Abstract
Noninvasive assessment with a technique such as single-photon emission computed tomography (SPECT) or positron emission tomography (PET) myocardial perfusion imaging (MPI) is common and appropriate before coronary angiography to define coronary anatomy. The diagnostic accuracy of these techniques has been extensively studied with over well over 100 publications reporting the sensitivity, specificity, area under the receiver operating characteristic curve, and diagnostic odds ratio for identifying coronary artery disease with both of them throughout their evolution. Meta-analytic techniques have emerged to combine diagnostic accuracy studies while retaining the 2-dimensional value of sensitivity and specificity data. Recent diagnostic accuracy meta-analyses estimated sensitivity and specificity for SPECT for coronary artery disease at 85 %–88 % and 76 %–85 %, respectively, and the corresponding values for PET at 90 %–92 % and 81 %–88 %. These meta-analytic estimates will be reviewed along with areas of ongoing work with myocardial blood flow measurement and hybrid SPECT/CT and PET/CT imaging systems that will continue improve the diagnostic performance of nuclear techniques.








Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levine GN, Bates ER, Blankenship JC, et al. ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice guidelines and the society for cardiovascular angiography and interventions. J Am Coll Cardiol. 2011;58:e44–122.
Altman DG, Bland JM. Statistics notes. Diagnostic tests 1: sensitivity and specificity. BMJ. 1994;308:1552.
Altman DG, Bland JM. Statistics notes. Diagnostic tests 3: receiver operating characteristic plots. BMJ. 1994;309:188.
Mallett S, Halligan S, Thompson M, Collins GS, Altman DG. Interpreting diagnostic accuracy studies for patient care. BMJ. 2012;345:e3999.
White CW, Wright CB, Doty DB, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med. 1984;310:819–24.
Fleming RM, Kirkeeide RL, Smalling RW, Gould KL. Patterns in visual interpretation of coronary arteriograms as detected by quantitative coronary arteriography. J Am Coll Cardiol. 1991;18:945–51.
Vas R, Eigler N, Miyazono C, et al. Digital quantification eliminates intra-observer and inter-observer variability in the evaluation of coronary artery stenosis. Am J Cardiol. 1985;56:718–23.
Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;63:380–406.
Gould KL, Johnson NP, Bateman TM, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62:1639–53. Comprehensive review of physiologic, vs anatomic, assessment of coronary artery disease.
De Bruyne B, Baudhuin T, Melin JA, et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation. 1994;89:1013–22.
Pijls NHJ, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenosis. N Engl J Med. 1996;334:1703–8.
Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354–67.
Tonino PAL, De Bruyne B, Pijls NHJ, et al. Fractional flow reserve vs angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356:830–40.
Begg CB, Greenes RA. Assessment of diagnostic tests when disease verification is subject to selection bias. Biometrics. 1983;39:207–15.
de Groot JAH, Dendukuri N, Janssen KJM, et al. Adjusting for partial verification or workup bias in meta-analyses of diagnostic accuracy studies. Am J Epidemiol. 2012;175:847–53.
Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Whiting P, Rutjes AWS, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Trikalinos TA, Balion CM, et al. Chapter 8: meta-analysis of test performance when there is a “gold standard”. J Gen Intern Med. 2012;27 Suppl 1:S56–66.
Reitsma JB, Glas AS, Rutjes AWS, et al. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–90.
Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging–executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). J Am Coll Cardiol. 2003;42:1318–33.
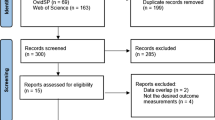
Health Quality Ontario. Single photon emission computed tomography for the diagnosis of coronary artery disease: an evidence-based analysis. Ont Health Technol Assess Ser. 2010;10:1–64.
Schünemann HJ, Schünemann AHJ, Oxman AD, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008;336:1106–10.
Ladapo JA, Blecker S, Elashoff MR, et al. Clinical implications of referral bias in the diagnostic performance of exercise testing for coronary artery disease. J Am Heart Assoc. 2013;2:e000505.
Zhou T, Yang L-F, Zhai J-L, et al. SPECT myocardial perfusion versus fractional flow reserve for evaluation of functional ischemia: a meta-analysis. Eur J Radiol. 2014;83:951–6.
Beanlands RSB, Youssef G. Diagnosis and prognosis of coronary artery disease: PET is superior to SPECT: Pro. J Nucl Cardiol. 2010;17:683–95.
Nandalur KR, Dwamena BA, Choudhri AF, et al. Diagnostic performance of positron emission tomography in the detection of coronary artery disease: a meta-analysis. Acad Radiol. 2008;15:444–51.
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Berman DS, Kang X, Slomka PJ, et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;14:521–8.
Ziadi MC, deKemp RA, Williams K, et al. Does quantification of myocardial flow reserve using rubidium-82 positron emission tomography facilitate detection of multi-vessel coronary artery disease? J Nucl Cardiol. 2012;19:670–80.
Fiechter M, Ghadri JR, Gebhard C, et al. Diagnostic value of 13N-ammonia myocardial perfusion PET: added value of myocardial flow reserve. J Nucl Med. 2012;53:1230–4. Myocardial flow reserve calculation in addition to PET MPI dramatically improved sensitivity for detecting significant CAD in 73 patients from 79% to 96% without loss of specificity of the test.
Heijenbrok-Kal MH, Fleischmann KE, Hunink MGM. Stress echocardiography, stress single-photon-emission computed tomography and electron beam computed tomography for the assessment of coronary artery disease: a meta-analysis of diagnostic performance. Am Heart J. 2007;154:415.
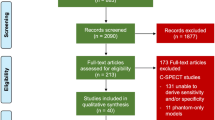
Parker MW, Iskandar A, Limone B, et al. Diagnostic accuracy of cardiac positron emission tomography vs single photon emission computed tomography for coronary artery disease: a bivariate meta-analysis. Circ Cardiovasc Imaging. 2012;5:700–7. Large and rigorous meta-analysis of the diagnostic accuracy of SPECT and PET; analyzed SPECT MPI in 11,212 patients and PET MPI in 650 patients to estimate sensitivity and specificity of SPECT at 88% and 76%, respectively, compared with 92% and 81% for PET.
McArdle BA, Dowsley TF, deKemp RA, Wells GA, Beanlands RS. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease? A systematic review and meta-analysis. J Am Coll Cardiol. 2012;60:1828–37. Thorough modern meta-analysis of Tc-99m SPECT with attenuation correction and ECG-gating in 1755 patients compared with Rb-82 PET in 1344 patients that estimated sensitivity and specificity of 85% and 85% for SPECT and 90% and 88% for PET.
Jaarsma C, Leiner T, Bekkers SC, et al. Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. J Am Coll Cardiol. 2012;59:1719–28. Comprehensive meta-analysis of cardiac magnetic resonance as well as SPECT and PET MPI for coronary artery disease. With #33 & #34, these meta-analyses are likely the last to be performed upon SPECT and PET with anatomic (percent) stenosis as the reference standard.
Candell-Riera J, Oller-Martínez G, Pereztol-Valdés O, et al. Usefulness of myocardial perfusion SPECT in patients with left bundle branch block and previous myocardial infarction. Heart. 2003;89:1039–42.
Iskandrian AE, Verani MS, editors. Nuclear cardiac imaging: principles and applications. 3rd ed. New York: Oxford University Press; 2003. p. 164–89.
Burns RJ, Galligan L, Wright LM, Lawand S, Burke RJ, Gladstone PJ. Improved specificity of myocardial thallium-201 single-photon emission computed tomography in patients with left bundle branch block by dipyridamole. Am J Cardiol. 1991;68:504–8.
Rockett JF, Wood WC, Moinuddin M, et al. Intravenous dipyridamole thallium-201 SPECT imaging in patients with left bundle branch block. Clin Nucl Med. 1990;15:401–7.
O’Keefe JH, Bateman TM, Silvestri R, Barnhart C. Safety and diagnostic accuracy of adenosine thallium-201 scintigraphy in patients unable to exercise and those with left bundle branch block. Am Heart J. 1992;124:614–21.
Koepfli P, Wyss CA, Gaemperli O, et al. Left bundle branch block causes relative but not absolute septal underperfusion during exercise. Eur Heart J. 2009;30:2993–9.
Shaw LJ, Bairey Merz CN, Pepine CJ, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 2006;47:S4–20.
Iskandar A, Limone B, Parker MW, et al. Gender differences in the diagnostic accuracy of SPECT myocardial perfusion imaging: a bivariate meta-analysis. J Nucl Cardiol. 2013;20:53–63.
Danad I, Raijmakers PG, Knaapen P. Diagnosing coronary artery disease with hybrid PET/CT: it takes two to tango. J Nucl Cardiol. 2013;20:874–90. Review of the nascent diagnostic accuracy literature for hybrid PET with computed tomography coronary angiography.
Rispler S, Keidar Z, Ghersin E, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol. 2007;49:1059–67.
Sato A, Nozato T, Hikita H, et al. Incremental value of combining 64-slice computed tomography angiography with stress nuclear myocardial perfusion imaging to improve noninvasive detection of coronary artery disease. J Nucl Cardiol. 2010;17:19–26.
Schaap J, Kauling RM, Boekholdt SM, et al. Incremental diagnostic accuracy of hybrid SPECT/CT coronary angiography in a population with an intermediate to high pre-test likelihood of coronary artery disease. Eur Heart J Cardiovasc Imaging. 2013;14:642–9.
Groves AM, Speechly-Dick M-E, Kayani I, et al. First experience of combined cardiac PET/64-detector CT angiography with invasive angiographic validation. Eur J Nucl Med Mol Imaging. 2009;36:2027–33.
Kajander S, Joutsiniemi E, Saraste M, et al. Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122:603–13.
Danad I, Raijmakers PG, Appelman YE, et al. Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2013;54:55–63.
Bateman TM, Heller GV, McGhie AI, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13:24–33.
Yoshinaga K, Chow BJW, Williams K, et al. What is the prognostic value of myocardial perfusion imaging using rubidium-82 positron emission tomography? J Am Coll Cardiol. 2006;48:1029–39.
Bateman TM. Advantages and disadvantages of PET and SPECT in a busy clinical practice. J Nucl Cardiol. 2012;19 Suppl 1:S3–11.
Diamond GA. The wizard of odds: Bayes theorem and diagnostic testing. Mayo Clin Proc. 1999;74:1179–82.
Compliance with Ethics Guidelines
Conflict of Interest
Matthew Parker has received grants and personal fees from Intersocietal Accreditation Commission and grants from Lantheus Medical Imaging.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiac Nuclear Imaging
Rights and permissions
About this article
Cite this article
Parker, M.W. Comparison of the Diagnostic Accuracy of PET and SPECT for Coronary Artery Disease. Curr Cardiovasc Imaging Rep 8, 9302 (2015). https://doi.org/10.1007/s12410-014-9302-0
Published:
DOI: https://doi.org/10.1007/s12410-014-9302-0