Abstract
Objectives
Due to the water-rich cooking process required to soften texture modified diets (TMDs), TMDs may have poorer nutrition. The aim of this study was to investigate the associations between daily premorbid TMD consumption and nutritional status at the time of hospitalization, and its burden on hospitalization outcomes.
Design
Retrospective observational study.
Setting
An academic hospital.
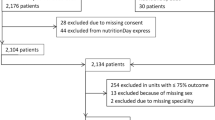
Participants
The cohort comprised 3,594 older adult patients aged ≥65 years admitted to the hospital.
Measurements
Patients were interviewed on admission using a premorbid daily consumption meal form to determine whether the patient ate a TMD. Nutritional status was examined using nutritional screening tools (Mini-Nutritional Assessment Short Form [MNA-SF], Malnutrition Universal Screening Tool [MUST], Geriatric Nutritional Risk Index [GNRI]) and the European Society of Clinical Nutrition and Metabolism (ESPEN)-defined criteria of malnutrition at admission. Length of hospital stay (LOS) and in-hospital mortality were considered outcomes of hospitalization. Multivariate analyses were performed to detect associations between premorbid TMD consumption and nutritional status and outcomes.
Results
The mean age of the subjects was 75.9±7.0 years, including 58% males. Overall, 110 (3.1%) patients consuming a premorbid TMD were identified. They were older (p<0.001), had poor nutritional status (lower MNA-SF score [p<0.001] and GNRI value [p<0.001], higher MUST score [p<0.001], and more prevalent ESPEN-defined malnutrition [61.8% vs. 14.0%, p<0.001] than did patients without a TMD. The mortality rate and LOS of patients with TMD was higher (7.3% vs. 2.9%, p=0.017) and longer (19 days vs. 8 days, p<0.001) than those without TMD. Multivariate analyses showed that TMD consumption was independently associated with poor nutritional status and prolonged LOS after adjusting confounders.
Conclusion
Daily consumption of a TMD during the premorbid period affects nutritional status at the time of hospitalization and outcomes. Further studies are necessary to investigate whether nutritional intervention can improve outcomes for people on a TMD.
Similar content being viewed by others
Abbreviations
- CCI:
-
Charlson Comorbidity Index
- DRM:
-
disease-related malnutrition
- ESPEN:
-
European Society of Clinical Nutrition and Metabolism
- FFMI:
-
fat-free mass index
- GNRI:
-
Geriatric Nutritional Risk Index
- MNA-SF:
-
Mini-Nutritional Assessment Short Form
- LOS:
-
length of stay
- MUST:
-
Malnutrition Universal Screening Tool
- TMD:
-
texture modified diet
References
Kagansky N, Berner Y, Koren-Morag N et al. Poor nutritional habits are predictors of poor outcome in very old hospitalized patients. Am J Clin Nutr 2005;82:784–791, doi: https://doi.org/10.1093/ajcn/82.4.784.
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr 2003;22:235–239; doi: https://doi.org/10.1016/S0261-5614(02)00215-7.
Salvi F, Giorgi R, Grilli A et al. Mini Nutritional Assessment (short form) and functional decline in older patients admitted to an acute medical ward. Aging Clin Exp Res 2008;20:322–328; doi: https://doi.org/10.1007/BF03324863.
Rasheed S, Woods RT. Malnutrition and quality of life in older people: a systematic review and meta-analysis. Ageing Res Rev 2013;12:561–566, doi: https://doi.org/10.1016/j.arr.2012.11.003.
Cederholm T, Barazzoni R, Austin P et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nut 2017;36:49–64, doi: https://doi.org/10.1016/j.clnu.2016.09.004.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412–423, doi: https://doi.org/10.1093/ageing/afq034.
Cederholm T, Jensen GL, Correia M et al. GLIM criteria for the diagnosis of malnutrition — A consensus report from the global clinical nutrition community. Clin Nutr 2019;38:1–9, doi: https://doi.org/10.1016/j.clnu.2018.08.002.
Maeda K, Takaki M, Akagi J. Decreased Skel et al. Muscle Mass and Risk Factors of Sarcopenic Dysphagia: A Prospective Observational Cohort Study. J Gerontol A Biol Sci Med Sci 2017;72:1290–1294, doi: https://doi.org/10.1093/gerona/glw190.
Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int 2016;16:515–521, doi: https://doi.org/10.1111/ggi.12486.
Fujishima I, Fujiu-Kurachi M, Arai H et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr Gerontol Int 2019;19:91–97, doi: https://doi.org/10.1111/ggi.13591.
Shimizu A, Maeda K, Tanaka K et al. Texture-modified diets are associated with decreased muscle mass in older adults admitted to a rehabilitation ward. Geriatr Gerontol Int 2018;18:698–704, doi: https://doi.org/10.1111/ggi.13233.
Maeda K, Ishida Y, Nonogaki T et al (Epub ahead of print) Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr, doi: https://doi.org/10.1016/j.clnu.2019.01.011.
Vucea V, Keller HH, Morrison JM et al. Modified Texture Food Use is Associated with Malnutrition in Long Term Care: An Analysis of Making the Most of Mealtimes (M3) Project. J Nutr Health Aging 2018;22:916–922, doi: https://doi.org/10.1007/s12603-018-1016-6.
Cederholm T, Bosaeus I, Barazzoni R et al. Diagnostic criteria for malnutrition — An ESPEN Consensus Statement. Clin Nutr 2015;34:335–40; doi: https://doi.org/10.1016/j.clnu.2015.03.001.
Rubenstein LZ, Harker JO, Salva A et al. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 2001;56:M366–372, doi: https://doi.org/10.1093/gerona/56.6.m366.
Stratton RJ, Hackston A, Longmore D et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr 2004;92:799–808, doi: https://doi.org/10.1079/BJN20041258.
Bouillanne O, Morineau G, Dupont C et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 2005;82:777–783, doi: https://doi.org/10.1093/ajcn/82.4.777.
Jassal SK, Wassel CL, Laughlin GA et al. Urine creatinine-based estimates of fat-free mass in community-dwelling older persons: the Rancho Bernardo study. J Ren Nutr 2015;25:97–102, doi: https://doi.org/10.1053/j.jrn.2014.07.005.
Maeda K, Akagi J. Muscle Mass Loss Is a Potential Predictor of 90-Day Mortality in Older Adults with Aspiration Pneumonia. J Am Geriatr Soc 2017;65:e18–e22, doi: https://doi.org/10.1111/jgs.14543.
Beck AM, Kjaersgaard A, Hansen T et al. Systematic review and evidence based recommendations on texture modified foods and thickened liquids for adults (above 17 years) with oropharyngeal dysphagia — An updated clinical guideline. Clin Nutr 2018;37:1980–1991, doi: https://doi.org/10.1016/j.clnu.2017.09.002.
Zanini M, Bagnasco A, Catania G et al. A Dedicated Nutritional Care Program (NUTRICARE) to reduce malnutrition in institutionalised dysphagic older people: A quasi-experimental study. J Clin Nurs 2017;26:4446–4455, doi: https://doi.org/10.1111/jocn.13774.
Reyes-Torres CA, Castillo-Martinez L, Reyes-Guerrero R et al (Epub ahead of print) Design and implementation of modified-texture diet in older adults with oropharyngeal dysphagia: a randomized controlled trial. Eur J Clin Nutr, doi: https://doi.org/10.1038/s41430-019-0389-x.
Pritchard SJ, Davidson I, Jones J et al. A randomised trial of the impact of energy density and texture of a meal on food and energy intake, satiation, satiety, appetite and palatability responses in healthy adults. Clin Nutr 2014;33:768–775, doi: https://doi.org/10.1016/j.clnu.2013.10.014.
Waza M, Maeda K, Katsuragawa C et al (Epub ahead of print) Comprehensive Tool to Assess Oral Feeding Support for Functional Recovery in Post-acute Rehabilitation. J Am Med Dir Assoc, doi: https://doi.org/10.1016/j.jamda.2018.10.022.
Maeda K, Koga T, Akagi J. Tentative nil per os leads to poor outcomes in older adults with aspiration pneumonia. Clin Nutr 2016;35:1147–1152, doi: https://doi.org/10.1016/j.clnu.2015.09.011.
Brogan E, Langdon C, Brookes K et al. Can’t swallow, can’t transfer, can’t toilet: factors predicting infections in the first week post stroke. J Clin Neurosci 2015;22:92–97, doi: https://doi.org/10.1016/j.jocn.2014.05.035.
Konturek PC, Herrmann HJ, Schink K et al. Malnutrition in Hospitals: It Was, Is Now, and Must Not Remain a Problem! Med Sci Monit 2015;21:2969–75; doi: https://doi.org/10.12659/MSM.894238
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia 2015;30:80–87, doi: https://doi.org/10.1007/s00455-014-9577-y.
Hartley P, Costello P, Fenner R et al. Change in skeletal muscle associated with unplanned hospital admissions in adult patients: A systematic review and meta-analysis. PLoS One 2019;14:e0210186, doi: https://doi.org/10.1371/journal.pone.0210186.
Cichero JA, Lam P, Steele CM et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia 2017;32:293–314, doi: https://doi.org/10.1007/s00455-016-9758-y.
Acknowledgments
The authors thank all the collaborators from our nutrition support teams at Aichi Medical University Hospital for their clinical work. This research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure statement: Keisuke Maeda received a grant from the Japan Society for the Promotion of Science (grant number: 18K11142) outside the submitted work. Other authors have no conflicts of interests.
Ethical standards: The study was approved by the ethics committee of Aichi Medical University. This study complies with the Japanese ethical guidelines for epidemiological research.
Rights and permissions
About this article
Cite this article
Maeda, K., Ishida, Y., Nonogaki, T. et al. Burden of Premorbid Consumption of Texture Modified Diets in Daily Life on Nutritional Status and Outcomes of Hospitalization. J Nutr Health Aging 23, 973–978 (2019). https://doi.org/10.1007/s12603-019-1237-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1237-3