Abstract
Idiopathic pulmonary fibrosis (IPF) is a progressive lung disease associated with significant morbidity and mortality. The diagnosis of IPF involves a combination of clinical history, radiological imaging and examination of histopathological samples in appropriate cases. Historically, transbronchial biopsy (TBB) has been used to obtain histological samples; however this lacks diagnostic accuracy. At present, surgical lung biopsy (SLB) is the gold standard technique for obtaining specimen samples; however this carries a significant mortality risk. Transbronchial lung cryobiopsy (TBLC) is a new technique that has been pioneered in the management of lung malignancy and offers a potential alternative to SLB. The technique employs a freezing probe, which is used to obtain lung tissue samples that are larger and better quality than traditional TBB samples. This affords TBLC an estimated diagnostic yield of 80% in interstitial lung disease. However, with limited evidence directly comparing TBLC to SLB, the diagnostic accuracy of the procedure has been uncertain. Common complications of TBLC include pneumothorax and bleeding. Mortality in TBLC is low compared with SLB, with exacerbation of IPF frequently reported as the cause. TBLC represents an exciting potential option in the diagnostic pathway in IPF; however its true value has yet to be determined.
Similar content being viewed by others
Introduction
Interstitial lung diseases (ILDs) are a heterogeneous group of disorders causing inflammation and scarring of the lung interstitium. Idiopathic pulmonary fibrosis (IPF) is the commonest form of ILD, characterised by progressive fibrosis of the lung parenchyma. It is associated with significant morbidity and mortality, with a reported median survival of 3–5 years post diagnosis [1]. Distinguishing IPF from other forms of ILD is of great importance as there are significant implications for treatment options and prognosis. Two novel antifibrotic agents, pirfenidone and nintedanib, have been shown to slow the progression of IPF and now represent first-line therapeutic options [2, 3]. Conversely, immunosuppressive therapy, formerly the mainstay of treatment and a common treatment option in other forms of ILD, has been associated with increased mortality in IPF [4].
Despite recent progress in the treatment of IPF, significant challenges exist, particularly regarding accuracy of diagnosis. The diagnosis of IPF involves a combination of clinical history, radiological imaging and examination of histopathological samples in appropriate cases. Clinical history is required to exclude known causes of lung fibrosis, such as occupational exposure and connective tissue disease, while imaging and biopsy specimens are examined for evidence of a usual interstitial pneumonia (UIP) pattern of disease. Two international consensus guidelines have recently been published, one by the joint thoracic societies and the other by the Fleischner Society, which update the description of UIP on both high-resolution computer tomography (HRCT) and surgical lung biopsy (SLB) specimen [5, 6]. The guidelines suggest that a diagnosis of IPF can be made on clinical history and HRCT scan alone if a definite pattern of UIP is seen, that is, fibrosis that has a subpleural and basal distribution with visible honeycomb cysts. If honeycomb cysts are not seen but the distribution is typical and other features of fibrosis are present, such as reticulation and traction bronchiectasis/bronchiolectasis, the pattern can only be described as “probable UIP”. Less typical patterns would be described as “indeterminate” or not UIP (“alternative diagnosis”) if features of an alternative ILD are seen. The American Thoracic Society (ATS)/European Respiratory Society (ERS)/Japanese Respiratory Society (JRS)/Latin American Thoracic Society (ALAT) guidelines recommend that histological sampling should be considered in any case where a definite UIP pattern is not seen on HRCT. In a large therapeutic clinical trial, only 53.4% of patients had evidence of honeycombing on HRCT [7]. Importantly, the Fleischner Society offer an alternative opinion regarding the role of biopsy [6]. These guidelines suggest that, in the appropriate clinical context, a diagnosis of IPF can be made if a probable UIP pattern is observed on HRCT, without the need for histological examination.
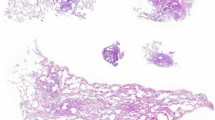
A histological diagnosis of UIP relies upon the identification of alternating areas of preserved lung architecture and advanced fibrosis with minimal inflammation, creating a variegated appearance. These are better appreciated at low magnification and require adequate tissue size and specimen quality. In the past, traditional transbronchial biopsy (TBB) sampling has been used to obtain histological samples in suspected IPF; however it has long been recognised that their value in the diagnostic process is extremely limited [1]. TBB samples are small in size and subject to significant crush artefact, preventing detailed study of tissue architecture [8]. Surgical lung biopsy (SLB) samples are ideal for histological examination as they are generally large, and the lung architecture is well preserved. In clinical practice SLB rates are low and it is common for a “working diagnosis of IPF” to be made solely on radiology and clinical history [9, 10]. This is particularly true in the context of a probable UIP pattern on HRCT, in line with Fleischner Society recommendations [6]. A recent study involving 404 physicians from around the globe found that 63% were prepared to prescribe treatment for patients with a “working diagnosis of IPF” without requesting an SLB [11]. In the UK, it is estimated that only 13% of IPF diagnoses included an SLB [12]. The primary reason for low SLB rates centres around concerns regarding high morbidity and mortality risks compared with standard diagnostic tests. The procedure can be performed either through an open thoracotomy or via video-assisted thoracoscopic surgery (VATS), which is generally the preferred option due to reduced length of stay [13, 14]. Mortality rates post-procedure have been variably reported with two recent studies noting 30-day mortality at 2.4% and 7.1% [15, 16]. Mortality is higher in patients undergoing a non-elective SLB but is also higher in older, co-morbid patients. Death following an exacerbation of ILD is the most commonly reported cause of mortality in patients undergoing a diagnostic SLB [17,18,19].
There is a drive within the ILD community to develop safer diagnostic techniques with sufficient yield that they would provide a feasible alternative to SLB. Transbronchial lung cryobiopsy (TBLC) is seen by many as the most promising option. Cryosurgical techniques have been used in the airways since 1968, traditionally in palliative treatment of obstructive endobronchial tumours and the management of acute airway obstruction [20, 21]. Their role in lung biopsies has been relatively recent and has predominantly involved malignant sample retrieval [22]. TBLC represents an attractive diagnostic tool in ILD as it may allow large tissue samples to be extracted and improve histological architecture preservation compared with TBB [8]. In this review article we will discuss the technical aspects of this procedure, the evidence for its use as a method of obtaining biopsy tissue in IPF and potential risks associated with the procedure. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Transbronchial Lung Cryobiopsy: Technical Aspects
Flexible cryoprobes employ the Joule-Thomson effect of thermodynamics by which a gas, nitrous oxide in this context, is rapidly decompressed through a small nozzle leading to extreme drops in temperature. This freezing process leads to tissue adhering to the probe, which can subsequently be removed. There are no standardised methods for performing TBLC in ILD and a wide variety of techniques have been employed in the published data. A recent statement from an international expert panel has sought to provide some clarity regarding the optimum sampling technique [23]. Although TBLC has been performed under local anaesthetic, expert consensus is that the procedure should be performed under general anaesthetic, using either a flexible or rigid bronchoscope. A bronchial blocker or Fogarty balloon may be employed to manage potential haemorrhage [24, 25]. The bronchoscope is positioned within the relevant area of interest, often guided by pre-procedure high-resolution CT thorax. The cryoprobe is advanced to its limit and then withdrawn 1–2 cm to a final position equating to approximately 1 cm from the pleura [24,25,26,27,28,29]. Some studies include the use of fluoroscopy to confirm the final position of the cryoprobe and one small prospective study reported safe use of a radial miniprobe to guide TBLC in ILD [30]. The cryoprobe is then cooled for 5–7 s and then withdrawn from the bronchoscope [24,25,26,27, 29]. The temperature reached by the probe varies from − 45 to − 89.5 °C [31]. The tip of the probe is placed in a saline bath and once the sample has thawed and fallen away from the scope it can be transferred to formalin for processing.
There is no consistent number of samples within the range of studies that have been conducted but typically between two and five samples were taken [27, 29]. In a prospective study of 46 patients, it was found that diagnostic yield increased with a second biopsy if the sample arises from two different segments within the same lobe (69% vs. 96%) [32]. The cryoprobes are available in different lengths, generally 900 mm or 1150 mm, with a diameter of 1.9 mm or 2.4 mm. There has been a suggestion that activation time, the point from which contact is made between probe and tissue, and probe size could affect the amount of tissue obtained via biopsy; however the smallest cryoprobe was still noted to provide a larger biopsy than a forceps biopsy [33]. The size of the sample obtained is important, as diagnostic yield appears to correlate with specimen size [24]. It has been suggested that specimen samples should be ≥ 5 mm to be considered adequate for histological examination [26].
Transbronchial Lung Cryobiopsy: Evidence for Use in IPF
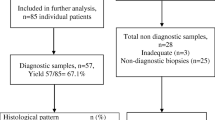
Table 1 summarises the published studies of TBLC in suspected ILD including IPF patients. The majority of the evidence for diagnostic yield in ILD comes from retrospective cohort studies and case series. In the first study reporting the use of TBLC in ILD, 39 of the 41 patients undergoing the procedure received a definitive diagnosis at a multi-disciplinary team (MDT) meeting while the other two patients required a further SLB to confirm diagnosis [22]. Subsequent single-centre studies have reported variable diagnostic yields, ranging between 44.2 and 87.8 for histological diagnosis and 68.3–98% for an MDT diagnosis [27, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. A small prospective study reported that 87.5% of patients undergoing TBLC obtained an MDT diagnosis with high confidence [51]. Several meta-analyses have been published that consistently report a diagnostic yield for TBLC of approximately 80%, however with significant heterogeneity between the included studies [5, 45, 52, 53]. Most recently, a large multi-centre cohort study of 699 patients, including some previously published data, reported a diagnostic yield of 87.8%, which helped achieve a multidisciplinary diagnosis in 90.1% of cases [54]. IPF was the most common diagnosis in this cohort. In cases of UIP, interobserver agreement amongst three pathologists was moderate at 0.54. Similar levels of agreement have been noted in SLB specimen interpretation [55], reflecting the difficulty in making a diagnosis even with optimum pathological sampling. It has been suggested that TBLC significantly increases the confidence of making a diagnosis of IPF at the MDT level [49]. In a cross-sectional study assessing the impact of TBLC on the MDT diagnostic process in fibrotic ILD, the addition of TBLC improved the confidence of IPF diagnosis from 29% to 63% and was comparable to SLB. In 19% of cases the diagnosis was changed to IPF following the addition of TBLC samples. In another study [27], 20 patients with a radiological pattern of possible UIP as per previous international consensus guidelines [1] underwent TBLC. At MDT, nine subsequently received a diagnosis of IPF, three of hypersensitivity pneumonitis, two of non-specific interstitial pneumonia, five with alternative diagnoses and one did not receive a diagnosis.
As expected, TBLC compares favourably to TBB in diagnostic utility in ILD. A randomised control trial comparing TBLC to TBB in 77 patients under an ILD diagnostic pathway found that the diagnostic yield was significantly higher in those patients who had TBLC (74.4% vs. 34.1%) [56]. A retrospective analysis of a cohort of 56 patients who underwent both TBB and TBLC for suspected ILD in a single centre reported that TBLC was diagnostic in 11 cases where TBB was non-diagnostic [57]. Interestingly, TBB was diagnostic in four cases in which TBLC was not and in 15 cases neither were diagnostic. A meta-analysis of eight studies, which included a total 916 patients, concluded that TBLC allowed for larger specimen sizes, fewer artefacts and superior diagnostic yield compared with TBB [58]. Despite a significant improvement in diagnostic yield in comparison to TBB, TLBC appears to fall short of SLB, which is still considered the gold standard method of obtaining adequate lung tissue for diagnosis in IPF and other forms of ILD. A retrospective analysis of 150 patients undergoing SLB and 297 having TBLC found that the diagnostic yield of SLB was 98.7% compared with 82.8% with TBLC [45]. Meta-analyses have estimated a diagnostic yield of 83.7–84.4% in TBLC and 91.1–92.7% in SLB [59, 60]. While the diagnostic yield of TBLC has been well reported, the diagnostic accuracy of TBLC in ILD is not as clear, as few patients will undergo both TBLC and SLB. Early data are emerging from prospective studies in patients receiving both procedures. A small two-centre study has recently been published in which 21 patients had TBLC and SLB from the same anatomical locations [61]. In only 38% of cases was the histological diagnosis concordant between the two biopsy methods. SLB was concordant with the final MDT diagnosis in 62% cases compared with 48% with TBLC. Another prospective study comparing TBLC, TBB and SLB in 20 patients is ongoing (NCT01972685).
Transbronchial Lung Cryobiopsy: Safety in IPF
A significant concern regarding the use of TBLC in the diagnosis of IPF is safety. Reported complication rates vary considerably, possibly because of the heterogeneity of the sampling methods used and experience of the operator. The two most commonly reported complications are pneumothorax and bleeding. The reported rates of these complications are summarised in Table 1.
The rates of pneumothorax post-TBLC have been variably reported between 0% and 33% [22, 24, 27, 29, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51, 56, 61,62,63,64]. One meta-analysis reported an overall pneumothorax risk of 6% with a 3% risk of chest drain insertion [45]. More recent meta-analyses estimate the overall procedural pneumothorax risk to be closer to 10% [5, 59, 60]. Comparatively, these studies estimated pneumothorax risk post-TBB to be similar at 6–10%, while persistent air-leak post-SLB was 2–6%. A large multicentre retrospective study reported an overall pneumothorax rate of 19.2% in a cohort of 699 patients with suspected ILD undergoing TBLC of which 70% required drainage [54]. The impact this had on length of stay was not reported. Pneumothorax risk was significantly higher when the larger 2.4 mm probe was used as opposed to the 1.9 mm probe (21.2% vs. 2.7%). In addition, pneumothorax was also more common when multiple lobes were sampled and when three or more biopsies were taken. Pneumothorax was more common when biopsies were taken from the lower lobes. The risk of developing a pneumothorax is increased if pleural fragments are identified in the biopsy and declines if fluoroscopic guidance is used [24, 65]. Patients with IPF are more at risk of pneumothorax than other forms of ILD [23, 54]. In addition, patients who suffer from pneumothorax tend to have poorer baseline lung function, although an FVC of < 50% predicted does not appear to be a risk factor for developing a pneumothorax as a complication of TBLC [54].
Bleeding is common post TBLC; however overall bleeding risk is difficult to quantify as there is no internationally accepted severity scale, although a classification of mild, moderate and severe bleeding described by Ernst et al. is most commonly used [66]. Mild bleeding, not requiring intervention, has been reported in 30% of cases [56]. Pooled analyses of studies reporting moderate and severe bleeding estimate a risk of 4.9–39% [53, 59, 60]. Risk of bleeding appears to be higher when the lower lobes are sampled, likely reflecting the basal predominance of UIP pattern fibrosis, but does not appear to be related to the number of sites sampled or the size of the probe [54]. Due to the risk of severe bleeding, it is recommended that a pre-emptive endobronchial blocker or occlusive balloon be placed in the airway [23]. The use of an occlusion balloon has been associated with a significantly lower incidence of moderate-to-severe bleeding (1.8% vs. 35.7%) [65]. To accommodate both a bronchoscope and a blocker/balloon simultaneously, a rigid bronchoscope or flexible endotracheal tube is required and would require general anaesthetic support. However, techniques using a deflated endobronchial blocker alongside a flexible bronchoscope have been described, obviating the requirement for rigid bronchoscopy or general anaesthesia [67].
The major concern that troubles both patients and physicians with regard to SLB in the diagnosis of IPF is the risk of mortality. Thirty-day mortality post-SLB has recently been reported to be as high as 7.1% [16]. Exacerbation of IPF following SLB is felt to be a leading cause of mortality [19]. In comparison, pooled-analyses estimated mortality rates post-TBLC to be 0.1–2.7% [5, 52, 59, 60]. Exacerbation of IPF remains a leading cause of death in these patients [24, 54, 65, 68]. The overall frequency of exacerbation post-TBLC is unclear as it is not commonly reported in the published data. This may reflect the lack of a universally recognised definition of an acute exacerbation. Length of stay has been estimated at 3 days for patients with IPF undergoing TBLC compared with 6 days for those undergoing SLB [49].
Conclusion
The use of TBLC in the diagnosis of IPF continues to divide opinion in the ILD community. This is apparent from the publication of the 2018 guidelines for diagnosis of IPF when the guideline panel did not make a recommendation regarding its use in the context of probable or indeterminate UIP on CT [5]. The panel were evenly split for and against the use. On one hand, TBLC appears to offer the opportunity to obtain large-volume, well-preserved lung tissue allowing reasonable diagnostic yield with less mortality risk than SLB. However, on the other hand, morbidity post-TBLC is not insignificant and concerns regarding diagnostic accuracy have been raised [61]. Of concern is the fact that some complications, such as pneumothorax, are more common in patients with IPF [54]. The safety data published thus far for TBLC in suspected ILD may not be fully reflective of patients diagnosed with IPF. As shown in Table 1, the proportion of patients in the published work with an eventual diagnosis of IPF is commonly < 30%. In addition, the average age of patients included in a recent large retrospective analysis was 61 with a forced vital capacity of 85.4% predicted and transfer factor of 61.2% [54]. Registry data suggest the average age of IPF patients is closer to 70 with significantly poorer lung function [69]. The risk of TBLC in this group needs further examination to determine whether the technique is significantly safer than SLB. While these concerns need to be addressed, there are other areas such as cost in which TBLC appears to carry significant benefit over SLB [60, 70, 71]. In addition, as expertise and experience grow, the accuracy and safety of the technique will also improve.
While the body of evidence regarding the use of TBLC in IPF grows, the quality remains low. The majority of publications are retrospective single-centre studies, which suffer from significant risk of bias. The reported diagnostic yield varies considerably within the study set. This reflects intrinsic differences in patient selection based on clinical characteristics, such as age and co-morbidities, and disease features, such as radiological extent of disease. There has been a dearth of protocolised prospective work in the field to date; however, change is on the horizon. In addition to the recently published prospective comparison study between TBLC and SLB [61], there are a further 11 studies registered to clinicaltrials.gov assessing the utility of TBLC in ILD. However, at present it remains unclear as to the eventual role of TBLC in the diagnosis of IPF and there remains a definite need to identify novel tests that have high diagnostic accuracy and are minimally invasive.
References
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. https://doi.org/10.1164/rccm.2009-040gl.
King TE Jr, Bradford WZ, Castro-Bernardini S, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–92. https://doi.org/10.1056/nejmoa1402582.
Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82. https://doi.org/10.1056/nejmoa1402584.
Network TIPFCR. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366:1968–77. https://doi.org/10.1056/nejmoa1113354.
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of Idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–68. https://doi.org/10.1164/rccm.201807-1255st.
Lynch DA, Sverzellati N, Travis WD, et al. Diagnostic criteria for idiopathic pulmonary fibrosis: a Fleischner Society White Paper. Lancet Respir Med. 2018;6:138–53. https://doi.org/10.1016/s2213-2600(17)30433-2.
Raghu G, Wells AU, Nicholson AG, et al. Effect of nintedanib in subgroups of idiopathic pulmonary fibrosis by diagnostic criteria. Am J Respir Crit Care Med. 2017;195:78–85. https://doi.org/10.1164/rccm.201602-0402oc.
Griff S, Ammenwerth W, Schonfeld N, et al. Morphometrical analysis of transbronchial cryobiopsies. Diagn Pathol. 2011;6:53. https://doi.org/10.1186/1746-1596-6-53.
Cottin V. Lung biopsy in interstitial lung disease: balancing the risk of surgery and diagnostic uncertainty. Eur Respir J. 2016;48:1274–7. https://doi.org/10.1183/13993003.01633-2016.
Wells AU. Any fool can make a rule and any fool will mind it. BMC Med. 2016;14:23. https://doi.org/10.1186/s12916-016-0562-1.
Walsh SLF, Lederer DJ, Ryerson CJ, et al. Diagnostic likelihood thresholds that define a working diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2019. https://doi.org/10.1164/rccm.201903-0493oc.
The British Thoracic Society Interstitial Lung Disease Registry Programme Annual Report 2015/2016. 2016.
Bensard DD, McIntyre RC Jr, Waring BJ, et al. Comparison of video thoracoscopic lung biopsy to open lung biopsy in the diagnosis of interstitial lung disease. Chest. 1993;103:765–70.
Carnochan FM, Walker WS, Cameron EW. Efficacy of video assisted thoracoscopic lung biopsy: an historical comparison with open lung biopsy. Thorax. 1994;49:361–3.
Hutchinson JP, McKeever TM, Fogarty AW, et al. Surgical lung biopsy for the diagnosis of interstitial lung disease in England: 1997–2008. Eur Respir J. 2016;48:1453–61. https://doi.org/10.1183/13993003.00378-2016.
Fisher JH, Shapera S, To T, et al. Procedure volume and mortality after surgical lung biopsy in interstitial lung disease. Eur Respir J. 2018. https://doi.org/10.1183/13993003.01164-2018.
Fibla JJ, Brunelli A, Cassivi SD, et al. Aggregate risk score for predicting mortality after surgical biopsy for interstitial lung disease. Interact Cardiovasc Thorac Surg. 2012;15:276–9. https://doi.org/10.1093/icvts/ivs174.
Bando M, Ohno S, Hosono T, et al. Risk of acute exacerbation after video-assisted thoracoscopic lung biopsy for interstitial lung disease. J Bronchol Interv Pulmonol. 2009;16:229–35. https://doi.org/10.1097/lbr.0b013e3181b767cc.
Kreider ME, Hansen-Flaschen J, Ahmad NN, et al. Complications of video-assisted thoracoscopic lung biopsy in patients with interstitial lung disease. Ann Thorac Surg. 2007;83:1140–4. https://doi.org/10.1016/j.athoracsur.2006.10.002.
Hetzel M, Hetzel J, Schumann C, et al. Cryorecanalization: a new approach for the immediate management of acute airway obstruction. J Thorac Cardiovasc Surg. 2004;127:1427–31. https://doi.org/10.1016/j.jtcvs.2003.12.032.
Sheski FD, Mathur PN. Endoscopic treatment of early-stage lung cancer. Cancer Control. 2000;7:35–44. https://doi.org/10.1177/107327480000700103.
Babiak A, Hetzel J, Krishna G, et al. Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration. 2009;78:203–8. https://doi.org/10.1159/000203987.
Hetzel J, Maldonado F, Ravaglia C, et al. Transbronchial cryobiopsies for the diagnosis of diffuse parenchymal lung diseases: expert statement from the Cryobiopsy Working Group on safety and utility and a call for standardization of the procedure. Respiration. 2018;95:188–200. https://doi.org/10.1159/000484055.
Casoni GL, Tomassetti S, Cavazza A, et al. Transbronchial lung cryobiopsy in the diagnosis of fibrotic interstitial lung diseases. PLoS One. 2014;9:e86716. https://doi.org/10.1371/journal.pone.0086716.
Bondue B, Pieters T, Alexander P, et al. Role of transbronchial lung cryobiopsies in diffuse parenchymal lung diseases: interest of a sequential approach. Pulm Med. 2017;2017:6794343. https://doi.org/10.1155/2017/6794343.
Colby TV, Tomassetti S, Cavazza A, et al. Transbronchial cryobiopsy in diffuse lung disease: update for the pathologist. Arch Pathol Lab Med. 2017;141:891–900. https://doi.org/10.5858/arpa.2016-0233-ra.
Kronborg-White S, Folkersen B, Rasmussen TR, et al. Introduction of cryobiopsies in the diagnostics of interstitial lung diseases—experiences in a referral center. Eur Clin Respir J. 2017;4:1274099–1274099. https://doi.org/10.1080/20018525.2016.1274099.
Hetzel J, Eberhardt R, Herth FJ, et al. Cryobiopsy increases the diagnostic yield of endobronchial biopsy: a multicentre trial. Eur Respir J. 2012;39:685–90. https://doi.org/10.1183/09031936.00033011.
Bango-Álvarez A, Ariza-Prota M, Torres-Rivas H, et al. Transbronchial cryobiopsy in interstitial lung disease: experience in 106 cases—how to do it. ERJ Open Res. 2017;3:00148–2016. https://doi.org/10.1183/23120541.00148-2016.
Gnass M, Filarecka A, Pankowski J, et al. Transbronchial lung cryobiopsy guided by endobronchial ultrasound radial miniprobe in interstitial lung diseases: preliminary results of a prospective study. Pol Arch Intern Med. 2018;128:259–62. https://doi.org/10.20452/pamw.4253.
Schumann C, Hetzel J, Babiak AJ, et al. Cryoprobe biopsy increases the diagnostic yield in endobronchial tumor lesions. J Thorac Cardiovasc Surg. 2010;140:417–21. https://doi.org/10.1016/j.jtcvs.2009.12.028.
Ravaglia C, Wells AU, Tomassetti S, et al. Transbronchial lung cryobiopsy in diffuse parenchymal lung disease: comparison between biopsy from 1 segment and biopsy from 2 segments—diagnostic yield and complications. Respiration. 2017;93:285–92. https://doi.org/10.1159/000456671.
Franke KJ, Szyrach M, Nilius G, et al. Experimental study on biopsy sampling using new flexible cryoprobes: influence of activation time, probe size, tissue consistency, and contact pressure of the probe on the size of the biopsy specimen. Lung. 2009;187:253–9. https://doi.org/10.1007/s00408-009-9156-4.
Lentz RJ, Taylor TM, Kropski JA, et al. Utility of flexible bronchoscopic cryobiopsy for diagnosis of diffuse parenchymal lung diseases. J Bronchol Interv Pulmonol. 2018;25:88–96. https://doi.org/10.1097/lbr.0000000000000401.
Ussavarungsi K, Kern RM, Roden AC, et al. Transbronchial cryobiopsy in diffuse parenchymal lung disease: retrospective analysis of 74 cases. Chest. 2017;151:400–8. https://doi.org/10.1016/j.chest.2016.09.002.
DiBardino DM, Haas AR, Lanfranco AR, et al. High complication rate after introduction of transbronchial cryobiopsy into clinical practice at an Academic Medical Center. Ann Am Thorac Soc. 2017;14:851–7. https://doi.org/10.1513/AnnalsATS.201610-829OC.
Cooley J, Balestra R, Aragaki-Nakahodo AA, et al. Safety of performing transbronchial lung cryobiopsy on hospitalized patients with interstitial lung disease. Respir Med. 2018;140:71–6. https://doi.org/10.1016/j.rmed.2018.05.019.
Fruchter O, Fridel L, El Raouf BA, et al. Histological diagnosis of interstitial lung diseases by cryo-transbronchial biopsy. Respirology. 2014;19:683–8. https://doi.org/10.1111/resp.12296.
Marçôa R, Linhas R, Apolinário D, et al. Diagnostic yield of transbronchial lung cryobiopsy in interstitial lung diseases. Pulmonology. 2017;23:296–8. https://doi.org/10.1016/j.rppnen.2017.07.002.
Kuse N, Inomata M, Awano N, et al. Management and utility of transbronchial lung cryobiopsy in Japan. Respir Investig. 2019;57:245–51. https://doi.org/10.1016/j.resinv.2018.12.011.
Griff S, Schonfeld N, Ammenwerth W, et al. Diagnostic yield of transbronchial cryobiopsy in non-neoplastic lung disease: a retrospective case series. BMC Pulm Med. 2014;14:171. https://doi.org/10.1186/1471-2466-14-171.
Hernandez-Gonzalez F, Lucena CM, Ramirez J, et al. Cryobiopsy in the diagnosis of diffuse interstitial lung disease: yield and cost-effectiveness analysis. Arch Bronconeumol. 2015;51:261–7. https://doi.org/10.1016/j.arbres.2014.09.009.
Samitas K, Kolilekas L, Vamvakaris I, et al. Introducing transbronchial cryobiopsies in diagnosing diffuse parenchymal lung diseases in Greece: implementing training into clinical practice. PLoS One. 2019;14:e0217554. https://doi.org/10.1371/journal.pone.0217554.
Almeida LM, Lima B, Mota PC, et al. Learning curve for transbronchial lung cryobiopsy in diffuse lung disease. Rev Port Pneumol 2006. 2017. https://doi.org/10.1016/j.rppnen.2017.09.005.
Ravaglia C, Bonifazi M, Wells AU, et al. Safety and diagnostic yield of transbronchial lung cryobiopsy in diffuse parenchymal lung diseases: a comparative study versus video-assisted thoracoscopic lung biopsy and a systematic review of the literature. Respiration. 2016;91:215–27. https://doi.org/10.1159/000444089.
Cho R, Zamora F, Gibson H, et al. Transbronchial lung cryobiopsy in the diagnosis of interstitial lung disease: a retrospective single-center experience. J Bronchol Interv Pulmonol. 2019;26:15–21. https://doi.org/10.1097/LBR.0000000000000514.
Sriprasart T, Aragaki A, Baughman R, et al. A single US Center experience of transbronchial lung cryobiopsy for diagnosing interstitial lung disease with a 2-scope technique. J Bronchol Interv Pulmonol. 2017;24:131–5. https://doi.org/10.1097/lbr.0000000000000366.
Kropski JA, Pritchett JM, Mason WR, et al. Bronchoscopic cryobiopsy for the diagnosis of diffuse parenchymal lung disease. PLoS One. 2013;8:e78674. https://doi.org/10.1371/journal.pone.0078674.
Tomassetti S, Wells AU, Costabel U, et al. Bronchoscopic lung cryobiopsy increases diagnostic confidence in the multidisciplinary diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2016;193:745–52. https://doi.org/10.1164/rccm.201504-0711OC.
Echevarria-Uraga JJ, Perez-Izquierdo J, Garcia-Garai N, et al. Usefulness of an angioplasty balloon as selective bronchial blockade device after transbronchial cryobiopsy. Respirology. 2016;21:1094–9. https://doi.org/10.1111/resp.12827.
Cascante JA, Cebollero P, Herrero S, et al. Transbronchial cryobiopsy in interstitial lung disease: are we on the right path? J Bronchol Interv Pulmonol. 2016;23:204–9. https://doi.org/10.1097/LBR.0000000000000292.
Dhooria S, Sehgal IS, Aggarwal AN, et al. Diagnostic yield and safety of cryoprobe transbronchial lung biopsy in diffuse parenchymal lung diseases: systematic review and meta-analysis. Respir Care. 2016;61:700–12. https://doi.org/10.4187/respcare.04488.
Johannson KA, Marcoux VS, Ronksley PE, et al. Diagnostic yield and complications of transbronchial lung cryobiopsy for interstitial lung disease. A systematic review and metaanalysis. Ann Am Thorac Soc. 2016;13:1828–38. https://doi.org/10.1513/AnnalsATS.201606-461SR.
Ravaglia C, Wells AU, Tomassetti S, et al. Diagnostic yield and risk/benefit analysis of trans-bronchial lung cryobiopsy in diffuse parenchymal lung diseases: a large cohort of 699 patients. BMC Pulm Med. 2019;19:16. https://doi.org/10.1186/s12890-019-0780-3.
Nicholson AG. Inter-observer variation between pathologists in diffuse parenchymal lung disease. Thorax. 2004;59:500–5. https://doi.org/10.1136/thx.2003.011734.
Pajares V, Puzo C, Castillo D, et al. Diagnostic yield of transbronchial cryobiopsy in interstitial lung disease: a randomized trial. Respirology. 2014;19:900–6. https://doi.org/10.1111/resp.12322.
Ramaswamy A, Homer R, Killam J, et al. Comparison of transbronchial and cryobiopsies in evaluation of diffuse parenchymal lung disease. J Bronchol Interv Pulmonol. 2016;23:14–21. https://doi.org/10.1097/lbr.0000000000000246.
Ganganah O, Guo SL, Chiniah M, et al. Efficacy and safety of cryobiopsy versus forceps biopsy for interstitial lung diseases and lung tumours: a systematic review and meta-analysis. Respirology. 2016;21:834–41. https://doi.org/10.1111/resp.12770.
Iftikhar IH, Alghothani L, Sardi A, et al. Transbronchial lung cryobiopsy and video-assisted thoracoscopic lung biopsy in the diagnosis of diffuse parenchymal lung disease. A meta-analysis of diagnostic test accuracy. Ann Am Thorac Soc. 2017;14:1197–211. https://doi.org/10.1513/AnnalsATS.201701-086SR.
Sharp C, Adamali H, Medford AR, et al. Use of transbronchial cryobiopsy in the diagnosis of interstitial lung disease—a systematic review and cost analysis. QJM. 2016;110:207–14. https://doi.org/10.1093/qjmed/hcw142.
Romagnoli M, Colby TV, Berthet JP, et al. Poor concordance between sequential transbronchial lung cryobiopsy and surgical lung biopsy in the diagnosis of diffuse interstitial lung diseases. Am J Respir Crit Care Med. 2019;1:1. https://doi.org/10.1164/rccm.201810-1947OC.
Wälscher J, Eberhardt R, Heußel CP, et al. Real world experience with transbronchial cryobiopsies for diagnosing interstitial lung disease (ILD). Eur Respir J. 2017;50:OA4636. https://doi.org/10.1183/1393003.congress-2017.OA4636.
Hagmeyer L, Theegarten D, Treml M, et al. Validation of transbronchial cryobiopsy in interstitial lung disease—interim analysis of a prospective trial and critical review of the literature. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33:2–9.
Hagmeyer L, Theegarten D, Wohlschlager J, et al. The role of transbronchial cryobiopsy and surgical lung biopsy in the diagnostic algorithm of interstitial lung disease. Clin Respir J. 2016;10:589–95. https://doi.org/10.1111/crj.12261.
Dhooria S, Mehta RM. The safety and efficacy of different methods for obtaining transbronchial lung cryobiopsy in diffuse lung diseases. Clin Respir J. 2018;12:1711–20. https://doi.org/10.1111/crj.12734.
Ernst A, Eberhardt R, Wahidi M, et al. Effect of routine clopidogrel use on bleeding complications after transbronchial biopsy in humans. Chest. 2006;129:734–7. https://doi.org/10.1378/chest.129.3.734.
Hohberger LA, DePew ZS, Utz JP, et al. Utilizing an endobronchial blocker and a flexible bronchoscope for transbronchial cryobiopsies in diffuse parenchymal lung disease. Respiration. 2014;88:521–2. https://doi.org/10.1159/000368616.
Sanna S, Tomassetti S, Argnani D, et al. Multidisciplinary approach in the diagnosis of idiopathic pulmonary fibrosis: role of transbronchial lung cryobiopsy and surgical biopsy on a cohort of 153 patients. Eur Respir J. 2018;52:PA1740. https://doi.org/10.1183/13993003.congress-2018.PA1740.
Behr J, Kreuter M, Hoeper MM, et al. Management of patients with idiopathic pulmonary fibrosis in clinical practice: the INSIGHTS-IPF registry. Eur Respir J. 2015;46:186–96. https://doi.org/10.1183/09031936.00217614.
Nguyen W, Meyer KC. Surgical lung biopsy for the diagnosis of interstitial lung disease: a review of the literature and recommendations for optimizing safety and efficacy. Sarcoidosis Vasc Diffuse Lung Dis. 2013;30:3–16.
Montero Fernandez MA. Transbronchial cryobiopsy in interstitial lung disease: advantageous costs to benefits ratio. Arch Bronconeumol. 2015;51:257–8. https://doi.org/10.1016/j.arbres.2015.02.006.
Hagmeyer L, Theegarten D, Wohlschlager J, et al. Transbronchial cryobiopsy in fibrosing interstitial lung disease: modifications of the procedure lead to risk reduction. Thorax. 2019;74:711–4. https://doi.org/10.1136/thoraxjnl-2018-212095.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Taha Lodhi, Gareth Hughes, Stefan Stanel and Conal Hayton prepared the manuscript. Nazia Chaudhuri contributed to drafting the manuscript.
Disclosures
Conal Hayton has received a research grant from Boehringer Ingelheim. Nazia Chaudhuri has received a research grant from Boehringer Ingelheim and personal fees from Boehringer Ingelheim and Roche to participate in advisory boards and support to attend educational meetings from Roche and Intermune. Taha Lodhi, Gareth Hughes and Stefan Stanel have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8943491.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lodhi, T., Hughes, G., Stanel, S. et al. Transbronchial Lung Cryobiopsy in Idiopathic Pulmonary Fibrosis: A State of the Art Review. Adv Ther 36, 2193–2204 (2019). https://doi.org/10.1007/s12325-019-01036-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01036-y