Abstract
The purpose of the present study was to determine the effects of transcutaneous CO2 application on the blood flow and capillary architecture of the soleus muscle in rats with streptozotocin (STZ)-induced hyperglycemia. Wistar rats were randomly divided into four groups: control, control + CO2-treated, STZ-induced hyperglycemia, and STZ-induced hyperglycemia + CO2-treated groups. Blood flow in soleus muscle increased during the transcutaneous CO2 exposure, and continued to increase for 30 min after the treatment. In addition, the transcutaneous CO2 attenuated a decrease in capillary and the expression level of eNOS and VEGF protein, and an increase in the expression level of MDM-2 and TSP-1 protein of soleus muscle due to STZ-induced hyperglycemia. These results indicate that the application of transcutaneous CO2 could improve capillary regression via the change of pro- and anti-angiogenesis factors, which might be induced by an increase in blood flow.
Similar content being viewed by others
Introduction
The microvasculature in skeletal muscle changes in response to physiological or pathological conditions. An elevation in muscle activity such as exercise leads to angiogenesis [1], while a decrease in neuromuscular activity and an exposure to hyperglycemia result in capillary regression [2, 3].
Hyperglycemia is a risk factor for peripheral vascular diseases, which causes widespread tissue dysfunction and deleterious complications [4]. It is well known that poorly controlled hyperglycemia reduces both skeletal muscle mass [5, 6] and muscle capillarization [7, 8]. The number and diameter of capillaries are important factors in the delivery of oxygen and nutrients to all tissues including skeletal muscles and are these factors determining exercise capacity [9,10,11].
The architecture of capillaries is regulated by pro-angiogenic and anti-angiogenic factors in skeletal muscle. Vascular endothelial growth factor (VEGF) is a key factor in angiogenesis, while thrombospondin-1 (TSP-1) plays an important role in capillary regression [11,12,13,14,15,16]. These pro- and anti-angiogenic factors are well known to be associated with alterations in muscle capillaries in response to a variety of conditions, including exercise [11, 14], peripheral arterial disease [17, 18], and disuse [19,20,21]. In addition, an imbalance in the expression of pro- and anti-angiogenic factors is involved in capillary regression caused by diabetes-induced hyperglycemia [7]. Furthermore, it has been reported that high glucose levels are associated with increased expression levels of TSP-1 [22]. Therefore, it is necessary to optimize a balance in expression between pro-angiogenic and anti-angiogenic factors in order to attenuate angiopathy with hyperglycemia.
Endurance exercise training is well known as a principal countermeasure for attenuating hyperglycemia-induced capillary regression [23, 24]. However, there are instances where it is difficult for hyperglycemic subjects to undertake exercise training because of their complications and exercise intolerance. Therefore, it is necessary to develop an alternative treatment for hyperglycemic subjects with exercise intolerance.
Carbon dioxide (CO2) therapy has long been used as an effective treatment for cardiac disease and skin lesions [25,26,27]. CO2 therapy has been reported to promote effects such as vasodilation and increased blood flow in peripheral tissues, as well as a partial increase in O2 pressure in local tissues, known as the Bohr effects [25, 27,28,29,30,31]. The transfer of CO2 across the skin might have beneficial local vasomotor effects without causing systemic hemodynamic modifications [32]. These reports have indicated that CO2 therapy has a positive impact on microcirculation, such as elevated blood flow in peripheral tissues. An increase in blood flow leads to shear stress in endothelial cells and leads to enhancement of the expression levels of endothelial nitric oxide synthase (eNOS) in vascular endothelial cells [33,34,35], which plays a major role in many physiological functions, such as regulating vascular tone [36, 37] and insulin sensitivity [38]. In addition, up-regulation of eNOS expression by several types of stimulation, such as physical exercise and administration of prazosin, an α1-adrenergic receptor antagonist, leads to enhanced VEGF expression [35, 39] and resultant angiogenesis in skeletal muscle [39,40,41]. Indeed, it has been reported that CO2 therapy induces an increase in blood flow in subcutaneous tissues and angiogenesis via activation of eNOS and VEGF [31, 42, 43]. On the other hand, an increase in blood flow induced by administration of prazosin leads to an increase in the expression of murine double minute 2 (MDM-2) [23], which participates in capillary growth in skeletal muscle [44] and also acts as a negative regulator of TSP-1 [45]. It has been shown that TSP-1 in endothelial cells is downregulated in response to shear stress in vitro and vivo [46]. Therefore, the exposure of shear stress to endothelial cells could regulate the capillaries in skeletal muscle via the expression of MDM-2 and TSP-1. From these reports, it is plausible to conclude that application of transcutaneous CO2 to diabetic rats could increase the blood flow in skeletal muscle and play a positive role in the maintenance of the capillary network by modulating pro- and anti-angiogenic factors, such as VEGF, eNOS, MDM-2, and TSP-1 within the muscle. The purpose of the present study was to investigate whether transcutaneous application of CO2 treatment attenuates capillary regression and optimizes angiogenic signaling in skeletal muscle of rats with hyperglycemia.
Materials and methods
Animals
Twenty-nine male Wistar rats were purchased from Japan SLC (Hamamatsu, Japan). The rats were housed in an isolated and environmentally controlled room at 22 ± 2 °C on a 12–12-h light–dark cycle and had access to food and water ad libitum. The study was approved by the institutional Animal Care and Use Committee and was performed according to the Kobe University Animal Experimentation Regulations. All experiments were conducted in accordance with the National Institutes of Health (NIH) Guidelines for the Care and Use of Laboratory Animals (National Research Council 1996).
Transcutaneous CO2 therapy
All animals were anesthetized with isoflurane (Wako, Japan), the hairs on their hind limbs were shaved, and CO2 hydrogel, which enhances transcutaneous CO2 absorption (NeoChemir Inc., Kobe, Japan) was applied on their hind limbs, as previously described [30, 43]. In the previous study, the exposure of CO2 gas without CO2 hydrogel and application of CO2 hydrogel without CO2 gas do not almost give rise to transfer CO2 across the rat skin [30]. The CO2 adaptor was attached to the limbs and sealed under no anesthetic condition; 100% CO2 gas (Mizushima Sanso, Kobe, Japan) was administered into the adaptor for 30 min, as previously described [43].
Experiment 1
Firstly, the effects of transcutaneous CO2 application on blood flow in the soleus muscle were determined. Five Wistar rats (342–370 g) were used. Blood flow in the soleus muscle of each rat was measured before and 5, 10, 20, and 30 min after the application or not of transcutaneous CO2. During the measurement of blood flow, heart rate and blood pressure were also monitored. The rats were anesthetized by inhalation of 2% isoflurane gas via facemask. After administration of heparin (1000 IU/kg, i.p.), a cannula was inserted into the carotid artery. A tracheotomy was performed, followed by connection of the rat to an artificial ventilator (Shimano Seisakujo, Tokyo, Japan). The CO2 adaptor was attached to both of the hind limbs of rats and sealed, and 100% CO2 gas was administered into the adaptor. To analyze blood flow in soleus muscle during the CO2 application, firstly, a small hole was drilled in the adaptor. The probe of a laser Doppler flowmeter was inserted into the adaptor through the hole and then the adaptor was sealed. Transcutaneous CO2 was applied to both of their hind limbs. The belly of the soleus muscle was exposed and blood flow in the right skeletal muscle was measured with a laser Doppler flowmeter (ALF21, Advance, Tokyo, Japan).
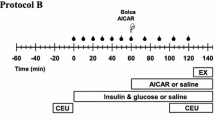
Experiment 2
We determined whether application of transcutaneous CO2 could prevent capillary regression due to hyperglycemia. We used a hyperglycemic rodent model generated by a single injection of streptozotocin (STZ), a compound that displays a preferential toxicity towards pancreatic β cells. Twenty-four 8-week-old rats (223–274 g) were randomly divided into four groups: control (CON; n = 6), carbon dioxide-treated (CO2; n = 6), streptozotocin-induced hyperglycemic (STZ; n = 6), and streptozotocin-induced hyperglycemic plus carbon dioxide-treated (STZ + CO2; n = 6) groups. Application of transcutaneous CO2 was performed five times a week for 8 weeks. Hyperglycemia was induced by a single intravenous injection of 50 mg/kg streptozotocin (Wako, Japan) dissolved in citrate buffer. Blood glucose levels were measured 2 days after the injection, and animals with blood glucose levels of more than 250 mg/dl were used as hyperglycemic models. The rats in the STZ and STZ + CO2 groups were injected with STZ, and the rats in the CON and CO2 groups were injected with the same volume of citrate buffer.
Muscle preparation
The rats were anesthetized deeply with sodium pentobarbital (50 mg/kg, i.p.). The left soleus muscle was removed, cleaned of excess fat and connective tissue, weighed, immediately frozen in isopentane cooled with dry ice, and stored at − 80 °C until histochemical and biochemical analyses were performed. The three-dimensional (3D) capillary architecture of the right soleus was visualized as described previously [2, 20, 21, 47, 48]. Briefly, a catheter was inserted into the right iliac artery and physiological saline containing heparin (50 mg/kg, i.p.) was injected to wash out intravascular blood. The right soleus was then perfused with 8% gelatin containing 2% fluorescent material as contrast medium. The right soleus muscle was removed and immediately frozen in isopentane cooled with dry ice and stored at − 80 °C until analyses of the 3D capillary architecture network were performed.
Histochemical analysis
The left soleus muscle was sliced into 10-μm-thick transverse sections using a cryostat microtome (CM-1510S, Leica Microsystems, Mannheim, Germany). Sections were stained with alkaline phosphatase (AP) to visualize capillaries in the soleus muscle. Sections were incubated in 0.1% 5-bromo-4-chloro-3-indolyl phosphate/nitro blue tetrazolium for 45 min at 37 °C and fixed with 4% paraformaldehyde, as previously described [19]. The stained sections were used for counting the number of capillaries and muscle fibers to calculate capillary-to-fiber (C/F) ratios with the ImageJ (NIH, Bethesda, MD, USA).
Three-dimensional visualization of the capillary network
The visualization of 3D capillary architecture in the soleus muscle was performed using a confocal laser scanning microscope (C2, Nikon, Tokyo, Japan) with an argon laser (488 nm), as previously described [2, 20, 47]. Briefly, the frozen right soleus muscle was longitudinally cut into 100-μm sections using a cryostat (CM-1510S, Leica Microsystems, Mannheim, Germany). Microscopic 3D capillary images were obtained at a magnification of 20× and scanned in 1-μm-thick longitudinal slices over a total depth of 50 μm. The 50 images were stacked and converted into digital images. These results of mean capillary volume and luminal diameter were obtained using 7–10 3D images per a muscle. The capillary volume was measured in a cube (200 µm long, 200 µm wide, and 50 µm deep) using NIH’s Image software program (NIH, Bethesda, MD, USA), and then calculated in cubic meters (10−2 mm3/mm3). At least five representative areas within each of 7–10 3D images were analyzed and overall average was calculated. The capillary luminal diameter (µm) was also measured about 30–90 spots per a 3D image using NIH’s Image software program.
Western blotting
Portions (approximately 10 mg) of each soleus muscle were homogenized in RIPA lysis buffer containing 1 mM Na3VO4, 1 mM NaF and protease inhibitor cocktail (1:100, P8340; Sigma Chemicals, Perth, WA, USA). Total supernatant protein concentrations were determined according to the Bradford method using a protein assay kit (Bio-Rad Laboratories, Hercules, CA, USA) before loading onto either 7.5, 10, or 12.5% SDS–polyacrylamide gels. Proteins were blotted on polyvinylidene difluoride (PVDF) membranes and blocked for 1 h with 5% skimmed milk in phosphate-buffered saline with 0.1% Tween 20 (PBST). Membranes were incubated using antibodies against eNOS (1:1000 in PBST, #5880; Cell Signaling, Danvers, MA, USA), VEGF (1:200 in PBST, sc-7269; Santa Cruz Biotechnology, Dallas, TX, USA), TSP-1 (1:200 in PBST, sc-59887; Santa Cruz Biotechnology) or MDM-2 (1:1000 in PBST, OP115; Calbiochem, La Jolla, CA, USA) overnight at 4 °C and then incubated in a solution with HRP-conjugated anti-mouse secondary antibodies (1:1000 in PBST, GE Healthcare, Waukesha, WI, USA) for 1 h. Proteins were detected using EzWestLumi One (ATTO, Tokyo, Japan). Finally, images were analyzed with a LAS-1000 (Fujifilm, Tokyo, Japan) using a chemiluminescent image analyzer and quantified using the Multi-Gauge Image Analysis Software program (Fujifilm) against a relative concentration of GAPDH (1:1000 in PBST, #97166; Cell Signaling) as an internal control.
Statistical analyses
The data of experiment 1 were assessed by two-way repeated measured ANOVA, followed by Tukey’s post hoc test. The data of experiment 2 were presented as mean ± SEM. The differences were assessed by two-way ANOVA, followed by Tukey’s post hoc test. Results were deemed statistically significant at p < 0.05.
Results
Blood flow dynamics, heart rate, and blood pressure
Blood flow in the soleus muscle was higher 5, 10, 20, 30 min after than before application of transcutaneous CO2 and higher at the same time points after application than no application (Fig. 1a). Blood pressure and heart rate were not affected by transcutaneous CO2 (Fig. 1b).
Changes in blood flow in skeletal muscle before and after application or not of CO2 (a). The data are expressed as fold change (a.u.) from the value before application or not of CO2. Blood pressure and heart rate in rats before and after application or not of CO2 (b). Values are presented as mean ± SEM. * and †: significantly different from before the same intervention, and no application of CO2 at the same time point, respectively, at p < 0.05
Body mass, soleus muscle mass, fasting blood glucose, and C/F ratio
The mean body mass and soleus muscle mass significantly decreased due to the 8-week hyperglycemia (Table 1). Blood glucose levels were significantly higher in the STZ and STZ + CO2 groups than in the CON and CO2 groups, and lower in the STZ + CO2 group than in the STZ group (Table 1). The C/F ratio was not significantly different between in the CON and CO2 groups, whereas it was significantly increased in the CON and STZ + CO2 groups compared to the STZ group (Table 1).
3D capillary architecture
Representative confocal images of the 3D capillary architecture of a soleus muscle from a rat in each group are shown in Fig. 2a–d. Mean capillary diameter was significantly higher in the CO2 group compared to the CON group (6.9 ± 0.1 vs. 6.3 ± 0.1 μm, Fig. 2e), whereas they were significantly lower in the STZ group than in the CON and STZ + CO2 groups (5.5 ± 0.2 vs. 6.3 ± 0.1 and 6.4 ± 0.1 μm, Fig. 2e). Mean capillary volume were significantly higher in the CO2 group than in the CON group (11.0 ± 0.6 vs. 8.9 ± 0.7 10−2 mm3/mm3, Fig. 2f), whereas they were significantly lower in the STZ group than in the CON and STZ + CO2 groups (6.6 ± 0.6 vs. 8.9 ± 0.7 and 9.9 ± 0.2 10−2 mm3/mm3, Fig. 2f). The frequency distributions of capillary luminal diameters and volumes are shown in Fig. 2g–n; the frequency distribution in the STZ group was shifted towards reduced capillary diameters and volumes compared with that in the CON, CO2 and STZ + CO2 groups, which indicates that smaller capillaries were more abundant and the capillary density in skeletal muscle decreased in the STZ group.
A representative confocal laser-scanning microscopy image of the 3D capillary architecture in the soleus muscle in the CON (a), CO2 (b), STZ (c), and STZ + CO2 (d) groups. Scale bar = 100 μm. Mean capillary luminal diameters (e) and volumes (f) in the soleus muscles in each group. Values are presented as mean ± SEM. * and † indicates significantly different from CON with same intervention and CO2 (−) vs. CO2 (+), respectively, at p < 0.05. Frequency distributions of capillary luminal diameters and capillary volumes for the CON (g, k), CO2 (h, l), STZ (i, m), and STZ + CO2 (j, n) groups are displayed. Arrows indicate the medians of capillary luminal diameters and volume
Expression levels of eNOS, VEGF, MDM-2, and TSP-1
Representative images of Western blots for eNOS, VEGF, MDM-2 and TSP-1 in the soleus muscle are shown in Fig. 3. There are no significant differences in the protein levels of eNOS, VEGF, MDM-2, and TSP-1 between the CON and CO2 groups. The protein levels of eNOS and VEGF were significantly higher in the STZ + CO2 group than in the STZ group (Fig. 3b, c). MDM-2 levels were significantly lower in the STZ group than in the CON group, whereas they were significantly higher in the STZ + CO2 group than in the STZ group (Fig. 3d). TSP-1 levels were significantly higher in the STZ group than in the CON group, whereas they were significantly lower in the STZ + CO2 group than in the STZ group (Fig. 3e).
Representative protein expression of eNOS, VEGF, MDM-2, and TSP-1 by Western blot (a). Mean protein expression levels of eNOS (b), VEGF (c), MDM-2 (d), and TSP-1 (f) in the soleus muscles in each group. The data are expressed as fold change (a.u.) from the value in the CON group, which is set to a value of 1. The levels of protein expression were normalized to GAPDH levels. Values are presented as mean ± SEM. * and † indicate significantly different from CON with same intervention and CO2 (−) vs. CO2 (+), respectively, at p < 0.05
Discussion
We found that application of transcutaneous CO2 increased muscle blood flow and attenuated capillary regression in the skeletal muscle of STZ-induced hyperglycemic rats in the present study. Furthermore, CO2 therapy counteracted the hyperglycemia-induced changes in pro- and anti-angiogenic factors, such as eNOS, VEGF, MDM-2, and TSP-1 as well as the alterations in muscle capillarity.
It has long been known that the change of blood pH influences microcirculation in local tissue via the change of vascular tone. This is due to the fact that a decrease in pH relaxes the vascular tissue, causing an increase in blood flow in local tissue, but an increase in pH induces vascular contraction [49, 50]. Also, an increase in CO2 tension in blood results in a decrease in pH of the blood [51]. It has been observed that CO2 applied to the vascular network induced arteriolar vasodilation [52]. From these reports, it is presumed that vasodilation in response to CO2 could be regulated by pH in blood. Indeed, the previous study demonstrated that our transcutaneous CO2 system led to a decrease in pH in intramuscular and an artificial Bohr effect [30]. Transfer of CO2 across the skin had beneficial local vasomotor effects without inducing systemic hemodynamic modifications, which was associated with an increase in blood flow by CO2 treatment [32]. Additionally, a recent study demonstrated that CO2 therapy resulted in vasodilation and an increase in blood flow in the femoral subcutaneous tissue of rats, as revealed by digital microscope and near-infrared spectroscopy [31]. The immersion of ischemic mouse hindlimbs into a bath of artificially created CO2-enriched water led to a nitric oxide-dependent increase in collateral blood perfusion [42]. Thus, CO2 treatment has beneficial effects for the microvascular circulation, such as vasodilation and an increase in blood flow in the tissue. In line with these reports, our results demonstrated that application of transcutaneous CO2 increases blood flow in skeletal muscle, as shown in experiment 1. Together these reports, CO2 application has a possible impact on an increase in blood flow in pH- and/or NO-dependent manner in the applied muscle tissue. However, the present study did not completely explain the underlying mechanisms, so that our future study should focus on whether or not the CO2 application actually affects blood pH and NO production in the applied muscle tissue such as soleus muscle.
Based on the results of the present study, we investigated the effect of CO2 therapy-induced increase in blood flow on capillary architecture and associated angiogenic factors in the skeletal muscles of STZ-induced hyperglycemic rats. VEGF is well known as a regulator of angiogenesis, stimulating the formation of new vascular networks by the recruitment and the promotion of differentiation of endothelial cells [53]. In addition, VEGF is an important molecule for angiogenesis in skeletal muscle [54]. In fact, endurance exercise training promotes angiogenesis in skeletal muscle via the expression of VEGF [55]. However, STZ-induced hyperglycemia resulted in capillary regression, whereas there was not a significant difference in VEGF expression between the CON and STZ group in this study. VEGF has been established as an essential trigger for the initiation of angiogenesis by several stimuli [55,56,57,58,59,60,61]. Nevertheless, capillary density remains unchanged in the organs and tissues of endothelial-cell-targeted Vegf gene deletion in mice [62]. Also, it has been reported that capillary regression in skeletal muscle may not be influenced to a greater degree by angiogenic factors such as VEGF in several conditions [8, 19, 48, 63]. Combining these results, Olfert et al. [64] concluded that while the evidence for VEGF as an essential trigger for the initiation of angiogenesis has been well established, VEGF is not required to maintain the already developed microvascular structure and capillary regression. From these reports, a decrease in the expression levels of VEGF would not necessarily be required for capillary regression in diabetic muscle. On the other hand, TSP-1 is generally known as an inhibitor of angiogenesis and has anti-proliferative and pro-apoptotic effects [1, 12, 14, 16, 65]. A decrease in the number and structural alterations of capillaries, such as a decrease in diameter and volume, is accompanied by an increase in TSP-1, which is observed in disuse, ovariectomy, and diabetes [20, 24, 48]. It has also been reviewed by Olfert et al. [64] that TSP-1 could be an important factor for capillary regression and rarefaction. In line with these reports, we found an increase in TSP-1 expression levels in diabetic muscle compared with non-diabetic control muscle. This suggested that capillary regression in the STZ group observed in this study did depend on an alteration in TSP-1, but not VEGF, protein expression.
It has been reported that elevated shear stress associated with an increase in blood flow promotes the expression of eNOS [33, 34, 66], which enhances endothelial cell proliferation [67]. In addition, prazosin, which increases tissue blood flow, induces angiogenesis in skeletal muscle via shear stress-dependent eNOS expression [35]. Thus, an increase in blood flow appears to be a strong modulator of eNOS concentration. An up-regulation of eNOS expression enhanced VEGF expression and the resultant capillary growth [39]. Moreover, it has been reported that the increased blood flow-induced eNOS and VEGF expression improved structural alterations of the microvasculature of unloaded muscle [21]. Accordingly, these results suggest that an increase in blood flow is a crucial factor for angiogenesis through the enhancement of eNOS and VEGF-related signaling. On the other hand, it has been shown that CO2 therapy promotes blood flow in subcutaneous tissue and, additionally, upregulates the expression of eNOS and VEGF in ischemic rodent muscles [31, 42]. In the present study, an increase in blood flow was observed by transcutaneous CO2 application, as shown in experiment 1. Also, the application of transcutaneous CO2 to hyperglycemic rats promoted eNOS and VEGF expression and improved the abnormality of the microvasculature caused by STZ-induced diabetes. Therefore, these results suggest that the increase in blood flow caused by transcutaneous CO2 enhanced eNOS and VEGF-related signaling, which contributed to protection of muscle capillary regression in hyperglycemic rats.
MDM-2 has been known as a major negative regulator of p53 and plays a major role in angiogenesis in tumors [68]. Notably, a recent study reported that MDM-2 contributes to capillary growth and regression in skeletal muscle tissue as well [45]. It has been reported that increased MDM-2 expression by exercise induces angiogenesis in the skeletal muscle of Zucker diabetic fatty rats [45]. The report also demonstrated that reduced MDM-2 expression in skeletal muscle results in an increase in TSP-1 expression and lower levels of angiogenesis independent of p53. Additionally, prazosin-induced increase in blood flow was associated with expression of MDM-2 [23], but downregulation of TSP-1 expression in endothelial cell in vivo studies [46]. From these studies, it can be concluded that elevated blood flow could regulate muscle angiogenesis via modulating MDM-2- and TSP-1-related signaling. In the present study, STZ-induced diabetes decreased the expression of MDM-2 and increased the expression of TSP-1. Therefore, these results suggested that a decrease in MDM-2 in STZ-induced diabetes could be associated with capillary regression induced by overexpression of TSP-1. On the other hand, transcutaneous CO2 improved the alterations in MDM-2 and TSP-1 expression in hyperglycemic muscle. These results suggest that blood flow elevated by transcutaneous CO2 could increase not only eNOS expression but also MDM-2 expression, which suppresses the upregulation of TSP-1 and resultant capillary regression observed in hyperglycemic muscle.
However, application of transcutaneous CO2 to control rats failed to increase the expression levels of eNOS and VEGF in experimental 2, even though led to an increase in the blood flow in the experiment 1. In the previous study, it has been shown that shear stress was increased in muscle of normal rats after acute electrically muscle stimulation but not after chronic stimulation [69]. It has also been reviewed that shear stress in capillary had returned to control value level after chronic stimulation, since there were many more pre-capillary arterioles distributing flow through a capillary bed that had increased in size [70]. It has also been reviewed that after chronic stimulation, shear stress in capillary had returned to control values since there were many more pre-capillary arterioles distributing flow through a capillary bed that had increased in size [71]. In this study, an increase in blood flow of skeletal muscle was observed as an acute effect of transcutaneous CO2. On the other hand, the chronic treatment in experiment 2 demonstrated that the application of transcutaneous CO2 had already increased capillary luminal diameter and volume. Together these results suggested that an increase in eNOS and VEGF expression levels might be occurred in the early stage of the CO2 treatment, resulting in an increased capillary luminal diameter and volume in the CO2 group, but not at a point after 8 weeks of the treatment in the present study.
This study demonstrates a novel effect of transcutaneous CO2 on capillary abnormalities in STZ-induced hyperglycemia, as shown by improvement in the number and architecture of capillaries in skeletal muscle. The underlying mechanisms could involve eNOS and VEGF expression as well as MDM-2 and TSP-1-related signaling, which could be induced by the increase in blood flow brought about by CO2 application. The positive effects of transcutaneous CO2 on blood flow and the capillaries result in enhanced supply of oxygen and nutrition to the skeletal muscles and most likely improve exercise endurance capacity, as a reduction in the density/quality of the capillary network leads to exercise intolerance.
References
Slopack D, Roudier E, Liu ST, Nwadozi E, Birot O, Haas TL (2014) Forkhead BoxO transcription factors restrain exercise-induced angiogenesis. J Physiol 592:4069–4082
Tanaka M, Kanazashi M, Kondo H, Ishihara A, Fujino H (2018) Protective effects of Brazilian propolis supplementation of capillary regression in the soleus muscle of hindlimb-unloading rats. J Physiol Sci. https://doi.org/10.1007/s12576-018-0639-z
Emanueli C, Salis MB, Pinna A, Stacca T, Milia AF, Spano A, Chao J, Chao L, Sciola L, Madeddu P (2002) Prevention of diabetes-induced microangiopathy by human tissue kallikrein gene transfer. Circulation 106:993–999
Thiruvoipati T (2015) Peripheral artery disease in patients with diabetes: epidemiology, mechanisms, and outcomes. World J Diabetes 6:961–969
Frier BC, Noble EG, Locke M (2008) Diabetes-induced atrophy is associated with a muscle-specific alteration in NF-κB activation and expression. Cell Stress Chaperones 13:287–296
Fortes MAS, Pinheiro CHJ, Guimarães-Ferreira L, Vitzel KF, Vasconcelos DAA, Curi R (2015) Overload-induced skeletal muscle hypertrophy is not impaired in STZ-diabetic rats. Physiol Rep. https://doi.org/10.14814/phy2.12457
Kivelä R, Silvennoinen M, Touvra AM, Lehti TM, Kainulainen H, Vihko V (2006) Effects of experimental type 1 diabetes and exercise training on angiogenic gene expression and capillarization in skeletal muscle. FASEB J 20:1570–1572
Kondo H, Fujino H, Murakami S, Nagatomo F, Roy RR, Ishihara A (2011) Regressed three-dimensional capillary network and inhibited angiogenic factors in the soleus muscle of non-obese rats with type 2 diabetes. Nutr Metab. https://doi.org/10.1186/1743-7075-8-77
Tadaishi M, Miura S, Kai Y, Kano Y, Oishi Y, Ezaki O (2011) Skeletal muscle-specific expression of PGC-1α-b, an exercise-responsive isoform, increases exercise capacity and peak oxygen uptake. PLoS ONE. https://doi.org/10.1371/journal.pone.0028290
Voltarelli VA, Bacurau AVN, Bechara LRG, Bueno Júnior CR, Bozi LHM, Mattos KC, Salemi VMC, Brum PC (2012) Lack of β2-AR improves exercise capacity and skeletal muscle oxidative phenotype in mice. Scand J Med Sci Sports 22:e125–e132
Olfert MI, Howlett RA, Tang K, Dalton ND, Gu Y, Peterson KL, Wagner PD, Breen EC (2009) Muscle-specific VEGF deficiency greatly reduces exercise endurance in mice. J Physiol 587:1755–1767
Lawler J (2002) Thrombospondin-1 as an endogenous inhibitor of angiogenesis and tumor growth. J Cell Mol Med. https://doi.org/10.1111/j.1582-4934.2002.tb00307.x
Tang K, Breen EC, Gerber HP, Ferrara NMA, Wagner PD (2004) Capillary regression in vascular endothelial growth factor-deficient skeletal muscle. Physiol Genom 18:63–69
Malek MH, Olfert IM (2009) Global deletion of thrombospondin-1 increases cardiac and skeletal muscle capillarity and exercise capacity in mice. Exp Physiol 94:749–760
Malek MH, Olfert IM, Esposito F (2010) Detraining losses of skeletal muscle capillarization are associated with vascular endothelial growth factor protein expression in rats. Exp Physiol 95:359–368
Lawler PR, Lawler J (2012) Molecular basis for the regulation of angiogenesis by thrombospondin-1 and-2. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a006627
Smadja DM, D’Audigier C, Bièche I, Evrard S, Mauge L, Dias JV, Labreuche J, Laurendeau I, Marsac B, Dizier B, Wagner-Ballon O, Boisson-Vidal C, Morandi V, Duong-Van-Huyen JP, Bruneval P, Dignat-George F, Emmerich J, Gaussem P (2011) Thrombospondin-1 is a plasmatic marker of peripheral arterial disease that modulates endothelial progenitor cell angiogenic properties. Arterioscler Thromb Vasc Biol 31:551–559
Roudier E, Milkiewicz M, Birot O, Slopack D, Montelius A, Gustafsson T, Paik JH, Depinho RA, Casale GP, Pipinos II, Haas TL (2013) Endothelial FoxO1 is an intrinsic regulator of thrombospondin 1 expression that restrains angiogenesis in ischemic muscle. Angiogenesis 16:759–772
Roudier E, Gineste C, Wazna A, Dehghan K, Desplanches D, Birot O (2010) Angio-adaptation in unloaded skeletal muscle: new insights into an early and muscle type-specific dynamic process. J Physiol 588:4579–4591
Kanazashi M, Okumura Y, Al-Nassan S, Murakami S, Kondo H, Nagatomo F, Fujita N, Ishihara A, Roy RR, Fujino H (2013) Protective effects of astaxanthin on capillary regression in atrophied soleus muscle of rats. Acta Physiol 207:405–415
Hirayama Y, Nakanishi R, Tategaki A, Maeshige N, Kondo H, Ishihara A, Roy RR, Fujino H (2017) Enterococcus faecium strain R30 increases red blood cell velocity and prevents capillary regression in the soleus of hindlimb-unloaded rats via the eNOS/VEGF pathway. Microcirculation. https://doi.org/10.1111/micc.12356
Kivelä R, Silvennoinen M, Lehti M, Jalava S, Vihko V, Kainulainen H (2008) Exercise-induced expression of angiogenic growth factors in skeletal muscle and in capillaries of healthy and diabetic mice. Cardiovasc Diabetol. https://doi.org/10.1186/1475-2840-7-13
Dunford EC, Leclair E, Aiken J, Mandel ER, Haas TL, Birot O, Riddell MC (2017) The effects of voluntary exercise and prazosin on capillary rarefaction and metabolism in streptozotocin-induced diabetic male rats. J Appl Physiol 122:492–502
Kondo H, Fujino H, Murakami S, Tanaka M, Kanazashi M, Nagatomo F, Ishihara A, Roy RR (2015) Low-intensity running exercise enhances the capillary volume and pro-angiogenic factors in the soleus muscle of type 2 diabetic rats. Muscle Nerve 51:391–399
Riggs A (1960) The nature and significance of the Bohr effect in mammalian hemoglobins. J Gen Physiol 43:737–752
Goodman M, Moore GW, Matsuda G (1975) Darwinian evolution in the genealogy of haemoglobin. Nature 253:603–608
Wells RMG (1999) Evolution of haemoglobin function: molecular adaptations to environment. Clin Exp Pharmacol Physiol 26:591–595
Hartmann BR, Bassenge E, Pittler M, Hartmann BR (1997) Effect of carbon dioxide-enriched water and fresh water on the cutaneous microcirculation and oxygen tension in the skin of the foot. Angiology 48:337–343
Jensen FB (2004) Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport. Acta Physiol Scand 182:215–227
Sakai Y, Miwa M, Oe K, Ueha T, Koh A, Niikura T, Iwakura T, Lee SY, Tanaka M, Kurosaka M (2011) A novel system for transcutaneous application of carbon dioxide causing an “artificial Bohr effect” in the human body. PLoS ONE. https://doi.org/10.1371/journal.pone.0024137
Izumi Y, Yamaguchi T, Yamazaki T, Yamashita N, Nakamura Y, Shiota M, Tanaka M, Sano S, Osada-Oka M, Shimada K, Wanibuchi H, Miura K, Yoshiyama M, Iwao H (2015) Percutaneous carbon dioxide treatment using a gas mist generator enhances the collateral blood flow in the ischemic hindlimb. J Atheroscler Thromb 22:38–51
Savin E, Bailliart O, Bonnin P, Bedu M, Cheynel J, Coudert J, Martineaud JP (1995) Vasomotor effects of transcutaneous CO2 in stage II peripheral occlusive arterial disease. Angiology 46:785–791
Harrison DG, Sayegh H, Ohara Y, Inoue N, Venema RC (1996) Regulation of expression of the endothelial cell nitric oxide synthase. Clin Exp Pharmacol Physiol 23:251–255
Fleming I, Busse R (2003) Molecular mechanisms involved in the regulation of the endothelial nitric oxide synthase. Am J Physiol Integr Comp Physiol 284:R1–R12
Baum O, Da Silva-Azevedo L, Willerding G, Wöckel A, Planitzer G, Gossrau R, Pries AR, Zakrzewicz A (2004) Endothelial NOS is main mediator for shear stress-dependent angiogenesis in skeletal muscle after prazosin administration. Am J Physiol Heart Circ Physiol 287:H2300–H2308
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC (1995) Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature 377:239–242
Duplain H, Burcelin R, Sartori C, Cook S, Egli M, Lepori M, Vollenweider P, Pedrazzini T, Nicod P, Thorens B, Scherrer U (2001) Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation 104:342–345
Vincent MA, Barrett EJ, Lindner JR, Clark MG, Rattigan S (2003) Inhibiting NOS blocks microvascular recruitment and blunts muscle glucose uptake in response to insulin. Am J Physiol Endocrinol Metab 285:E123–E129
Egginton S (2009) Invited review: activity-induced angiogenesis. Pflugers Arch Eur J Physiol 457:963–977
Vassilakopoulos T, Deckman G, Kebbewar M, Rallis G, Harfouche R, Hussain SNA (2003) Regulation of nitric oxide production in limb and ventilatory muscles during chronic exercise training. Am J Physiol Lung Cell Mol Physiol 284:L452–L457
Lee-Young RS, Ayala JE, Hunley CF, James FD, Bracy DP, Kang L, Wasserman DH (2010) Endothelial nitric oxide synthase is central to skeletal muscle metabolic regulation and enzymatic signaling during exercise in vivo. AJP Regul Integr Comp Physiol 298:R1399–R1408
Irie H, Tatsumi T, Takamiya M, Zen K, Takahashi T, Azuma A, Tateishi K, Nomura T, Hayashi H, Nakajima N, Okigaki M, Matsubara H (2005) Carbon dioxide-rich water bathing enhances collateral blood flow in ischemic hindlimb via mobilization of endothelial progenitor cells and activation of NO-cGMP system. Circulation 111:1523–1529
Oe K, Ueha T, Sakai Y, Niikura T, Lee SY, Koh A, Hasegawa T, Tanaka M, Miwa M, Kurosaka M (2011) The effect of transcutaneous application of carbon dioxide (CO2) on skeletal muscle. Biochem Biophys Res Commun 407:148–152
Milkiewicz M, Roudier E, Doyle JL, Trifonova A, Birot O, Haas TL (2011) Identification of a mechanism underlying regulation of the anti-angiogenic forkhead transcription factor FoxO1 in cultured endothelial cells and ischemic muscle. Am J Pathol 178:935–944
Roudier E, Forn P, Perry ME, Birot O (2012) Murine double minute-2 expression is required for capillary maintenance and exercise-induced angiogenesis in skeletal muscle. FASEB J 26:4530–4539
Bongrazio M, Da Silva-Azevedo L, Bergmann EC, Baum O, Hinz B, Pries AR, Zakrzewicz A (2006) Shear stress modulates the expression of thrombospondin-1 and CD36 in endothelial cells in vitro and during shear stress-induced angiogenesis in vivo. Int J Immunopathol Pharmacol 19:35–48
Fujino H (2005) Regression of capillary network in atrophied soleus muscle induced by hindlimb unweighting. J Appl Physiol 98:1407–1413
Tanaka M, Kanazashi M, Maezawa T, Kondo H, Fujino H (2015) Abnormalities in three-dimensional capillary architecture and imbalance between vascular endothelial growth factor-A and thrombospondin-1 in soleus muscle of ovariectomized rat. Acta Histochem 117:605–611
Rohra DK (2003) Effects of changes in pH on the contractility of vascular smooth muscle. J Coll Physicians Surg Pak 13:544–548
Zsother T, Banderman L, Chappel CL (1961) The effects of “local” pH changes on blood flow in the dog. Am Heart J 61:777–782
Kellum JA (2000) Determinants of blood pH in health and disease. Crit Care 4(1):6
Charter ME, Lamb IR, Murrant CL (2018) Arteriolar and capillary responses to CO2 and H+ in hamster skeletal muscle microvasculature: implications for active hyperemia. Microcirculation. https://doi.org/10.1111/micc.12493
Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L (2006) VEGF receptor signalling? In control of vascular function. Nat Rev Mol Cell Biol 7:359–371
Wagner PD (2011) The critical role of VEGF in skeletal muscle angiogenesis and blood flow. Biochem Soc Trans 39:1556–1559
Delavar H, Nogueira L, Wagner PD, Hogan MC, Metzger D, Breen EC (2014) Skeletal myofiber VEGF is essential for the exercise training response in adult mice. AJP Regul Integr Comp Physiol 306:R586–R595
Duling BR (1973) Changes in microvascular diameter and oxygen tension induced by carbon dioxide. Circ Res 32:370–376
Graubert MD, Ortega MA, Kessel B, Mortola JF, Iruela-Arispe ML (2001) Vascular repair after menstruation involves regulation of vascular endothelial growth factor-receptor phosphorylation by sFLT-1. Am J Pathol 158:1399–1410
Greenaway J, Gentry PA, Feige JJ, LaMarre J, Petrik JJ (2005) Thrombospondin and vascular endothelial growth factor are cyclically expressed in an inverse pattern during bovine ovarian follicle development. Biol Reprod 72:1071–1078
Olfert IM, Howlett RA, Wagner PD, Breen EC, Virginia W (2010) Myocyte vascular endothelial growth factor is required for exercise-induced skeletal muscle angiogenesis. Am J Physiol 299:1059–1067
Gorman JL, Liu STK, Slopack D, Shariati K, Hasanee A, Olenich S, Olfert IM, Haas TL (2014) Angiotensin II evokes angiogenic signals within skeletal muscle through co-ordinated effects on skeletal myocytes and endothelial cells. PLoS ONE. https://doi.org/10.1371/journal.pone.0085537
Uchida C, Nwadozi E, Hasanee A, Olenich S, Olfert IM, Haas TL (2015) Muscle-derived vascular endothelial growth factor regulates microvascular remodelling in response to increased shear stress in mice. Acta Physiol 214:349–360
Lee S, Chen TT, Barber CL, Jordan MC, Murdock J, Desai S, Ferrara N, Nagy A, Roos KP, Iruela-Arispe ML (2007) Autocrine VEGF signaling is required for vascular homeostasis. Cell 130:691–703
Kanazashi M, Tanaka M, Murakami S, Kondo H, Nagatomo F, Ishihara A, Roy RR, Fujino H (2014) Amelioration of capillary regression and atrophy of the soleus muscle in hindlimb-unloaded rats by astaxanthin supplementation and intermittent loading. Exp Physiol 99:1065–1077
Olfert IM (2016) Physiological capillary regression is not dependent on reducing VEGF expression. Microcirculation 23:145–156
Audet GN, Fulks D, Stricker JC, Olfert IM (2013) Chronic delivery of a thrombospondin-1 mimetic decreases skeletal muscle capillarity in mice. PLoS ONE. https://doi.org/10.1371/journal.pone0055953
Zhang Y, Liao B, Li M, Cheng M, Fu Y, Liu Q, Chen Q, Liu H, Fang Y, Zhang G, Yu F (2016) Shear stress regulates endothelial cell function through SRB1-eNOS signaling pathway. Cardiovasc Ther 34:308–313
Metaxa E, Meng H, Kaluvala SR, Szymanski MP, Paluch RA, Kolega J (2008) Nitric oxide-dependent stimulation of endothelial cell proliferation by sustained high flow. Am J Physiol Heart Circ Physiol 295:H736–H742
Shangary S, Wang S (2008) Targeting the MDM2-p53 interaction for cancer therapy. Clin Cancer Res 14:5318–5324
Hudlicka O, Brown MD, May S, Zakrzewicz A, Pries AR (2006) Changes in capillary shear stress in skeletal muscles exposed to long-term activity: role of nitric oxide. Microcirculation 13:249–259
Rivilis I, Milkiewicz M, Boyd P, Goldstein J, Brown MD, Egginton S, Hansen FM, Hudlica O, Haas TL (2002) Differential involvement of MMP-2 and VEGF during muscle stretch-versus shear stress-induced angiogenesis. Am J Physiol Heart Circ Physiol 283:H1430–H1438
Hudlicka O, Brown MD (2009) Adaptation of skeletal muscle microvasculature to increased or decreased blood flow: role of shear stress, nitric oxide and vascular endothelial growth factor. J Vasc Res 46:504–512
Acknowledgements
The study was supported by Grants-in-Aid for Scientific Research (No. 16H03208) from the Japanese Ministry of Education, Culture, Sports, Science and Technology.
Author information
Authors and Affiliations
Contributions
TM, MT, TI, and HF conceived and designed the experiments. TM, MT and TI performed the experiments. MT, TI and HF analyzed the data. MT, NM, YS, TA, HK, AI and HF contributed by providing regents, materials and analysis tools. TM, MT, TI, HK, AI and HF interpreted the data and wrote the paper. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. This article does not contain any studies with human participants performed by any of the authors.
About this article
Cite this article
Matsumoto, T., Tanaka, M., Ikeji, T. et al. Application of transcutaneous carbon dioxide improves capillary regression of skeletal muscle in hyperglycemia. J Physiol Sci 69, 317–326 (2019). https://doi.org/10.1007/s12576-018-0648-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-018-0648-y