Abstract
Objectives
To collect information on actual nutritional intervention requirements in long-term care institutions and on the role of institutional factors in nutritional care.
Design
A cross-sectional analysis of baseline data (collected between September 2011 and September 2013) within the context of a multicenter prospective cohort study.
Setting
Nineteen long-term care institutions. Participants: Thirteen hundred and ninety-four resident elderly (age ≥60 years).
Measurements
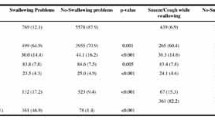
The prevalence of nutritional derangements (MNA-Short Form) and the need to introduce nutritional interventions on the residents. Results: Prevalence of malnutrition and risk of malnutrition were 35.2% [95%CI, 32.8–37.8] and 52.6% [95%CI, 50.0–55.2], respectively. Malnutrition was more frequent upon admission and in larger institutions (≥50 beds). Overall, 50% of the residents requiring an individualized nutritional care plan (any type) were not receiving it. Oral diet, the use of fluid thickeners and oral nutritional supplements had to be introduced in 306 (22.5%), 201 (15%) and 175 (13%) residents, respectively. The need to implement the oral diet was mainly due to inadequacy of texture according to chewing and swallowing capabilities. In gender and age-adjusted multivariable logistic regression models, nutritional interventions were associated with worse nutritional status (P<0.001 for all). Moreover, while the duration of stay was unrelated to the need for nutritional interventions, we observed that residents living in larger long-term care institutions (=50 beds) were more likely to require improvement in nutrition care.
Conclusions
In long-term care elderly residents nutritional derangements are very common, underdiagnosed and undertreated. Nutritional screening should be part of routine care. However, also the systematic involvement of a nutritional care specialist appears to be an urgent need, particularly in larger institutions where the standards of care are likely to be lower.
Similar content being viewed by others
References
Cereda E, Pedrolli C, Zagami A et al. Body mass index and mortality in institutionalized elderly. J Am Med Dir Assoc 2011;12:174–178.
Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr 2008;27:5–15.
Cereda E. Mini nutritional assessment. Curr Opin Clin Nutr Metab Care 2012;15:29–41.
Guigoz Y. The mini nutritional assessment (MNA) review of the literature what does it tell us? J Nutr Health Aging 2006;10:466–485.
Thomas DR, Ashmen W, Morley JE, Evans WJ. Nutritional management in long-term care: development of a clinical guideline. Council for Nutritional Strategies in Long-Term Care. J Gerontol A Biol Sci Med Sci 2000 Dec;55:M725–734.
Arvanitakis M, Beck A, Coppens P et al. Nutrition in care homes and home care: how to implement adequate strategies (report of the Brussels Forum (22–23 November 2007)). Clin Nutr 2008;27:481–488.
Salva A, Coll-Planas L, Bruce S et al. Nutritional assessment of residents in long-term care facilities (LTCFs): recommendations of the task force on nutrition and ageing of the IAGG European region and the IANA. J Nutr Health Aging 2009;13:475–483.
Tolson D, Rolland Y, Andrieu S et al.; The International Association of Gerontology and Geriatrics/World Health Organization/Society Française de Gérontologie et de Gériatrie Task Force. International Association of Gerontology and Geriatrics: a global agenda for clinical research and quality of care in nursing homes. J Am Med Dir Assoc 2011;12:184–189.
Morley JE, Vellas B, van Kan GA et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392–397.
Nieuwenhuizen WF, Weenen H, Rigby P, Hetherington MM. Older adults and patients in need of nutritional support: review of current treatment options and factors influencing nutritional intake. Clin Nutr 2010;29:160–169.
Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A, Hemsley A, Stein K. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev 2013;12:967–81.
National Institute of Statistics. Report on residential health and social care facilities in Italy (as of December 31st, 2010). iAvailable at: http://www.istat.it/it/archivio/77525
Amerio ML, Pezzana A, Bassetti G, Depau S, Devalle P. Proposte operative per la ristorazione assistenziale Regione Piemonte, Assessorato alla Tutela della salute e Sanità — Direzione Sanità Pubblica. Torino 2007
Kaiser MJ, Bauer JM, Ramsch C et al. for the MNA-International Group Validation of the mini nutritional assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009;13:782–788
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995;854:1–452.
Cereda E, Bertoli S, Vanotti A, Battezzati A. Estimated height from knee-height in Caucasian elderly: implications on nutritional status by mini nutritional assessment. J Nutr Health Aging 2010;14:16–22.
Cereda E, Vanotti A. Short dietary assessment improves muscle dysfunction identification by Geriatric Nutritional Risk Index in uncomplicated institutionalised patients over 70 years old. Clin Nutr. 2008;27:126–32.
Frankenfield DC, Muth ER, Rowe WA. The Harris–Benedict studies of human basal metabolism: history and limitations. J Am Diet Assoc 1998;98:439–445
Suiter DM, Leder SB. Clinical utility of the 3-ounce water swallow test. Dysphagia 2008;23:244–250.
ESPEN Guidelines on Enteral Nutrition. Clin Nutr 2006; 25:175–360.
ESPEN guidelines on Parenteral Nutrition. Clin Nutr 2009; 28:359–480.
Società Italiana di Nutrizione Parenterale ed Ente¬rale. Manuale di Nutrizione Artificiale. II Edizione. Alfredo Guida Editore, 2007
Cereda E, Pedrolli C, Zagami A et al. Nutritional screening and mortality in newly institutionalised elderly: a comparison between the Geriatric Nutritional Risk Index and the Mini Nutritional Assessment. Clin Nutr 2011;30:793–798.
National Pressure Ulcer Advisory Panel (NPUAP), European Pressure Ulcer Advisory Panel (EPUAP). Prevention and treatment of pressure ulcers: clinical practice guideline. Washington, DC: National Pressure Ulcer Advisory Panel; 2009.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Med State Med J 1965;14, 61–65.
American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (4th ed.). Washington, DC: American Psychiatric Press.
http://www.palmx.org/samplesize/Calc_Samplesize.xls
Verbrugghe M, Beeckman D, Van Hecke A et al. Malnutrition and associated factors in nursing home residents: a cross-sectional, multi-centre study. Clin Nutr 2013;32:438–443.
Cereda E, Klersy C, Pedrolli C, Cameletti B, Bonardi C, Quarleri L, Cappello S, Bonoldi A, Bonadeo E, Caccialanza R. The Geriatric Nutritional Risk Index predicts hospital length of stay and in-hospital weight loss in elderly patients. Clin Nutr 2014; IN PRESS. doi: 10.1016/j.clnu.2014.01.017.
Cereda E, Pusani C, Limonta D, Vanotti A. The ability of the Geriatric Nutritional Risk Index to assess the nutritional status and predict the outcome of home-care resident elderly: a comparison with the Mini Nutritional Assessment. Br J Nutr 2009;102:563–70.
Strathmann S, Lesser S, Bai-Habelski J et al. Institutional factors associated with thenutritional status of residents from 10 German nursing homes (ErnSTES study). J Nutr Health Aging 2013;17:271–276.
Martin AW. Dietary management of swallowing disorders. Dysphagia. 1991;6(3):129–34.
Bourdel-Marchasson I, Rolland C, Jutand MA et al. Undernutrition in geriatric institutions in South-West France: policies and risk factors. Nutrition 2009;25:155–164.
Shindler JS, Kelly JH. Swallowing disorders in the elderly. Laryngoscope 2002;112:589–602.
Rayner CK, Horowitz M. Physiology of the ageing gut. Curr Opin Clin Nutr Metab Care 2013;16:33–38.
Vahabi M, Schindel Martin L. Food security: who is being excluded? A case of older people with dementia in long-term care homes. J Nutr Health Aging 2014;18:685–91.
Dorner B, Friedrich EK, Posthauer ME. Practice paper of the American Dietetic Association: individualized nutrition approaches for older adults in health care communities. J Am Diet Assoc 2010;110:1554–1563.
Lorefält B, Wilhelmsson S. A Multifaceted Intervention Model Can Give a Lasting Improvement of Older peoples’ Nutritional Status. J Nutr Health Aging 2012;16:378–382.
Lee LC, Tsai AC, Wang JY, Hurng BS, Hsu HC, Tsai HJ. Need-based intervention is an effective strategy for improving the nutritional status of older people living in a nursing home: A randomized controlled trial. Int J Nurs Stud 2013;50:1580–1588
Simmons SF, Keeler E, Zhuo X, Hickey KA, Sato HW, Schnelle JF. Prevention of unintentional weight loss in nursing home residents: a controlled trial of feeding assistance. J Am Geriatr Soc 2008;56:1466–73.
Nijs KA, de Graaf C, Kok FJ, van Staveren WA. Effect of family style mealtimes on quality of life, physical performance, and body weight of nursing home residents: cluster randomised controlled trial. BMJ 2006;332:1180–4.
Shatenstein B, Ferland G. Absence of nutritional or clinical consequences of decentralized bulk food portioning in elderly nursing home residents with dementia in Montreal. J Am Diet Assoc 2000;100:1354–60.
Kruizenga HM, van Tulder MW, Seidell Jc et al. Effectiveness and cost-effectiveness of early screening and treatment of malnourished patients. Am J Clin Nutr 2005; 82:1082–1089.
Lorefält B, Andersson A, Wirehn AB, Wilhelmsson S. Nutritional status and health care costs for the elderly living in municipal residential homes—an intervention study. J Nutr Health Aging 2011;15:92–97.
Freijer K, Nuijten MJ, Schols JM. The budget impact of oral nutritional supplements for disease related malnutrition in elderly in the community setting. Front Pharmacol 2012;3:78.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pezzana, A., Cereda, E., Avagnina, P. et al. Nutritional care needs in elderly residents of long-term care institutions: Potential implications for policies. J Nutr Health Aging 19, 947–954 (2015). https://doi.org/10.1007/s12603-015-0537-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-015-0537-5