Abstract
Purpose
The aim of this study is to identify and assess evidence related to the efficacy of mind–body interventions on irritable bowel syndrome (IBS) in the Chinese population.
Method
Drawn from Chinese databases, nine RCTs and three Q-E studies were included in the systematic review. The methodological quality of RCTs was evaluated based on the following criteria: adequate sequence generation, allocation concealment, blinding, completeness of outcome data, selective reporting, and other potential biases. For continuous variables, the effect size (ES) was determined by calculating the standardized mean difference between groups. For dichotomous variables, the ES was determined by calculating the risk ratio (RR) between groups. Given the heterogeneity between the trials and the small number of studies included, both random effects and fixed effects models were used. The inverse variance method was used for pooling. Statistical analyses were performed using Review Manager version 5.0.
Results
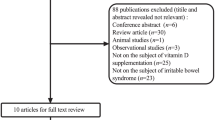
The total number of papers identified was 710: 462 from English language databases and 248 from Chinese language databases. Twelve studies met our eligibility criteria. Among the studies selected, three were Q-E studies the rest RCTs. Two studies described the randomization process. None of the studies reported allocation concealment nor blinding. Seven studies reported no dropouts. One of the studies mentioned the total amount of dropouts; though the reason for dropping out was not referenced. The other four studies did not clearly report dropouts. With the exception of three studies, there was inadequate information to determine biased reporting for the majority; the level of risk for bias in these studies is unclear. Finally, six meta-analyses were performed. One was conducted with four randomized controlled trials (RCTs) that used cure rate as outcome measures to evaluate gastrointestinal (GI) symptoms, which suggested that mind–body interventions were effective in improving GI symptoms (random effects model: RR = 1.08; 95 % CI 1.01 to 1.17; fixed effects model: RR = 1.07; 95 % CI 1.01 to 1.12). The remaining five were conducted in three RCTs, which suggested that mind–body interventions were effective in improving several aspects of quality of life, including interference with activity (random effects and fixed effects models: SMD = 0.64; 95 % CI 0.41 to 0.86), body image (random effects model: SMD = 0.36; 95 % CI 0.06 to 0.67; fixed effects model: SMD = 0.33; 95 % CI 0.11 to 0.55), health worry (random effects and fixed effects models: SMD = 0.67; 95 % CI 0.44 to 0.90), food avoidance (random effects and fixed effects models: SMD = 0.45; 95 % CI 0.23 to 0.68), and social reaction (random effects model: SMD = 0.79; 95 % CI 0.47 to 1.12; fixed effects model: SMD = 0.78; 95 % CI 0.55 to 1.01), as measured by Irritable Bowel Syndrome Quality of Life Questionnaire ( IBS-QOL).
Conclusion
Mind–body interventions may have the potential to improve GI symptoms in Chinese patients with IBS. The improvement of GI symptoms was also accompanied with the improvement of various outcomes, including depression, anxiety, and quality of life, just to mention a few. However, the published studies generally had significant methodological limitations. Future clinical trials with rigorous research design are needed in this field. More studies focusing on the mind–body interventions originated in China, such as tai chi and qi gong should be encouraged.



Similar content being viewed by others
References
Pan G, Lu S, Ke M, Han S, Guo H, Fang X. Anepidemiologic study of irritable bowel syndrome in Beijing—a stratified randomized study by clustering sampling. Zhonghua Liu Xing Bing Xue Za Zhi. 2000;21:26–9.
Xiong LS, Chen MH, Chen HX, Xu AG, Wang WA, Hu PJ. A population-based epidemiologic study of irritable bowel syndrome in South China: stratified randomized study by cluster sampling. Aliment Pharmacol Ther. 2004;19:1217–24.
Zhang L, Duan L, Liu Y, Leng Y, Zhang H, Liu Z, et al. A meta-analysis of the prevalence and risk factors of irritable bowel syndrome in Chinese community. Zhonghua Nei Ke Za Zhi. 2014;53(12):969–75.
Lau EM, Chan FK, Ziea ET, Chan CS, Wu JC, Sung JJ. Epidemiology of irritable bowel syndrome in Chinese. Dig Dis Sci. 2002;47(11):2621–4.
Rey E, Talley NJ. Irritable bowel syndrome: novel views on the epidemiology and potential risk factors. Dig Liver Dis. 2009;41:772–80.
Hayee B, Forgacs I. Psychological approach to managing irritable bowel syndrome. BMJ. 2007;334(7603):1105–9.
Medicine NCfCaA. What is complementary and alternative medicine? 2015. Available from: https://www.nccih.nih.gov/video/series/mindbody. Modified 8 Jan 2015.
National Center of Complementary and Alternative Medicine. CAM basics. Online document.[cited 2010 Feb 23]. Available from: http://nccam.nih.gov/health/whatiscam/D347.pdf/.
Cuellar NG. Hypnosis for pain management in the older adult. Pain Manag Nurs. 2005;6:105–11.
Hutton J. Cognitive behaviour therapy for irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2005;17:11–4.
Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31.
Tsiros MD, Sinn N, Brennan L, Coates AM, Walkley JW, Petkov J, et al. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr. 2008;87:1134–40.
Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007;127:276–86.
Kabat-Zinn J. Commentary on Majumdar et al.: mindfulness meditation and health. J Altern Complement Med. 2002;8:731–5.
Wayne PM, Kaptchuk TJ. Challenges inherent to t’ai chi research: part II—defining the intervention and optimal study design. J Altern Complement Med. 2008;14:191–7.
Rogers CE, Larkey LK, Keller C. A review of clinical trials of tai Chi and Qigong in older adults. Western J Nurs Res. 2009;31(2):245–79.
Sancier K, Holman D. Multifaceted health benefits of medical qigong. J Altern Complement Med. 2004;10(1):163–6.
Sancier KM. Therapeutic benefits of qigong exercises in combination with drugs. J Altern Complement Med. 1999;5(4):383–9.
Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States. Natl Health Stat Report. 2008;12:1–23.
Bernstein D, Borkovec T, Carlson K. Progressive relaxation training: a manual for the helping profession. Mashhad: Ferdowsi University Press; 1992.
Durand, VM, Barlow D. Abnormal psychology: an integrative approach. Belmont, CA: Wadsworth Cengage Learning. 2009; 331.
Kim JK, Jeon BG, Song YS, Seo MS, Kwon YH, Park JW, et al. Biofeedback therapy before ieostomy closure in patients undergoing sphincter-saving surgery for rectal cancer: a pilot study. Ann Coloproctol. 2015;31(4):138–43.
Linnemann A, Kappert MB, Fischer S, Doerr JM, Strahler J, Nater UM. The effects of music listening on pain and stress in the daily life of patientss with fibromyalgia syndrome. Front Hum Neurosci. 2015;9:434.
Roberts L, Wilson S, Singh S, Roalfe A, Greenfield S. Gut-directed hypnotherapy for irritable bowel syndrome: piloting a primary care-based randomised controlled trial. Br J Gen Pract. 2006;56(523):115–21.
Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007;133(5):1430–6.
Gonsalkorale WM, Miller V, Afzal A, Whorwell PJ. Long term benefits of hypnotherapy for irritable bowel syndrome. Gut. 2003;52(11):1623–9.
Kennedy T, Jones R, Darnley S, Seed P, Wessely S, Chalder T. Cognitive behaviour therapy in addition to antispasmodic treatment for irritable bowel syndrome in primary care: randomised controlled trial. BMJ. 2005;331(7514):435.
Webb AN, Kukuruzovic RH, Catto-Smith AG, Sawyer SM. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2007;4(4):CD005110.
Li CY, Li SC. Treatment of irritable bowel syndrome in China: a review. World J Gastroenterol. 2015;21(8):2315–22.
Grundmann O, Yoon SL. Complementary and alternative medicines in irritable bowel syndrome: an integrative view. World J Gastroenterol. 2014;20(2):346–62.
Lee HH, Choi YY, Choi MG. The efficacy of hypnotherapy in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. J Neurogastroenterol Motil. 2014; 3020(2):152–62.
Aucoin M, Lalonde-Parsi MJ, Cooley K. Mindfulness-based therapies in the treatment of functional gastrointestinal disorders: a meta-analysis. Evid Based Complement Alternat Med. 2014. doi:10.1155/2014/140724.22.
Lakhan SE, Schofield KL. Mindfulness-based therapies in the treatment of somatization disorders: a systematic review and meta-analysis. PLoS One. 2013;8(8):e71834.
Altayar O, Sharma V, Prokop LJ, Sood A, Murad MH. Psychological therapies in patients with irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Gastroenterol Res Pract. 2015;2015:549308.
Liu B, Zhang Y, Xue C, Jin S. Effects of simple cognitive behavioral therapy on patients with irritable bowel syndrome. Chin J Coal Ind Med. 2004;7(2):137–8.
Qi H, Xu D. Effects of Shuang Xiang ping Heng therapy on 87 patients with irritable bowel syndrome. J New Chin Med. 2002;34(7):23–4.
Zheng Y, Hong Q, Wang H, Zhou L. Effects of music therapy and psychotherapy cognitive behavioral therapy on patients with irritable bowel syndrome. Chin J Clin Rehabil. 2003;7(24):3382–3.
Chi D. Study of cognitive characteristics, and effects of cognitive behavioral therapy on cognitions, emotions, and symptom severity of IBS-D patients[MS Dissertation].China Medical University; 2009.
Feng Y, Bian B, Pan H, Chen C, Chen C. Effects of Baduanjin on older adults with constipation-predominant irritable bowel syndrome. Sport Sci Res. 2010;31(2):89–90,98.
Li C, Feng H, Xiao S, Huang H. The influence of tai Ji on the therapeutic effect for irritable bowel syndrome. JPMT. 2008;15(11):1384–6.
Li H. Cognitive behavior therapy for the treatment of patients with IBS. [MS Dissertation]. The Second Military Medical University; 2011.
Shao Y, Xia J, Wang X. Curative effects of pinaverium bromide combined with venlafaxine or cognitive behavioral group therapy on patients with irritable bowel syndrome. Chin J New Drugs Clin Rem. 2008;27(2):101–5.
Xiong Y. Effect of progressive muscle relaxation training on patients with irritable bowel syndrome. Chin J Mod Nurs. 2008;14(21):2263–5.
Zhao J, Mi Y, Dong Y. Clinical observation of electromyographic biofeedback on irritable bowel syndrome. J Southeast Univ (Med Sci Edi). 2011;30(6):873–6.
Zhao Y, Sun H, Xu G, Dai L, Gao Z, Ji W, et al. The influence of hypnotherapy on mental health, quality of life and clinical efficacy of patients with irritable bowel syndrome. Chin J Behav Med Brain Sci. 2009;18(12):1106–8.
Chen L. The influence of gut-directed hypnotherapy on quality of life and clinical efficacy of patients with irritable bowel syndrome. Chin J Prev Contr Chron Dis. 2013;21(1):74–6.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Yang K. How to write a systematic review. Beijing: People’s Medical Publishing House; 2010.
Cohen J. A coefficient of agreement for nominal scales. Educ Educ Psychol Meas. 1960;20:37–346.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso-Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol. 2011;64(12):1311–6.
Blanchard EB, Lackner J, Jaccard J, Rowell D, Carosella AM, Powell C. The role of stress in symptom exacerbation among IBS patients. J Psychosom Res. 2008;64(2):119–28.
Mason S, Tovey P, Long AF. Evaluating complementary medicine: methodological challenges of randomized controlled trials. BMJ. 2002;325(7368):832–4.
Caspi O, Burleson KO. Methodological challenges in meditation research. Adv Mind Body Med. 2005;21:4–11.
Akehurst R, Kaltenthaler E. Treatment of irritable bowel syndrome: a review of randomised controlled trials. Gut. 2001;48:272–82.
Brandt LJ, Bjorkman D, Fennerty MB, Locke GR, Olden K, Peterson W, et al. Systematic review on the management of irritable bowel syndrome in North America. Am J Gastroenterol. 2002;97:S7–26.
Tack J, Fried M, Houghton LA, Spicak J, Fisher G. Systematic review: the efficacy of treatments for irritable bowel syndrome – a European perspective. Aliment Pharmacol Ther. 2006;24:183–205.
Daley AJ, Grimmett C, Roberts L, Wilson S, Fatek M, Roalfe A, Singh S. The effects of exercise upon symptoms and quality of life in patients diagnosed with irritable bowel syndrome: a randomised controlled trial. Int J Sports Med. 2008;29:778–82.
Kim YJ, Ban DJ. Prevalence of irritable bowel syndrome, influence of lifestyle factors and bowel habits in Korean college students. Int J Nurs Stud. 2005;42:247–54.
Villoria A, Serra J, Azpiroz F, Malagelada JR. Physical activity and intestinal gas clearance in patients with bloating. Am J Gastroenterol. 2006;101:2552–7.
Lustyk MK, Jarrett ME, Bennett JC, Heitkemper MM. Does a physically active lifestyle improve symptoms in women with irritable bowel syndrome? Gastroenterol Nurs. 2001;24:129–37.
Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2011;106:915–22.
Berrill JW, Sadlier M, Hood K, Green JT. Mindfulness-based therapy for inflammatory bowel disease patients with functional abdominal symptoms or high perceived stress levels. J Crohns Colitis. 2014;8(9):945–55.
Zernicke KA, Campbell TS, Blustein PK, Fung TS, Johnson JA, Bacon SL, et al. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: a randomized wait-list controlled trial. Curr Gastroenterol Rep. 2012;14(4):283–9.
Keefer L, Blanchard EB. A one year follow-up of relaxation response meditation as a treatment for irritable bowel syndrome. Behav Res Ther. 2002;40(5):541–6.
Larkey LK, Roe DJ, Weihs KL, Jahnke R, Lopez AM, Rogers CE, et al. Randomized controlled trial of qigong/tai Chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med. 2015;49(2):165–76.
Evans S, Lung KC, Seidman LC, Sternlieb B, Zeltzer LK, Tsao JC. Iyengar yoga for adolescents and young adults with irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 2014;59(2):244–53.65.
Taneja I, Deepak KK, Poojary G, Acharya IN, Pandey RM, Sharma MP. Yogic versus conventional treatment in diarrhea-predominant irritable bowel syndrome: a randomized control study. Appl Psychophysiol Biofeedback. 2004;29(1):19–33.66.
Kuttner L, Chambers CT, Hardial J, Israel DM, Jacobson K, Evans K. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain Res Manag. 2006;11(4):217–23.
Acknowledgments
Research was partly funded by the following project: Clinical Evaluation in the Treatment of Depression with the Combination of Disease and Syndrome”-Projects in the National Science& Technology Pillar Program during the Twelfth Five-Year Plan Period, Ministry of Science and Technology of the People’s Republic of China (grant number2014BAI10B07).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Wang W, Wang F, Feng F, Sedas AC, and Wang J declare that they have no conflict of interest. They conformed to the Helsinki Declaration concerning human rights and informed consent, and they followed correct procedures concerning treatment of humans and animals in research. Each author’s contribution to this manuscript is as follows: Wang W designed the study. Wang F, Feng F and Wang J conducted the research. Wang F performed the meta-analysis and wrote the manuscript. Sedas AC proofread the manuscript. Wang W obtained funding from the Ministry of Science and Technology of the People’s Republic of China for the study.
Rights and permissions
About this article
Cite this article
Wang, W., Wang, F., Fan, F. et al. Mind–Body Interventions for Irritable Bowel Syndrome Patients in the Chinese Population: a Systematic Review and Meta-Analysis. Int.J. Behav. Med. 24, 191–204 (2017). https://doi.org/10.1007/s12529-016-9589-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-016-9589-0