Abstract
Species of Lactobacillus have been proposed as potential candidates for treating wound infections due to their ability to lower pH, decrease inflammation, and release antimicrobial compounds. This study investigated the impact of lactobacilli (Lactobacillus acidophilus ATCC 4356, Lactobacillus casei ATCC 393, Lactobacillus reuteri ATCC 23272) secreted products on wound pathogens in vitro and in a murine wound infection model. Evaluation of 1–5 day lactobacilli conditioned media (CM) revealed maximal inhibition against wound pathogens using the 5-day CM. The minimum inhibitory concentration (MIC) of 5-day Lactobacillus CMs was tested by diluting CM in Mueller-Hinton (MH) broth from 0 to 25% and was found to be 12.5% for A. baumannii. Concentrating the CM to 10× with a 3 kDa centrifuge filter decreased the CM MIC to 6.25–12.5% for A. baumannii planktonic cells. Minimal impact of 5-day CMs was observed against bacterial biofilms. No toxicity was observed when these Lactobacillus CMs were injected into Galleria melonella waxworms. For the murine A. baumannii wound infection studies, improved survival was observed following topical treatment with L. acidophilus ATCC 4356 or L. reuteri ATCC 23272, while L. reuteri ATCC 23272 treatment alone improved wound resolution. Overall, this study suggests that the topical application of certain Lactobacillus species byproducts could be effective against gram-negative multi-drug resistant (MDR) wound pathogens, such as A. baumannii.




Similar content being viewed by others
References
Huang XZ, Cash DM, Chahine MA, Van Horn GT, Erwin DP, McKay JT, Hamilton LR, Jerke KH, Co EM, Aldous WK, Lesho EP, Lindler LE, Bowden RA, Nikolich MP (2010) Methicillin-resistant Staphylococcus aureus infection in combat support hospitals in three regions of Iraq. Epidemiol Infect:1–4. https://doi.org/10.1017/S0950268810001950
Lee BY, Singh A, David MZ, Bartsch SM, Slayton RB, Huang SS, Zimmer SM, Potter MA, Macal CM, Lauderdale DS, Miller LG, Daum RS (2013) The economic burden of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA). Clin Microbiol Infect 19(6):528–536. https://doi.org/10.1111/j.1469-0691.2012.03914.x
Calhoun JH, Murray CK, Manring MM (2008) Multidrug-resistant organisms in military wounds from Iraq and Afghanistan. Clin Orthop Relat Res 466(6):1356–1362. https://doi.org/10.1007/s11999-008-0212-9
Hospenthal D, Crouch H, English J, Leach F, Pool J, Conger N, Whitman T, Wortmann G, Robertson J, Murray C (2011) Multidrug-resistant bacterial colonization of combat-injured personnel at admission to medical centers after evacuation from Afghanistan and Iraq. J Trauma 71:S52–S57. https://doi.org/10.1097/TA.0b013e31822118fb
Rice LB (2008) Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis 197(8):1079–1081. https://doi.org/10.1086/533452
Blackledge MS, Worthington RJ, Melander C (2013) Biologically inspired strategies for combating bacterial biofilms. Curr Opin Pharmacol 13(5):699–706. https://doi.org/10.1016/j.coph.2013.07.004
Be NA, Allen JE, Brown TS, Gardner SN, McLoughlin KS, Forsberg JA, Kirkup BC, Chromy BA, Luciw PA, Elster EA, Jaing CJ (2014) Microbial profiling of combat wound infection through detection microarray and next-generation sequencing. J Clin Microbiol 52(7):2583–2594. https://doi.org/10.1128/JCM.00556-14
Mohammedsaeed W, McBain AJ, Cruickshank SM, O’Neill CA (2014) Lactobacillus rhamnosus GG inhibits the toxic effects of Staphylococcus aureus on epidermal keratinocytes. Appl Environ Microbiol 80(18):5773–5781. https://doi.org/10.1128/AEM.00861-14
Vong L, Lorentz RJ, Assa A, Glogauer M, Sherman PM (2014) Probiotic Lactobacillus rhamnosus inhibits the formation of neutrophil extracellular traps. J Immunol 192(4):1870–1877. https://doi.org/10.4049/jimmunol.1302286
Sonal Sekhar M, Unnikrishnan MK, Vijayanarayana K, Rodrigues GS, Mukhopadhyay C (2014) Topical application/formulation of probiotics: will it be a novel treatment approach for diabetic foot ulcer? Med Hypotheses 82(1):86–88. https://doi.org/10.1016/j.mehy.2013.11.013
Karska-Wysocki B, Bazo M, Smoragiewicz W (2010) Antibacterial activity of Lactobacillus acidophilus and Lactobacillus casei against methicillin-resistant Staphylococcus aureus (MRSA). Microbiol Res 165(8):674–686. https://doi.org/10.1016/j.micres.2009.11.008
Jebur M (2010) Therapeutic efficacy of Lactobacillus acidophilus against bacterial isolates from burn wounds. N Am J Med Sci 2(12):586–591. https://doi.org/10.4297/najms.2010.2586
Tejero-Sarinena S, Barlow J, Costabile A, Gibson GR, Rowland I (2012) In vitro evaluation of the antimicrobial activity of a range of probiotics against pathogens: evidence for the effects of organic acids. Anaerobe 18(5):530–538. https://doi.org/10.1016/j.anaerobe.2012.08.004
Onbas T, Osmanagaoglu O, Kiran F (2018) Potential properties of Lactobacillus plantarum F-10 as a bio-control strategy for wound infections. Probiotics Antimicrob Proteins.:1–14. https://doi.org/10.1007/s12602-018-9486-8
Mohammedsaeed W, Cruickshank S, McBain AJ, O’Neill CA (2015) Lactobacillus rhamnosus GG lysate increases re-epithelialization of keratinocyte scratch assays by promoting migration. Sci Rep 5:16147. https://doi.org/10.1038/srep16147
Al-Mathkhury HJF, Al-Aubeidi HJAR (2008) Probiotic effect of lactobacilli on mice incisional wound infections. J Al-Nahrain Univ 11(3):111–116
Zahedi F, Nasrabadi MH, Ebrahimi MT, Aboutalebi H (2011) Comparison of the effects of Lactobacillus brevis and Lactobacillus plantarum on cutaneous wound healing in rats. Afr J Microbiol Res 5(24):4226–4233
Huseini HF, Rahimzadeh G, Fazeli MR, Mehrazma M, Salehi M (2012) Evaluation of wound healing activities of kefir products. Burns 38(5):719–723. https://doi.org/10.1016/j.burns.2011.12.005
Trabelsi I, Ktari N, Ben Slima S, Triki M, Bardaa S, Mnif H, Ben Salah R (2017) Evaluation of dermal wound healing activity and in vitro antibacterial and antioxidant activities of a new exopolysaccharide produced by Lactobacillus sp.Ca6. Int J Biol Macromol 103:194–201. https://doi.org/10.1016/j.ijbiomac.2017.05.017
Oryan A, Alemzadeh E, Eskandari MH (2019) Kefir accelerates burn wound healing through inducing fibroblast cell migration in vitro and modulating the expression of IL-1ss, TGF-ss1, and bFGF genes in vivo. Probiotics Antimicrob Proteins Sep 11:874–886. https://doi.org/10.1007/s12602-018-9435-6
Vagesjo E, Ohnstedt E, Mortier A, Lofton H, Huss F, Proost P, Roos S, Phillipson M (2018) Accelerated wound healing in mice by on-site production and delivery of CXCL12 by transformed lactic acid bacteria. Proc Natl Acad Sci U S A 115(8):1895–1900. https://doi.org/10.1073/pnas.1716580115
Poutahidis T, Kearney SM, Levkovich T, Qi P, Varian BJ, Lakritz JR, Ibrahim YM, Chatzigiagkos A, Alm EJ, Erdman SE (2013) Microbial symbionts accelerate wound healing via the neuropeptide hormone oxytocin. PloS one 8(10):e78898. https://doi.org/10.1371/journal.pone.0078898
Gudadappanavar AM, Hombal PR, Timashetti SS, Javali SB (2017) Influence of Lactobacillus acidophilus and Lactobacillus plantarum on wound healing in male Wistar rats - an experimental study. Int J Appl Basic Med Res 7(4):233–238. https://doi.org/10.4103/ijabmr.IJABMR_329_16
Twetman S, Keller MK, Lee L, Yucel-Lindberg T, Pedersen AML (2018) Effect of probiotic lozenges containing Lactobacillus reuteri on oral wound healing: a pilot study. Benef Microbes:1–6. https://doi.org/10.3920/BM2018.0003
Gan BS, Kim J, Reid G, Cadieux P, Howard JC (2002) Lactobacillus fermentum RC-14 inhibits Staphylococcus aureus infection of surgical implants in rats. J Infect Dis 185(9):1369–1372. https://doi.org/10.1086/340126
Valdez JC, Peral MC, Rachid M, Santana M, Perdigon G (2005) Interference of Lactobacillus plantarum with Pseudomonas aeruginosa in vitro and in infected burns: the potential use of probiotics in wound treatment. Clin Microbiol Infect 11(6):472–479. https://doi.org/10.1111/j.1469-0691.2005.01142.x
Argenta A, Satish L, Gallo P, Liu F, Kathju S (2016) Local application of probiotic bacteria prophylaxes against sepsis and death resulting from burn wound infection. PloS one 11(10):e0165294. https://doi.org/10.1371/journal.pone.0165294
Olofsson TC, Butler E, Lindholm C, Nilson B, Michanek P, Vasquez A (2016) Fighting off wound pathogens in horses with honeybee lactic acid bacteria. Curr Microbiol 73(4):463–473. https://doi.org/10.1007/s00284-016-1080-2
Fu T, Liu YM (2017) Antibacterial effect of bacteriocin isolated from Lactobacillus plantarum ATCC 8014 on postoperative infection of mandibular fracture in vivo. J Craniofac Surg 28(3):679–682. https://doi.org/10.1097/SCS.0000000000003469
Satish L, Gallo PH, Johnson S, Yates CC, Kathju S (2017) Local probiotic therapy with Lactobacillus plantarum mitigates scar formation in rabbits after burn injury and infection. Surg Infect (Larchmt) 18(2):119–127. https://doi.org/10.1089/sur.2016.090
Peral MC, Martinez MA, Valdez JC (2009) Bacteriotherapy with Lactobacillus plantarum in burns. Int Wound J 6(1):73–81. https://doi.org/10.1111/j.1742-481X.2008.00577.x
Peral MC, Rachid MM, Gobbato NM, Huaman Martinez MA, Valdez JC (2010) Interleukin-8 production by polymorphonuclear leukocytes from patients with chronic infected leg ulcers treated with Lactobacillus plantarum. Clin Microbiol Infect 16(3):281–286. https://doi.org/10.1111/j.1469-0691.2009.02793.x
Cannon JP, Lee TA, Bolanos JT, Danziger LH (2005) Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis 24(1):31–40. https://doi.org/10.1007/s10096-004-1253-y
Gouriet F, Million M, Henri M, Fournier PE, Raoult D (2012) Lactobacillus rhamnosus bacteremia: an emerging clinical entity. Eur J Clin Microbiol Infect Dis 31(9):2469–2480. https://doi.org/10.1007/s10096-012-1599-5
Jacobs AC, Thompson MG, Black CC, Kessler JL, Clark LP, McQueary CN, Gancz HY, Corey BW, Moon JK, Si Y, Owen MT, Hallock JD, Kwak YI, Summers A, Li CZ, Rasko DA, Penwell WF, Honnold CL, Wise MC, Waterman PE, Lesho EP, Stewart RL, Actis LA, Palys TJ, Craft DW, Zurawski DV (2014) AB5075, a highly virulent isolate of Acinetobacter baumannii, as a model strain for the evaluation of pathogenesis and antimicrobial treatments. MBio 5(3):e01076–e01014. https://doi.org/10.1128/mBio.01076-14
Vilela SF, Barbosa JO, Rossoni RD, Santos JD, Prata MC, Anbinder AL, Jorge AO, Junqueira JC (2015) Lactobacillus acidophilus ATCC 4356 inhibits biofilm formation by C. albicans and attenuates the experimental candidiasis in Galleria mellonella. Virulence 6(1):29–39. https://doi.org/10.4161/21505594.2014.981486
Wasfi R, Abd El-Rahman OA, Zafer MM, Ashour HM (2018) Probiotic Lactobacillus sp. inhibit growth, biofilm formation and gene expression of caries-inducing Streptococcus mutans. J Cell Mol Med 22(3):1972–1983. https://doi.org/10.1111/jcmm.13496
Koll-Klais P, Mandar R, Leibur E, Marcotte H, Hammarstrom L, Mikelsaar M (2005) Oral lactobacilli in chronic periodontitis and periodontal health: species composition and antimicrobial activity. Oral Microbiol Immunol 20(6):354–361. https://doi.org/10.1111/j.1399-302X.2005.00239.x
Stsepetova J, Sepp E, Kolk H, Loivukene K, Songisepp E, Mikelsaar M (2011) Diversity and metabolic impact of intestinal Lactobacillus species in healthy adults and the elderly. Br J Nutr 105(8):1235–1244. https://doi.org/10.1017/S0007114510004770
Stanbro J, Bond M, Moore J, Stockelman M, Watters C (2016) The probiotic biofilm: Lactobacillus and Bifidobacterium survival tactics. In: Henderson J (ed) Biofilms: Characterization, Applications and Recent Advances. Nova Science Publishers, Inc, Hauppauge, NY, pp 121–152
McHugh ML (2011) Multiple comparison analysis testing in ANOVA. Biochem Med (Zagreb) 21(3):203–209
Jerome NP, Orton MR, d’Arcy JA, Feiweier T, Tunariu N, Koh DM, Leach MO, Collins DJ (2015) Use of the temporal median and trimmed mean mitigates effects of respiratory motion in multiple-acquisition abdominal diffusion imaging. Phys Med Biol 60(2):N9–N20. https://doi.org/10.1088/0031-9155/60/2/N9
Thompson MG, Black CC, Pavlicek RL, Honnold CL, Wise MC, Alamneh YA, Moon JK, Kessler JL, Si Y, Williams R, Yildirim S, Kirkup BC Jr, Green RK, Hall ER, Palys TJ, Zurawski DV (2014) Validation of a novel murine wound model of Acinetobacter baumannii infection. Antimicrob Agents Chemother 58(3):1332–1342. https://doi.org/10.1128/AAC.01944-13
Regeimbal JM, Jacobs AC, Corey BW, Henry MS, Thompson MG, Pavlicek RL, Quinones J, Hannah RM, Ghebremedhin M, Crane NJ, Zurawski DV, Teneza-Mora NC, Biswas B, Hall ER (2016) Personalized therapeutic cocktail of wild environmental phages rescues mice from Acinetobacter baumannii wound infections. Antimicrob Agents Chemother 60(10):5806–5816. https://doi.org/10.1128/AAC.02877-15
Servin AL (2004) Antagonistic activities of lactobacilli and bifidobacteria against microbial pathogens. FEMS Microbiol Rev 28(4):405–440. https://doi.org/10.1016/j.femsre.2004.01.003
Ramos AN, Sesto Cabral ME, Arena ME, Arrighi CF, Arroyo Aguilar AA, Valdez JC (2015) Compounds from Lactobacillus plantarum culture supernatants with potential pro-healing and anti-pathogenic properties in skin chronic wounds. Pharm Biol 53(3):350–358. https://doi.org/10.3109/13880209.2014.920037
Onwuakor CE, Nwaugo VO, Nnadi CJ, Emetole JM (2014) Effect of varied culture conditions on crude supernatant (bacteriocin) production from four Lactobacillus species isolated from locally fermented maize (ogi). Amer J Microbiol Res 2(5):125–130. https://doi.org/10.12691/ajmr-2-5-1
Sesto Cabral ME, Ramos AN, Macedo AJ, Trentin DS, Treter J, Manzo RH, Valdez JC (2014) Formulation and quality control of semi-solid containing harmless bacteria by-products: chronic wounds pro-healing activity. Pharm Dev Technol:1–8. https://doi.org/10.3109/10837450.2014.938858
Cabrera CA, Ramos AN, Loandos Mdel H, Valdez JC, Sesto Cabral ME (2016) Novel topical formulation for ischemic chronic wounds. Technological design, quality control and safety evaluation. Pharm Dev Technol 21(4):399–404. https://doi.org/10.3109/10837450.2015.1011661
Prince T, McBain AJ, O’Neill CA (2012) Lactobacillus reuteri protects epidermal keratinocytes from Staphylococcus aureus-induced cell death by competitive exclusion. Appl Environ Microbiol 78(15):5119–5126. https://doi.org/10.1128/AEM.00595-12
Sultana R, McBain AJ, O’Neill CA (2013) Strain-dependent augmentation of tight-junction barrier function in human primary epidermal keratinocytes by Lactobacillus and Bifidobacterium lysates. Appl Environ Microbiol 79(16):4887–4894. https://doi.org/10.1128/AEM.00982-13
Castiblanco G A, Yucel-Lindberg T, Roos S, Twetman S (2017) Effect of Lactobacillus reuteri on cell viability and PGE2 production in human gingival fibroblasts. Probiotics Antimicrob Proteins 9(3):278–283. https://doi.org/10.1007/s12602-016-9246-6
Zimmerman T, Gyawali R, Ibrahim S (2017) Autolyse the cell in order to save it? Inducing, then blocking, autolysis as a strategy for delaying cell death in the probiotic Lactobacillus reuteri. Biotechnol Lett 39(10):1547–1551. https://doi.org/10.1007/s10529-017-2380-8
Rousselle P, Braye F, Dayan G (2018) Re-epithelialization of adult skin wounds: cellular mechanisms and therapeutic strategies. Adv Drug Deliv Rev. https://doi.org/10.1016/j.addr.2018.06.019
Halper J, Leshin LS, Lewis SJ, Li WI (2003) Wound healing and angiogenic properties of supernatants from Lactobacillus cultures. Exp Biol Med (Maywood) 228(11):1329–1337. https://doi.org/10.1177/153537020322801111
Schneider LA, Korber A, Grabbe S, Dissemond J (2007) Influence of pH on wound-healing: a new perspective for wound-therapy? Arch Dermatol Res 298(9):413–420. https://doi.org/10.1007/s00403-006-0713-x
Percival SL, McCarty S, Hunt JA, Woods EJ (2014) The effects of pH on wound healing, biofilms, and antimicrobial efficacy. Wound Repair Regen 22(2):174–186. https://doi.org/10.1111/wrr.12125
Nagoba B, Suryawanshi N, Wadher B, Selkar S (2015) Acidic environment and wound healing: a review. Wounds 27(1)
Chan AP, Choi Y, Brinkac LM, Krishnakumar R, DePew J, Kim M, Hinkle MK, Lesho EP, Fouts DE (2018) Multidrug resistant pathogens respond differently to the presence of co-pathogen, commensal, probiotic and host cells. Sci Rep 8(1):8656. https://doi.org/10.1038/s41598-018-26738-1
Acknowledgments
Special thanks to the Army Wound Infections department at WRAIR for their support and assistance with the animal studies, specifically Yonas Alamneh, Rania Abu-Taleb, Jonathan Shearer, Samandra Demons, Anna Jacobs, Kathleen Umayam, Natalie-Makenna Gingras, Daniel Zurawski, and Yuanzheng Si.
Funding
The support for this work was provided by the Office of Naval Research under work unit number A1601.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures were performed in accordance with protocols approved by the Walter Reed Army Institute of Research (WRAIR)/Naval Medical Research Center (NMRC) Institutional Animal Care and Use Committee in compliance with all applicable Federal regulations governing the protection of animals in research.
Disclaimers
The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Army, Department of Defense, nor the US Government. Some authors are service members of the US Government. I am a military service member or federal/contracted employee of the US government. This work was prepared as part of my official duties. Title 17 U.S.C. 105 provides that “copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a US Government work as work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
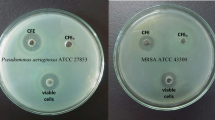
Fig. S1
(DOCX 49 kb)
Rights and permissions
About this article
Cite this article
Stanbro, J., Park, J.M., Bond, M. et al. Topical Delivery of Lactobacillus Culture Supernatant Increases Survival and Wound Resolution in Traumatic Acinetobacter baumannii Infections. Probiotics & Antimicro. Prot. 12, 809–818 (2020). https://doi.org/10.1007/s12602-019-09603-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-019-09603-z