Abstract
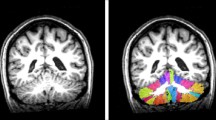
Whole-brain voxel-based morphometry (VBM) studies revealed patterns of patchy atrophy within the cerebellum of Friedreich’s ataxia patients, missing clear clinico-anatomic correlations. Studies so far are lacking an appropriate registration to the infratentorial space. To circumvent these limitations, we applied a high-resolution atlas template of the human cerebellum and brainstem (SUIT template) to characterize regional cerebellar atrophy in Friedreich’s ataxia (FRDA) on 3-T MRI data. We used a spatially unbiased voxel-based morphometry approach together with T2-based manual segmentation, T2 histogram analysis, and atlas generation of the dentate nuclei in a representative cohort of 18 FRDA patients and matched healthy controls. We demonstrate that the cerebellar volume in FRDA is generally not significantly different from healthy controls but mild lobular atrophy develops beyond normal aging. The medial parts of lobule VI, housing the somatotopic representation of tongue and lips, are the major site of this lobular atrophy, which possibly reflects speech impairment. Extended white matter affection correlates with disease severity across and beyond the cerebellar inflow and outflow tracts. The dentate nucleus, as a major site of cerebellar degeneration, shows a mean volume loss of about 30%. Remarkably, not the atrophy but the T2 signal decrease of the dentate nuclei highly correlates with disease duration and severity.




Similar content being viewed by others
Data Availability
The dentate atlases of FRDA patients and normal controls will be made available by the authors on request. Requests can be made via e-mail to either Tobias Lindig (Tobias.Lindig@med.uni-tuebingen.de) or Benjamin Bender (Benjamin.Bender@med.uni-tuebingen.de).
Abbreviations
- CSF:
-
Cerebrospinal fluid
- DN:
-
Dentate nucleus
- DTI:
-
Diffusion tensor imaging
- FRDA:
-
Friedreich’s ataxia
- FSL:
-
FMRIB software library
- FWE:
-
Family-wise error
- FWHM:
-
Full width at half maximum
- GAA:
-
Guanine-adenine-adenine
- GM:
-
Gray matter
- QSM:
-
Quantitative susceptibility mapping
- ROI:
-
Region of interest
- SARA:
-
Scale for the assessment and rating of ataxia
- SD:
-
Standard deviation
- SUIT:
-
Spatially unbiased infratentorial template
- TFCE:
-
Threshold-free cluster enhancement
- TIV:
-
Total intracranial volume
- VBM:
-
Voxel-based morphometry
- WM:
-
White matter
References
Reetz K, Dogan I, Hohenfeld C, Didszun C, Giunti P, Mariotti C, et al. Nonataxia symptoms in Friedreich ataxia: report from the registry of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS). Neurology. 2018;91(10):e917–e30.
Reetz K, Dogan I, Costa AS, Dafotakis M, Fedosov K, Giunti P, et al. Biological and clinical characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS) cohort: a cross-sectional analysis of baseline data. Lancet Neurol. 2015;14(2):174–82.
Schmucker S, Puccio H. Understanding the molecular mechanisms of Friedreich’s ataxia to develop therapeutic approaches. Hum Mol Genet. 2010;19(R1):R103–10.
Pastore A, Puccio H. Frataxin: a protein in search for a function. J Neurochem. 2013;126(Suppl 1):43–52.
Koeppen AH, Mazurkiewicz JE. Friedreich ataxia: neuropathology revised. J Neuropathol Exp Neurol. 2013;72(2):78–90.
Pagani E, Ginestroni A, Della Nave R, Agosta F, Salvi F, De Michele G, et al. Assessment of brain white matter fiber bundle atrophy in patients with Friedreich ataxia. Radiology. 2010;255(3):882–9.
Della Nave R, Ginestroni A, Tessa C, Salvatore E, Bartolomei I, Salvi F, et al. Brain white matter tracts degeneration in Friedreich ataxia. An in vivo MRI study using tract-based spatial statistics and voxel-based morphometry. NeuroImage. 2008;40(1):19–25.
Solbach K, Kraff O, Minnerop M, Beck A, Schols L, Gizewski ER, et al. Cerebellar pathology in Friedreich’s ataxia: atrophied dentate nuclei with normal iron content. Neuroimage Clin. 2014;6:93–9.
Waldvogel D, van Gelderen P, Hallett M. Increased iron in the dentate nucleus of patients with Friedrich’s ataxia. Ann Neurol. 1999;46(1):123–5.
Rezende TJ, Silva CB, Yassuda CL, Campos BM, D’Abreu A, Cendes F, et al. Longitudinal magnetic resonance imaging study shows progressive pyramidal and callosal damage in Friedreich’s ataxia. Mov Disord. 2016;31(1):70–8.
Selvadurai LP, Harding IH, Corben LA, Stagnitti MR, Storey E, Egan GF, et al. Cerebral and cerebellar grey matter atrophy in Friedreich ataxia: the IMAGE-FRDA study. J Neurol. 2016;263:2215–23.
Della Nave R, Ginestroni A, Giannelli M, Tessa C, Salvatore E, Salvi F, et al. Brain structural damage in Friedreich’s ataxia. J Neurol Neurosurg Psychiatry. 2008;79(1):82–5.
Burk K, Malzig U, Wolf S, Heck S, Dimitriadis K, Schmitz-Hubsch T, et al. Comparison of three clinical rating scales in Friedreich ataxia (FRDA). Mov Disord. 2009;24(12):1779–84.
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Diedrichsen J. A spatially unbiased atlas template of the human cerebellum. NeuroImage. 2006;33(1):127–38.
Diedrichsen J, Balsters JH, Flavell J, Cussans E, Ramnani N. A probabilistic MR atlas of the human cerebellum. NeuroImage. 2009;46(1):39–46.
Ashburner J, Friston KJ. Voxel-based morphometry—the methods. NeuroImage. 2000;11(6):805–21.
Ashburner J, Friston KJ. Unified segmentation. NeuroImage. 2005;26(3):839–51.
Rorden C, Brett M. Stereotaxic display of brain lesions. Behav Neurol. 2000;12(4):191–200.
Salimi-Khorshidi G, Smith SM, Nichols TE. Adjusting the effect of nonstationarity in cluster-based and TFCE inference. NeuroImage. 2011;54(3):2006–19.
Smith SM, Nichols TE. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage. 2009;44(1):83–98.
Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE. Permutation inference for the general linear model. NeuroImage. 2014;92:381–97.
Diedrichsen J, Zotow E. Surface-based display of volume-averaged cerebellar imaging data. PLoS One. 2015;10(7):e0133402.
Ridgway GR, Barnes J, Pepple T, Fox N, editors. Estimation of total intracranial volume: a comparison of methods. AAICAD Alzheimer’s imaging consortium; Paris, France; 2011.
Malone IB, Leung KK, Clegg S, Barnes J, Whitwell JL, Ashburner J, et al. Accurate automatic estimation of total intracranial volume: a nuisance variable with less nuisance. NeuroImage. 2015;104:366–72.
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. NeuroImage. 2006;31(3):1116–28.
Diedrichsen J, Maderwald S, Kuper M, Thurling M, Rabe K, Gizewski ER, et al. Imaging the deep cerebellar nuclei: a probabilistic atlas and normalization procedure. NeuroImage. 2011;54(3):1786–94.
Harding IH, Corben LA, Storey E, Egan GF, Stagnitti MR, Poudel GR, et al. Fronto-cerebellar dysfunction and dysconnectivity underlying cognition in friedreich ataxia: the IMAGE-FRDA study. Hum Brain Mapp. 2016;37(1):338–50.
Stefanescu MR, Dohnalek M, Maderwald S, Thurling M, Minnerop M, Beck A, et al. Structural and functional MRI abnormalities of cerebellar cortex and nuclei in SCA3, SCA6 and Friedreich’s ataxia. Brain. 2015;138(Pt 5):1182–97.
Ginestroni A, Diciotti S, Cecchi P, Pesaresi I, Tessa C, Giannelli M, et al. Neurodegeneration in Friedreich’s ataxia is associated with a mixed activation pattern of the brain. A fMRI study. Hum Brain Mapp. 2012;33(8):1780–91.
Deistung A, Stefanescu MR, Ernst TM, Schlamann M, Ladd ME, Reichenbach JR, et al. Structural and functional magnetic resonance imaging of the cerebellum: considerations for assessing cerebellar ataxias. Cerebellum. 2016;15(1):21–5.
Dogan I, Tinnemann E, Romanzetti S, Mirzazade S, Costa AS, Werner CJ, et al. Cognition in Friedreich’s ataxia: a behavioral and multimodal imaging study. Ann Clin Transl Neurol. 2016;3(8):572–87.
Selvadurai LP, Harding IH, Corben LA, Georgiou-Karistianis N. Cerebral abnormalities in Friedreich ataxia: a review. Neurosci Biobehav Rev. 2018;84:394–406.
Grodd W, Hulsmann E, Lotze M, Wildgruber D, Erb M. Sensorimotor mapping of the human cerebellum: fMRI evidence of somatotopic organization. Hum Brain Mapp. 2001;13(2):55–73.
Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106(5):2322–45.
Ackermann H, Brendel B. Cerebellar contributions to speech and language. In: Hickok G, Small SL, editors. Neurobiology of language. Elsevier; 2016.
Schols L, Amoiridis G, Przuntek H, Frank G, Epplen JT, Epplen C. Friedreich’s ataxia. Revision of the phenotype according to molecular genetics. Brain. 1997;120(Pt 12):2131–40.
Delatycki MB, Paris DB, Gardner RJ, Nicholson GA, Nassif N, Storey E, et al. Clinical and genetic study of Friedreich ataxia in an Australian population. Am J Med Genet. 1999;87(2):168–74.
Brendel B, Ackermann H, Berg D, Lindig T, Scholderle T, Schols L, et al. Friedreich ataxia: dysarthria profile and clinical data. Cerebellum. 2013;12(4):475–84.
Folker J, Murdoch B, Cahill L, Delatycki M, Corben L, Vogel A. Dysarthria in Friedreich’s ataxia: a perceptual analysis. Folia Phoniatr Logop. 2010;62(3):97–103.
Mascalchi M. The cerebellum looks normal in Friedreich ataxia. AJNR Am J Neuroradiol. 2013;34(2):E22.
Anheim M, Tranchant C, Koenig M. The autosomal recessive cerebellar ataxias. N Engl J Med. 2012;366(7):636–46.
Jacobi H, Hauser TK, Giunti P, Globas C, Bauer P, Schmitz-Hubsch T, et al. Spinocerebellar ataxia types 1, 2, 3 and 6: the clinical spectrum of ataxia and morphometric brainstem and cerebellar findings. Cerebellum. 2012;11(1):155–66.
Koeppen AH, Davis AN, Morral JA. The cerebellar component of Friedreich’s ataxia. Acta Neuropathol. 2011;122(3):323–30.
Koeppen AH, Ramirez RL, Becker AB, Feustel PJ, Mazurkiewicz JE. Friedreich ataxia: failure of GABA-ergic and glycinergic synaptic transmission in the dentate nucleus. J Neuropathol Exp Neurol. 2015;74(2):166–76.
Boddaert N, Le Quan Sang KH, Rotig A, Leroy-Willig A, Gallet S, Brunelle F, et al. Selective iron chelation in Friedreich ataxia: biologic and clinical implications. Blood. 2007;110(1):401–8.
Bonilha da Silva C, Bergo FP, D’Abreu A, Cendes F, Lopes-Cendes I, Franca MC Jr. Dentate nuclei T2 relaxometry is a reliable neuroimaging marker in Friedreich’s ataxia. Eur J Neurol. 2014;21(8):1131–6.
Koeppen AH, Michael SC, Knutson MD, Haile DJ, Qian J, Levi S, et al. The dentate nucleus in Friedreich’s ataxia: the role of iron-responsive proteins. Acta Neuropathol. 2007;114(2):163–73.
Koeppen AH, Ramirez RL, Yu D, Collins SE, Qian J, Parsons PJ, et al. Friedreich’s ataxia causes redistribution of iron, copper, and zinc in the dentate nucleus. Cerebellum. 2012;11(4):845–60.
Harding IH, Raniga P, Delatycki MB, Stagnitti MR, Corben LA, Storey E, et al. Tissue atrophy and elevated iron concentration in the extrapyramidal motor system in Friedreich ataxia: the IMAGE-FRDA study. J Neurol Neurosurg Psychiatry. 2016;87:1261–3.
van Baarsen KM, Kleinnijenhuis M, Jbabdi S, Sotiropoulos SN, Grotenhuis JA, van Cappellen van Walsum AM. A probabilistic atlas of the cerebellar white matter. NeuroImage. 2016;124(Pt A):724–32.
Eklund A, Nichols TE, Knutsson H. Cluster failure: why fMRI inferences for spatial extent have inflated false-positive rates. Proc Natl Acad Sci U S A. 2016;113(28):7900–5.
Eklund A, Andersson M, Knutsson H. Fast random permutation tests enable objective evaluation of methods for single-subject FMRI analysis. Int J Biomed Imaging. 2011;2011:627947.
Web References
Brain and Mind Institute, University of Western Ontario, Canada. Spatially unbiased infratentorial template for normalization of cerebellum and brainstem (SUIT). http://www.diedrichsenlab.org/imaging/suit.htm (last accessed 14.05.)
Wellcome Trust Centre for Neuroimaging, London, UK. Statistical Parameter Mapping (SPM). http://www.fil.ion.ucl.ac.uk/spm/ (last accessed 14.05.)
Chris Rorden’s Neuropsychology Lab, University of South Carolina, USA. MRIcron. http://www.mccauslandcenter.sc.edu/crnl/tools (last accessed 14.05.)
Structural Brain Mapping Group, University of Jena, Germany. Voxel Based Morphometry toolbox (VBM8). http://www.neuro.uni-jena.de/vbm/download/ (last accessed 14.05.) and http://www.neuro.uni-jena.de/vbm/check-sample-homogeneity/ (last accessed 14.05.)
Center for Investigating Healthy Minds, University of Wisconsin-Madison, USA. Mean centering continuous covariates. http://www.mumford.fmripower.org/mean_centering/ (last accessed 14.05.)
FMRIB, Oxford, UK. FMRIB Software Library (fsl). https://fsl.fmrib.ox.ac.uk/fsl/ (last accessed 14.05.)
Penn Image Computing and Science Laboratory, and Scientific Computing and Imaging Institute, University of Pennsylvania and University of Utah, USA. ITK-SNAP. http://www.itksnap.org/pmwiki/pmwiki.php (last accessed 14.05.)
Acknowledgments
The authors wish to thank Merim Bilalic and Matthew Bladen for proof-reading of the manuscript and language editing.
Funding
This work was supported by the European Union by a grant to EFACTS (HEALTH-F2-2010-242193) and the Else-Kröner Fresenius Stiftung (to MS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Lindig, T., Bender, B., Kumar, V.J. et al. Pattern of Cerebellar Atrophy in Friedreich’s Ataxia—Using the SUIT Template. Cerebellum 18, 435–447 (2019). https://doi.org/10.1007/s12311-019-1008-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-019-1008-z