Abstract
Spinocerebellar ataxias (SCAs) represent a large group of heredodegenerative diseases, with great phenotypic and genotypic heterogeneity. However, in the clinical neurological practice, some symptoms and signs might help differentiate the SCAs. This study’s aims were to evaluate the frequency of upward gaze palsy (UGP) and investigate its role in assisting in the clinical differentiation of SCAs. We included 419 patients with SCAs (248 with SCA3, 95 with SCA10, 38 with SCA2, 22 with SCA1, 12 with SCA7, and 4 with SCA6). This study compared UGP with other known markers of disease severity—age of onset, disease duration, SARA score, and size of CAG expansion, and also other semiologic features, as bulging eyes. This sign was significantly more prevalent in SCA3 (64.11%), compared with SCA10 (3.16%; p < 0.001) and other SCAs (SCA1, SCA2, SCA7–11.84%; p < 0.001). UGP showed very high sensibility ins SCA3 (92.9), although lacking of specificity (64.1%). The odds ratio (OR) of UGP were also very high, 23.52 (95% CI 12.38–44.69), and was significantly correlated with larger CAG expansions, age, and disease duration in SCA3 patients, but not with age of onset or severity of the ataxic syndrome. This study showed that UGP is highly suggestive of SCA3 and has high sensitivity for the differential diagnosis among SCAs, and it could be of great value for bedside semiologic tool.

Similar content being viewed by others
References
Marcoglis RL. Dominant spinocerebellar ataxias: a molecular approach to classification, diagnosis, pathogenesis and the future. Expert Rev Mol Diagn. 2003;3(6):715–32. https://doi.org/10.1586/14737159.3.6.715.
Durr A. Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol. 2010;9(9):885–94. https://doi.org/10.1016/S1474-4422(10)70183-6.
Teive HAG, Ashizawa T. Primary and secondary ataxias. Curr Opin Neurol. 2015;28(4):413–22. https://doi.org/10.1097/WCO.0000000000000227.
Rossi M, Perez-Lloret S, Doldan L, Cerquetti D, Balej J, Millar Vernetti P, et al. Autosomal dominant cerebellar ataxias: a systematic review of clinical features. Eur J Neurol. 2014;21(4):607–15. https://doi.org/10.1111/ene.12350.
Moscovich M, Okun MS, Favilla C, Figueroa KP, Pulst SM, Perlman S, et al. Clinical evaluation of eye movements in spinocerebellar ataxias. J Neuro-Ophthalmol. 2015;35(1):16–21. https://doi.org/10.1097/WNO.0000000000000167.
Coutinho P Doença de Machado-Joseph: Tentativa de Definição. Tese de Doutoramento 1992. https://repositorio-aberto.up.pt/bitstream/10216/10229/7/644_TD_01_P.pdf. Accessed 15 Jun 2020
Schmitz-Hü T, Du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia development of a new clinical scale. Neurology. 2006;66(11):1717–20. https://doi.org/10.1212/01.wnl.0000219042.60538.92.
Braga-Neto P, Godeiro-Junior C, Dutra LA, Pedroso JL, Barsottini OGP. Translation and validation into Brazilian version of the Scale of the Assessment and Rating of Ataxia (SARA). Arq Neuropsiquiatr. 2010;68(2):228–30. https://doi.org/10.1590/S0004-282X2010000200014.
Nascimento FA, Garcia BCM, Teive HAG. Teaching video Neuroimages: Upward gaze palsy is a sign of spinocerebellar ataxia type 3. Neurology. 2018;91(5):e-494. https://doi.org/10.1212/WNL.0000000000005913.
Jacobi H, Hauser TK, Giunti P, Globas C, Bauer P, Schmitz-Hübsch T, et al. Spinocerebellar ataxia types 1, 2, 3 and 6: the clinical spectrum of ataxia and morphometric brainstem and cerebellar findings. Cerebellum. 2012;11(1):155–66. https://doi.org/10.1007/s12311-011-0292-z.
Jardim LB, Hauser L, Kieling C, Saute JAM, Xavier R, Rieder CRM, et al. Progression rate of neurological deficits in a 10-year cohort of SCA3 patients. Cerebellum. 2010;9(3):419–28. https://doi.org/10.1007/s12311-010-0179-4.
Schmitz-Hübsch T, Coudert M, Bauer P, Giunti P, Globas C, Baliko L, et al. Spinocerebellar ataxia types 1, 2, 3, and 6: disease severity and nonataxia symptoms. Neurology. 2008;71(13):982–9. https://doi.org/10.1212/01.wnl.0000325057.33666.72.
Jacobi H, Bauer P, Giunti P, Labrum R, Sweeney MG, Charles P, et al. The natural history of spinocerebellar ataxia type 1, 2, 3, and 6: a 2-year follow-up study. Neurology. 2011;77(11):1035–41. https://doi.org/10.1212/WNL.0b013e31822e7ca0.
Paulson H. Machado-Joseph disease/spinocerebellar ataxia type 3. Handb Clin Neurol. 2012;103:437–49. https://doi.org/10.1016/B978-0-444-51892-7.00027-9.
Jardim LB, Pereira ML, Silveira I, Ferro A, Sequeiros J, Giugliani R. Neurologic findings in Machado-Joseph disease. Arch Neurol. 2001;58(6):899–904. https://doi.org/10.1001/archneur.58.6.899.
Teive H, Munhoz R, Arruda W, Lopes-Cendes I, Raskin S, Werneck L, et al. Spinocerebellar ataxias – genotype-phenotype correlations in 104 Brazilian families. Clinics. 2012;67(5):443–9.
Nascimento FA, Rodrigues VOR, Pelloso FC, Camargo CHF, Moro A, Raskin S, et al. Spinocerebellar ataxias in Southern Brazil: genotypic and phenotypic evaluation of 213 families. Clin Neurol Neurosurg. 2019;184:105427. https://doi.org/10.1016/j.clineuro.2019.105427.
Domingues BMD, Nascimento FA, Meira AT, Moro A, Raskin S, Ashizawa T, et al. Clinical and genetic evaluation of spinocerebellar ataxia type 10 in 16 Brazilian families. Cerebellum. 2019;18(5):849–54. https://doi.org/10.1007/s12311-019-01064-y.
Moro A, Munhoz RP, Arruda WO, Raskin S, Teive HAG. Clinical relevance of "bulging eyes" for the differential diagnosis of spinocerebellar ataxias. Arq Neuropsiquiatr. 2013;71(7):428–30. https://doi.org/10.1590/0004-282X20130056.
Wu C, Chen DB, Feng L, et al. Oculomotor deficits in spinocerebellar ataxia type 3: potential biomarkers of preclinical detection and disease progression. CNS Neurosci Ther. 2017;23(4):321–8. https://doi.org/10.1111/cns.12676.
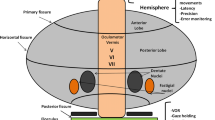
Lloyd-Smith SA, Rizzo JR, Rucker JC. Clinical approach to supranuclear brainstem saccadic gaze palsies. Front Neurol. 2017;8:429. https://doi.org/10.3389/fneur.2017.00429.
Geiner S, Horn AKE, Wadia NH, Sakai H, Büttner-Ennever JA. The neuroanatomical basis of slow saccades in spinocerebellar ataxia type 2 (Wadia-subtype). Prog Brain Res. 2008;171:575–81. https://doi.org/10.1016/S0079-6123(08)00683-3.
Rüb U, Bürk K, Schöls L, et al. Damage to the reticulotegmental nucleus of the pons in spinocerebellar ataxia type 1, 2, and 3. Neurology. 2004;63(7):1258–63. https://doi.org/10.1212/01.WNL.0000140498.24112.8C.
Acknowledgments
Professor Márcia Olandowski provided the statistical analysis of the study.
Author information
Authors and Affiliations
Contributions
Research project: conception—Gustavo L. Franklin, Fabio Nascimento, Hélio A. G. Teive; organization—Gustavo L. Franklin, Alex T. Meira, Carlos Henrique F. Camargo, Fabio Nascimento, Hélio A. G. Teive; execution—Gustavo L. Franklin, Alex T. Meira, Carlos Henrique F. Camargo, Fabio Nascimento, Hélio A. G. Teive
Manuscript preparation: writing of the first draft—Gustavo L. Franklin, Fabio Nascimento, Hélio A. G. Teive; review and critique—Gustavo L. Franklin, Alex T. Meira, Carlos Henrique F. Camargo, Fabio Nascimento, Hélio A. G. Teive
Statistics: acquisition of data—Gustavo L. Franklin; analysis—Gustavo L. Franklin, Carlos Henrique F. Camargo; interpretation of data—Gustavo L. Franklin, Alex T. Meira, Carlos Henrique F. Camargo
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• The presence of upward gaze palsy (UGP) is statistically higher in SCA3 patients.
• UGP is characteristic of SCA3 and of great value to distinguish from others spinocerebellar ataxias
• “Coutinho’s sign” should be used to describe the UGP in SCA3 patients.
Rights and permissions
About this article
Cite this article
Franklin, G.L., Meira, A.T., Camargo, C.H.F. et al. Upward Gaze Palsy: a Valuable Sign to Distinguish Spinocerebellar Ataxias. Cerebellum 19, 685–690 (2020). https://doi.org/10.1007/s12311-020-01154-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-020-01154-2