Abstract
Background
Down syndrome (DS) is the most common chromosomal disorder that causes mental retardation. In 2009, a population-based birth defects study was implemented in three provinces in southern Thailand. This study aimed to determine the prevalence of DS in the studied regions, and the proportion of DS fetuses detected by prenatal screening.
Methods
Data were obtained from a population-based surveillance study undertaken during 2009-2013. Entries in the birth defects registry included live births, stillbirths after 24 weeks gestational age, and terminations of pregnancy following prenatal diagnosis. Infants with clinical characteristics of DS had a chromosomal study to make a definite diagnosis.
Results
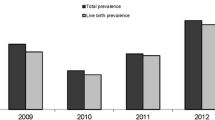
Of the total 186 393 births recorded during the study period, 226 DS cases were listed, giving a prevalence of 1.21 per 1000 births [95% confidence interval (CI) 1.05-1.37]. The median maternal age was 36.5 years with a percentage of maternal age ≥35 years of 60.6%. Seventy-seven cases (34.1% of all cases) were diagnosed prenatally and these pregnancies were terminated. The prevalence of DS per 1000 births was significantly higher in older women, from 0.47 (95% CI 0.28-0.67) in mothers aged <30 years to 0.88 (95% CI 0.59-1.17) in mothers 30-<35 years (P<0.01), and to 4.74 (95% CI 3.95-5.53) in mothers ≥35 years (P<0.001).
Conclusions
The prevalence of DS significantly increased with maternal age. About 35% of DS cases were detected prenatally and later terminated. Hence, examining only registry live births will result in an inaccurate prevalence rate of DS.
Similar content being viewed by others
References
Boyd PA, Khoshnood B, Loane M, Garne E, Dolk H, and the EUROCAT working group. Survey of prenatal screening in Europe for structural malformations and chromosome anomalies, and their impact on detection and termination rates for neural tube defects and Down’s syndrome. BJOG 2008;115:689–696.
Loane M, Morris JK, Addor M-C, Arriola L, Budd J, Doray B, et al. Twenty-year trends in the prevalence of Down syndrome and other trisomies in Europe: impact of maternal age and prenatal screening. Eur J Hum Genet 2012;21:27–33.
Savva GM, Walker K, Morris JK. The maternal age-specific live birth prevalence of trisomies 13 and 18 compared to trisomy 21 (Down syndrome). Prenat Diag 2009;30:57–64.
Cocchi G, Gualdi S, Bower C, Halliday J, Jonsson B, Myrelid A, et al. International trends of Down syndrome 1993-2004: births in relation to maternal age and terminations of pregnancies. Birth Defects Res (Part A) 2010;88:474–479.
Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res (Part A) 2010;88:1008–1016.
Wellesley D, Dolk H, Boyd PA, Greenlees R, Haeusler M, Nelen V, et al. Rare chromosome abnormalities, prevalence and prenatal diagnosis rates from population-based congenital anomaly registers in Europe. Eur J Hum Genet 2012;20:521–526.
Jou HJ, Kuo YS, Hsu JJ, Shyu MK, Hsieh TT, Hsieh FJ. The evolving national birth prevalence of Down syndrome in Taiwan. A study on the impact of second-trimester maternal serum screening. Prenat Diag 2005;25:665–670.
Wang YY, Luo J, Zhu MW, Liu LN, Ma X. Second-trimester double or triple screening for Down syndrome: a comparison of Chinese and Caucasian populations. Int J Gynecol Obstet 2006;94:67–72.
Leung TY, Chan LW, Leung TN, Fung TY, Sahota DS, Spencer K, et al. First-trimester combined screening for trisomy 21 in a predominantly Chinese population. Ultrasound Obstet Gynecol 2007;29:14–17.
Takeuchi A, Ehara H, Ohtani K, Maegaki Y, Nanba Y, Nagata I, et al. Live birth prevalence of Down syndrome in Tottori, Japan 1980-1999. Am J Med Genet Part A 2008;146A:1381–1386.
Siripoonya P, Tejavej A. Congenital abnormalities in the early neonatal period: ten years incidence at Ramathibodi Hospital. J Med Assoc Thai 1980;63:544–547.
Dissaneevate S, Jaruratanasirikul S, Chanvitan P, Janjindamai W. Congenital malformations of newborns at Songklanagarind Hospital. Songkla Med J 2003;21:267–276.
Hanprasertpong T, Kor-anantakul O, Prasartwanakit V, Leetanaporn R, Suntharasaj T, Suwanrath C. Outcome of second trimester amniocentesis in singleton pregnancy at Songklanagarind Hospital. J Med Assoc Thai 2011;94:1288–1292.
Pruksanusak N, Suwanrath C, Kor-anantakul O, Prasartwanakit V, Leetanaporn R, Suntharasuj T, et al. A survey of the knowledge and attitudes of pregnant Thai women towards Down syndrome screening. J Obstet Gynecol Res 2009;35:876–881.
Mason CA, Kirby RS, Sever LE, Langlois PH. Prevalence is the preferred measure of frequency of birth defect. Birth Defects Res A Clin Mol Teratol 2005;73:690–692.
Statistical Forecasting Bureau, National Statistical Office, Ministry of Information and Communication Technology, Thailand. Key Statistics of Thailand 2012. [internet]. Available from http://service.nso.go.th/nso/nsopublish/pubs/pubsfiles/Key55_T.pdf (accessed September 14, 2014).
Kajii T. Predicted prevalence of Down syndrome live births in Japan 1970-2006. Am J Med Genet A 2008;146A:1387–1388.
Breart G. Delayed childbearing. Eur J Obstet Gynecol Reprod Biol 1997;75:71–73.
Olsen CL, Cross PK, Gensburg LJ. Down syndrome: interaction between culture, demography, and biology in determining the prevalence of a genetic trait. Hum Biol 2003;75:503–520.
Shin M, Besser LM, Kucik JE, Lu C, Siffel C, Correa A. Prevalence of Down syndrome among children and adolescents in 10 regions of the United States. Pediatrics 2009;124:1565–1571.
Adams M, Erickson J, Layde P, Oakley G. Down’s syndrome recent trends in the United States. JAMA 1981;246:758–776.
Nagaishi M, Yamamoto T, Iinuma K, Shimomura K, Berend SA, Knops J. Chromosome abnormalities identified in 347 spontaneous abortions collected in Japan. J Obstet Gynecol Res 2004;90:237–241.
Menasha J, Levy B, Hirschhorn K, Kardon NB. Incidence and spectrum of chromosome abnormalities in spontaneous abortions: new insights from a 12-year study. Genet Med 2005;7:251–263.
Lai FM, Woo BH, Tan KH, Huang J, Lee ST, Yan TB, et al. Birth prevalence of Down syndrome in Singapore from 1993 to 1998. Singapore Med J 2002.43:70–76.
Hillman SC, McMullan DJ, Hall G, Togneri FS, James N, Maher EJ, et al. Use of prenatal chromosomal microarray: prospective cohort study and systematic review and meta-analysis. Ultrasound Obstet Gynecol 2013;41:610–620.
Lau TK, Cheung SW, Lo PS, Pursley AN, Chan MK, Jiang F, et al. Non-invasive prenatal testing for fetal chromosomal abnormalities by low-coverage whole genome sequencing of maternal plasma DNA: review of 1982 consecutive cases in a single center. Ultrasound Obstet Gynecol 2014;43:254–264.
Wax JR, Cartin A, Chard R, Lucas L, Pinette MG. Noninvasive prenatal testing: impact on genetic counseling, invasive prenatal diagnosis and trisomy 21 detection. J Clin Ultrasound 2014;43:1–6.
Acknowledgements
This research was supported by the Birth Defects Association (Thailand) and the Thai Health Promotion Foundation. The authors gratefully thank the staff of the 466 hospitals for their assistance with data collection. The authors thank Mr. David Patterson from the International Affairs Office in the Faculty of Medicine, Prince of Songkla University, for editorial help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jaruratanasirikul, S., Kor-anantakul, O., Chowvichian, M. et al. A population-based study of prevalence of Down syndrome in Southern Thailand. World J Pediatr 13, 63–69 (2017). https://doi.org/10.1007/s12519-016-0071-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-016-0071-5