotics used with bone cement.24
Diagnosis of periprosthetic joint infection remains challenging, even though a wide variety of tests and combinations of tests are used for diagnosis. Nevertheless, the database used in this study did not include information, such as the results of serum markers or culture of periprosthetic fluid. Therefore, a surrogate outcome for suspected periprosthetic joint infection was used in the study: proportion of arthrocentesis or debridement. Various diagnostic criteria and algorithms for periprosthetic joint infection25,26,27,28 indicate the importance of arthrocentesis in establishing a diagnosis of periprosthetic joint infection and debridement with prosthesis retention as the main treatment for early-onset periprosthetic joint infection.
Propensity score matching allows a quasi-experimental comparison of groups with similar observed characteristics, without specifying the relationships between confounders and outcomes.29,30 After propensity score matching, the proportion of patients who underwent arthrocentesis or debridement was 1.3% in the propofol group and 1.7% in the sevoflurane group. The upper limit of the 95% confidence interval of the difference between the two groups was 0.1%, which indicates that the risk of suspected periprosthetic joint infection with the use of propofol was not significantly different. After propensity score matching, the mean length of stay was approximately 32.5 days in the propofol group, which was comparable to the past reports in Japan.31,32 There was a significant difference in the mean length of stay despite the similar occurrence of suspected periprosthetic joint infection. The result suggests that propofol could theoretically affect the occurrence of infections other than periprosthetic joint infection (e.g., pneumonia). Nevertheless, as the difference in the mean length of stay after propensity score matching was approximately one day, it is not considered clinically significant. Overall, the results suggest that there is no clinically significant increase in the risk of suspected periprosthetic joint infection with the use of propofol.
It is known that SSIs, including periprosthetic joint infection, occur because of a combination of bacterial load, virulence, and weakened resistance of the host patient.23 Our results showed no significant association between the choice of anesthetic maintenance agent and the occurrence of suspected periprosthetic joint infection. On the one hand, propofol has been suggested to support bacterial growth, and some consider it to be a risk factor for SSI. One possible explanation for the result of the present study is that the amount of propofol used during general anesthesia for TKA might not be sufficient to influence the risk of infection. Although propofol is known to have anti-inflammatory and antioxidant effects, these may not be enough to decrease infection in a clinical situation.
Several limitations of the present study should be acknowledged. First, we used surrogate outcomes for suspected periprosthetic joint infection. Therefore, our results may not reflect the actual occurrence of early-onset periprosthetic joint infection after TKA. Suspected periprosthetic joint infection may have been overestimated by using arthrocentesis as a surrogate outcome. Although we excluded patients with gout or pseudogout, using arthrocentesis as a surrogate measure may have inadvertently captured patients with non-infective etiologies (e.g., joint hematoma). Second, although we used a nationwide database, the present study might still be underpowered. With a larger population, a significant difference in the occurrence of suspected early-onset periprosthetic joint infection between the two groups might emerge. Also, data on several possible confounders were not available in the DPC database, including drug dosages, PaO2/FiO2 ratios, and total intravenous infusion volumes during surgery. Furthermore, risk factors for SSI, such as low body temperature and hyperglycemia, were not recorded in the DPC database. Additionally, information on outcomes was not available in the database when they occurred at hospitals other than the hospital where the surgery was performed. Lastly, this study was conducted in Japan where length of hospitalization is relatively long.33 In Japan, surgery and postoperative rehabilitation are implemented in a single hospitalization, and hospitalization after TKA tends to be longer when postoperative rehabilitation is included.32 Therefore, the results may not be generalizable to countries with shorter hospitalizations.
In conclusion, there was no significant association between the choice of agent used for the maintenance of anesthesia and the occurrence of suspected early-onset periprosthetic joint infection in patients undergoing TKA. There is no clinically significant increase in the risk of suspected periprosthetic joint infection when using propofol.
References
Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ. The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty 2015; 30: 47-50.
Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res 2010; 468: 52-6.
Namba RS, Inacio MC, Paxton EW. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am 2013; 95: 775-82.
Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am 2013; 95: 2177-84.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 2012; 27(61-5): e1.
Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvisi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty 2008; 23: 984-91.
Korol E, Johnston K, Waser N, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PloS One 2013; 8: e83743.
Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev 2014; 27: 302-45.
Chang CC, Lin HC, Lin HW, Lin HC. Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study. Anesthesiology 2010; 113: 279-84.
Bennett SN, McNeil MM, Bland LA, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med 1995; 333: 147-54.
Zorrilla-Vaca A, Arevalo JJ, Escandón-Vargas K, Soltanifar D, Mirski MA. Infectious disease risk associated with contaminated propofol anesthesia, 1989-2014. Emerg Infect Dis 2016; 22: 981-92.
King CA, Ogg M. Safe injection practices for administration of propofol. AORN J 2012; 95: 365-72.
Chen RM, Chen TG, Chen TL, et al. Anti-inflammatory and antioxidative effects of propofol on lipopolysaccharide-activated macrophages. Ann N Y Acad Sci 2005; 1042: 262-71.
Shimizu K, Hirose M, Mikami S, et al. Effect of anaesthesia maintained with sevoflurane and propofol on surgical site infection after elective open gastrointestinal surgery. J Hosp Infect 2010; 74: 129-36.
Koo BW, Sim JB, Shin HJ, et al. Surgical site infection after colorectal surgery according to the main anesthetic agent: a retrospective comparison between volatile anesthetics and propofol. Korean J Anesthesiol 2016; 69: 332-40.
Jerath A, Panckhurst J, Parotto M, et al. Safety and efficacy of volatile anesthetic agents compared with standard intravenous midazolam/propofol sedation in ventilated critical care patients: a meta-analysis and systematic review of prospective trials. Anesth Analg 2076; 124: 1190-9.
Yasunaga H, Matsui H, Horiguchi H, Fushimi K, Matsuda S. Clinical epidemiology and health services research using the diagnosis procedure combination database in Japan. Asian Pac J Dis Manage 2013; 7: 19-24.
Brinkman GL, Coates EO Jr. The effect of bronchitis, smoking, and occupation on ventilation. Am Rev Respir Dis 1963; 87: 684-93.
Hashimoto H, Ikegami N, Shibuya K, et al. Cost containment and quality of care in Japan: is there a trade-off? Lancet 2011; 378: 1174-82.
World Health Organization. International statistical classification of diseases and related health problems. World Health Organization 2014. Available from URL: http://apps.who.int/classifications/icd10/browse/2014/en#/II (accessed March 2018).
Ministry of Health, Labour and Welfare, Japan. Reporting System for Functions of Medical Institutions and Formation of Community Health Care Visions. Available from URL: http://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/dl/140711-01.pdf (accessed March 2018).
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 2009; 38: 1228-34.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999; 27: 97-134
Walker LC, Baker P, Holleyman R, Deehan D. Microbial resistance related to antibiotic-loaded bone cement: a historical review. Knee Surg Sports Traumatol Arthrosc 2017; 25: 3808-17.
Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 2012; 56: e1-25.
Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J 2013; 95: 1450-2.
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet 2016; 387: 386-94.
American Academy of Orthopaedic Surgeons. The Diagnosis of Periprosthetic Joint Infections of the Hip and Knee. Guideline and Evidence Report, June 2010. Available from URL: https://www.aaos.org/research/guidelines/PJIguideline.pdf (accessed March 2018).
Griswold ME, Localio AR, Mulrow C. Propensity score adjustment with multilevel data: setting your sites on decreasing selection bias. Ann Internal Med 2010; 152: 393-5.
Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 1985; 39: 33-8.
Yasunaga H, Tsuchiya K, Matsuyama Y, Ohe K. Analysis of factors affecting operating time, postoperative complications, and length of stay for total knee arthroplasty: nationwide web-based survey. J Orthop Sci 2009; 14: 10-6.
Ishii Y, Noguchi H, Takeda M, Sato J, Suzuki T. Length of hospital stay with patient-dependent determination in bilateral scheduled staged total knee arthroplasty. Eur J Orthop Surg Traumatol 2014; 24: 961-5.
Organisation for Economic Co-operation and Development. Length of hospital stay (indicator). Available from URL: https://data.oecd.org/healthcare/length-of-hospital-stay.htm (accessed March 2018).
Acknowledgements
The present study was supported by the Project for Accelerating Medical Research through Cross-regional ICT utilization from the Japan Agency for Medical Research and Development (AMED) and the Ministry of Health, Labour, and Welfare.
The authors would like to express their gratitude to the following individuals: Yuichi Nishioka, M.D., from the Department of Public Health, Health Management and Policy at Nara Medical University for statistical advice; Tetsuro Tani, M.D., from the Arthroplasty Center at Osaka Medical Center and Mr. Shinichiro Kubo from the Department of Public Health, Health Management and Policy at Nara Medical University for clinical advice; and Andrew Davies, Ph.D., for English editing.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Miwa Kishimoto, Hayato Yamana, and Satoki Inoue were involved in the study design, data analysis, data interpretation, and drafting of the manuscript. Tatsuya Noda, Hiroki Matsui, Hideo Yasunaga, Masahiko Kawaguchi, and Tomoaki Imamura were involved in data interpretation and revision of the manuscript; Manabu Akahane was involved in the study design, data interpretation, clinical advice as an orthopedic doctor, and revision of the manuscript. Yusuke Inagaki was involved in the clinical advice as an orthopedic doctor and revision of manuscript.
Funding disclosure
The present study was supported by the Project for Accelerating Medical Research through Cross-regional ICT utilization from the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kishimoto, M., Yamana, H., Inoue, S. et al. Suspected periprosthetic joint infection after total knee arthroplasty under propofol versus sevoflurane anesthesia: a retrospective cohort study. Can J Anesth/J Can Anesth 65, 893–900 (2018). https://doi.org/10.1007/s12630-018-1139-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-018-1139-6