Abstract
Background
Patients recently discharged from the hospital are vulnerable and are at high risk for readmission. Home-delivered meals may be beneficial in improving their health and facilitating independent living in the community. The purpose of this study was to identify the association between home-delivered meals and use of hospital services.
Methods
This study includes 120 clients recently discharged from an inpatient hospital stay or from an emergency department (ED) visit who received meal services from Meals On Wheels, Inc., of Tarrant County. Healthcare utilization data was extracted from the Dallas-Fort Worth Hospital Council Foundation, a regional all claims database used by over 90% of hospitals in Dallas-Fort Worth area. Signed tests and generalized linear models (GLM) were performed.
Results
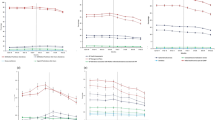
A total of 16,959 meals were delivered from March 2013 through March 2014. Each client received an average of 6.19 meals per week. The average number of ED visits decreased from 5.03 before receipt of meals to 1.45 after receipt of meals, z = -5.23, p <.001. The average number of hospitalizations decreased from 1.33 to.83, z = -7.29, p <.001. The average length of stay per hospitalization decreased from 5.47 days to 2.34 days, z = -5.84, p <.001. Clients who received more meals were less likely to experience ED visits and hospitalizations after controlling for demographic characteristics and levels of physical functioning.
Conclusion
The findings of this study indicate that home-delivered meals services may contribute to a reduction in hospital based care services among frail and vulnerable adults. Additional studies should consider the short and long-term effects of home-delivered meals services on healthcare utilization and the potential to decrease healthcare costs.





Similar content being viewed by others
References
Sokolovsky J. The cultural context of aging: Worldwide Perspectives. 3rd ed. Westport, CT: Praeger/Greenwood., 2009
United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2013. United Nations; New York, NY: 2013. ST/ESA/SER A/348. Available at: http://tinyurl.com/mx5cyyp. Accessed March 30, 2015.
Ortman JM, Velkoff VA, Hogan H. An aging nation: The older population in the United States. United States Census Bureau; 2014. Current Population Reports, P25-1140, Available at: http://tinyurl.com/n54vw9e. Accessed March 2015;30, 2015.
Admi H, Shadmi E, Baruch H, Zisberg A. From research to reality: Minimizing the effects of hospitalization on older adults. Rambam Maimonides Med J. 2015 Apr 29;6(2):e0017. doi: 10.5041/RMMJ.10201. eCollection 2015.
Naruishi K, Kunita A, Kubo K, Nagata T, Takashiba S, Adachi S. Predictors of improved functional outcome in elderly inpatients after rehabilitation: a retrospective study. Clin Interv Aging. 2014;9:2133–3241.
Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: ‘interface geriatrics’ Age Ageing 2011;40:436–443.
Medicare Payment Advisory Commission. Report to the Congress Medicare Payment Policy. Washington, DC: Medpac; 2013. Hospital Inpatient and Outpatient Services; pp. 41–74. Available at: http://www.medpac.gov/docs/default-source/reports/mar13_ ch03.pdf?sfvrsn=0. Accessed January 20, 2017.
Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J. Am Geriatr Soc 2004;52:1263–1270
Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med 2013;368:100–1022
Bohannon RW, Maljanian R, Ferullo J. Mortality and readmission of the elderly one year after hospitalization for pneumonia. Aging Clin Exp Res 2004;16:22–25
Sager MA, Rudberg MA, Jalaluddin M et al. Hospital admission risk profile (HARP): Identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc 1996;44:251–257
Pitta F, Troosters T, Probst VS et al. Physical activity and hospitalization for exacerbation of COPD. Chest 2006;129:536–544
Kansagara D, Englander H, Salanitro A et al. Risk prediction models for hospital readmission: A systematic review. JAMA 2011;306:1688–1698
Covinsky KE, Palmer RM, Fortinsky RH et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc 2003;51:451–458.
Gariballa SE, Parker SG, Taub N Castleden M. Nutritional status of hospitalized acute stroke patients. Br J Nutr 1998;79:481–487
Sullivan DH. The role of nutrition in increased morbidity and mortality. Clin Geriatr Med 1995;11:661–674
Sullivan DH, Walls RC, Bopp MM. Protein-energy undernutrition and the risk of mortality within one year of hospital discharge: A follow-up study. J Am Geriatr Soc 1995;43:507–512
Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: A prospective study. JAMA 1999;281:2013–2019
Vellas B, Conceicao J, Lafont C et al. Malnutrition and falls. Lancet 1990;336:1447–1447
Johnson CS. The association between nutritional risk and falls among frail elderly. J Nutr Health Aging 2003;7:247–250
Gazzotti C, Arnaud-Battandier F, Parello M et al. Prevention of malnutrition in older people during and after hospitalisation: Results from a randomised controlled clinical trial Age Ageing 2003;32:321–325
Chen CCH, Tang ST, Wang C et al. Trajectory and determinants of nutritional health in older patients during and six-month post-hospitalisation J Nutr Clin Nurs 2009;18:3299–3307
Neelemaat F, Bosmans JE, Thijs A et al. Post-discharge nutritional support in malnourished elderly individuals improves functional limitations J Am Med Dir Assoc 2011;12:295–301
Beck AM, Kjaer S, Hansen BS et al. Follow-up home visits with registered dietitians have a positive effect on the functional and nutritional status of geriatric medical patients after discharge: A randomized controlled trial Clin Rehabil 2012;6:483–493
Beck AM, Holst M, Rasmussen HH. Oral nutritional support of older (65 years+) medical and surgical patients after discharge from hospital: Systematic review and meta-analysis of randomized controlled trials Clin Rehabil 2013;27:19–27
Administration on Aging. AGing Integrated Database (AGID). Available at: http://www.agid.acl.gov/. Accessed January 11, 2017
Administration for Community Living. Nutrition services (OAA Title IIIC). Available at: https://aoa.acl.gov/AoA_Programs/hpw/Nutrition_Services/index.aspx. Accessed January 11, 2017.
Thomas KS, Mor V. The relationship between Older Americans Act Title III state expenditures and prevalence of low-care nursing home residents. Health Serv Res. 2013;48(3):1215–1226
Kamp B, Wellman NS, Russell C. Food and nutrition programs for older adults: Position statement of the American Dietetic Association, American Society for Nutrition, and Society for Nutrition Education. J Am Diet Assoc. 2010;110:463–472.
Sahyoun NR, Anyanwu UO, Sharkey JR, Netterville L. Recently hospital discharged older adults are vulnerable and may be underserved by the Older Americans Act Nutrition Program. J Nutr Elder 2010;29(2):227–240.
Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549–55.
Cho J, Throud J., Marishak-Simon S., Frawley L., Stevens AB. A model homedelivered meals program to support transitions from hospital to home. J Nutr Gerontol Geriatr 2015;34(2):207–217
Sharma S, Ogunyankin F, Shelton G, Jenkins KM. Readmissions in North Texas: A Comprehensive Overview of Statistics, Demographics and Charges to Identify Disparities. Irving, TX: Dallas-Fort-Worth Hospital Council Research and Education Foundation, 2014.
Rosati RJ, Huang L, Navaie-Waliser M, Feldman PH. Risk factors for repeated hospitalizations among home healthcare recipients. J Healthc Qual 2003;25(2):4–10; quiz-1
Posner BM, Jette AM, Smith KW, Miller DR. Nutrition and health risks in the elderly: The nutrition screening initiative. Am J Public Health 1993;83:972–978.
White JV, Ham RJ, Lipschitz DA, Dwyer JT, Wellman NS. Consensus of the Nutrition Screening Initiative: Risk factors and indicators of poor nutritional status in older Americans. J Am Diet Assoc. 1991;91:783–787.
Sahyoun NR, Jacques PF, Dallal GE, Russell RM. Nutrition Screening Initiative Checklist may be a better awareness/educational tool than a screening one. J Am Diet Assoc 1997;97:760–763.
Texas Health and Human Services. Form 2060, Needs Assessment Questionnaire and Task/Hour Guide. Available at: https://hhs.texas.gov/laws-regulations/forms/2000-2999/form-2060-needs-assessment-questionnaire-taskhour-guide. Accessed June 16, 2017
Thomas KS, Akobundu U, Dosa D. More than a meal? A randomized control trial comparing the effects of home-delivered meals programs on participants’ feelings of loneliness. J Gerontol B Psychol Sci Soc Sci 2016;71(6):1049–1058
Campbell AD, Godfryd A, Buys DR, Locher JL. Does participation in homedelivered meals programs improve outcomes for older adults? Results of a systematic review. J Nutr Gerontol Geriatr 2015;34(2):124–167
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–1428
Medicare & Medicaid Statistical Supplement. Baltimore: Centers for Medicare & Medicaid Services, 2007. Available at: www.cms.hhs.gov/MedicareMedicaidStatSupp/downloads/2007Table5.1b.pdf. Accessed January 20, 2017
Edwards DL, Frongillo EA, Rauschenbach B, et al. Home-delivered meals benefit the diabetic elderly. Journal of American Dietetic Association 1993;93(5):585–587.
Ponza M, Ohls JC, Millen BE, et al. 1996a. Serving elders at risk. The Older Americans Act Nutrition Programs: National evaluation of the Elderly Nutrition Program 1993–1995. Volume II: Title VI evaluation findings. 1996. Available at: http://mathematica-mpr.com/publications/pdfs/nutrition/elderlynutrition_vol2.pdf.
Ponza M, Ohls JC, Millen BE, et al. 1996b. Serving elders at risk. The Older Americans Act Nutrition Programs: National evaluation of the Elderly Nutrition Program 1993–1995. Volume I: Title III evaluation findings. Available at: http://ideas.repec.org/p/mpr/mprres/1675.html.
Frongillo EA and Wolfe WS. Impact of participation in Home-Delivered Meals on nutrient intake, dietary patterns, and food insecurity of older persons in New York state. Journal of Nutrition for the Elderly 2010;29(3):293–310.
Altshuler N, Schimmel J. Aging in place: Do Older Americans Act Title III services reach those most likely to enter nursing homes? Administration on Aging Research Brief Number 1. Available at: http://www.aoa.gov/AoARoot/Program_Results/docs/2010/AoA_1NursingHomes_041311.pdf.
Barrett A, Schimmel J. Multiple service use among OAA Title III program participants. Administration on Aging Research Brief Number 3. Available at: http://www.aoa.gov/AoARoot/Program_Results/docs/2010/AoA_3_ MultipleServices_041311.pdf.
Kleinman R, Foster L (2011) Multiple chronic conditions among OAA Title III program participants. Administration on Aging Research Brief Number 4. Available at: http://www.aoa.gov/AoARoot/Program_Results/docs/2011/AoA4_Chronic_508. pdf.
Gollub EA, Weddle DO. Improvements in nutritional intake and quality of life among frail homebound older adults receiving home-delivered breakfast and lunch. Journal of American Dietetic Association 2004;104(8):1227–1235.
Nieuwenhuizen WF, Weenen H, Rigby P, Hetherington MM. Older adults and patients in need of nutritional support: Review of current treatment options and factors influencing nutritional intake. Clin Nutr 2010;29(2):160–169.
Denissen KF, Janssen LM, Eussen SJ, van Dongen MC, Wijckmans NE, van Deurse ND, Dagnelie PC. Delivery of Nutritious Meals to Elderly Receiving Home Care: Feasibility and Effectiveness. J Nutr Health Aging 2017;21(4):370–380. doi: 10.1007/s12603-016-0790-2.
Chen CC, Schilling LS, Lyder CH. A concept analysis of malnutrition in the elderly. J Adv Nurs 2001;1):131–142.
Chumbler N, Beverly C, Beck C. Determinants of in-home health and support service utilization for rural older adults. Res Sociol Health Care. 1998;15:205–227.
Lee JS, Shannon J, Brown A. Characteristics of older Georgians receiving Older Americans Act Nutrition Program Services and other home-and community-based services: Findings from the Georgia Aging Information Management System (GA AIMS). J Nutr Gerontol Geriatr. 2015;34:168–188.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cho, J., Thorud, J.L., Marishak-Simon, S. et al. Frequency of Hospital Use Before and After Home-Delivery Meal by Meals On Wheels, of Tarrant County, Texas. J Nutr Health Aging 22, 519–525 (2018). https://doi.org/10.1007/s12603-017-0973-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0973-5