Abstract
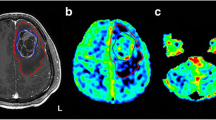
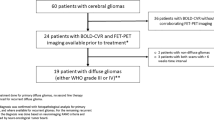
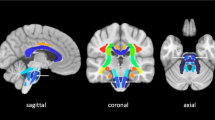
Decreased cerebral blood volume (CBV) in contralateral cerebellar gray matter (cGM) in conjunction with cerebellar white matter (cWM) damage, consistent with crossed cerebro-cerebellar diaschisis (cCCD) develop following supratentorial hemispheric stroke. In this study, we investigated the longitudinal evolution of diaschisis-related cerebellar perfusion and diffusion tensor-imaging (DTI) changes in patients after surgery for supratentorial brain tumors. Eight patients (M:F 5:3, age 8–22 years) who received surgery for supratentorial high-grade gliomas were evaluated. Initial MRI studies were performed 19–54 days postoperatively, with follow-ups at 2- to 3-month intervals. For each study, parametric maps of the cerebellum were generated and coregistered to T1-weighted images that had been previously segmented for cGM and cWM. Aggregate mean values of CBV, cerebral blood flow (CBF), and fractional anisotropy (FA) were obtained separately for cGM and cWM, and asymmetry indices (AIs) were calculated. Hemodynamic changes were more robust in cGM than in cWM. Seven patients showed decreased perfusion within cGM contralateral to the supratentorial lesion on the first postoperative study, and asymmetry was significant for both CBV (p = 0.008) and CBF (p < 0.01). For CBV, follow-up studies showed a significant trend towards recovery (p < 0.02). DTI changes were more pronounced in cWM. FA values suggested a “paradoxical” increase at initial follow-up, but steadily declined thereafter (p = 0.0003), without evidence of subsequent recovery. Diaschisis-related hemodynamic alterations within cGM appear on early postoperative studies, but CBV recovers over time. Conversely, cWM DTI changes are delayed and progressive. Although the clinical correlates of cCCD are yet to be elucidated, better understanding of longitudinal structural and hemodynamic changes within brain remote from the area of primary insult could have implications in research and clinical rehabilitative strategies.



Similar content being viewed by others
References
Shih WJ, Huang WS, Milan PP. F-18 FDG PET demonstrates crossed cerebellar diaschisis 20 years after stroke. Clin Nucl Med. 2006;31(5):259–61.
Kajimoto K, Oku N, Kimura Y, Kato H, Tanaka MR, Kanai Y, et al. Crossed cerebellar diaschisis: a positron emission tomography study with l-[methyl-11C]methionine and 2-deoxy-2-[18F]fluoro-d-glucose. Ann Nucl Med. 2007;21(2):109–13.
Krishnananthan R, Minoshima S, Lewis D. Tc-99 m ECD neuro-SPECT and diffusion weighted MRI in the detection of the anatomical extent of subacute stroke: a cautionary note regarding reperfusion hyperemia. Clin Nucl Med. 2007;32(9):700–2.
Yamada H, Koshimoto Y, Sadato N, Kawashima Y, Tanaka M, Tsuchida C, et al. Crossed cerebellar diaschisis: assessment with dynamic susceptibility contrast MR imaging. Radiology. 1999;210(2):558–62.
Kim J, Lee SK, Lee JD, Kim YW, Kim DI. Decreased fractional anisotropy of middle cerebellar peduncle in crossed cerebellar diaschisis: diffusion-tensor imaging-positron-emission tomography correlation study. AJNR Am J Neuroradiol. 2005;26(9):2224–8.
Lin DD, Kleinman JT, Wityk RJ, Gottesman RF, Hillis AE, Lee AW, et al. Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol. 2009;30(4):710–5.
Team RDC. A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2011.
Brunberg JA, Frey KA, Horton JA, Kuhl DE. Crossed cerebellar diaschisis: occurrence and resolution demonstrated with PET during carotid temporary balloon occlusion. AJNR Am J Neuroradiol. 1992;13(1):58–61.
Reese TG, Heid O, Weisskoff RM, Wedeen VJ. Reduction of eddy-current-induced distortion in diffusion MRI using a twice-refocused spin echo. Magn Reson Med. 2003;49(1):177–82.
Ashburner J, Friston KJ. Voxel-based morphometry—the methods. Neuroimage. 2000;11(6 Pt 1):805–21.
Miller NG, Reddick WE, Kocak M, Glass JO, Lobel U, Morris B, et al. Cerebellocerebral diaschisis is the likely mechanism of postsurgical posterior fossa syndrome in pediatric patients with midline cerebellar tumors. AJNR Am J Neuroradiol. 2010;31(2):288–94.
Di Costanzo A, Trojsi F, Giannatempo GM, Vuolo L, Popolizio T, Catapano D, et al. Spectroscopic, diffusion and perfusion magnetic resonance imaging at 3.0 Tesla in the delineation of glioblastomas: preliminary results. J Exp Clin Cancer Res. 2006;25(3):383–90.
Fox RJ, Sakaie K, Lee JC, Debbins JP, Liu Y, Arnold DL, et al. A validation study of multicenter diffusion tensor imaging: reliability of fractional anisotropy and diffusivity values. AJNR Am J Neuroradiol. 2012;72(2):89–96.
Sobesky J, Thiel A, Ghaemi M, Hilker RH, Rudolf J, Jacobs AH, et al. Crossed cerebellar diaschisis in acute human stroke: a PET study of serial changes and response to supratentorial reperfusion. J Cereb Blood Flow Metab. 2005;25(12):1685–91.
Flint AC, Naley MC, Wright CB. Ataxic hemiparesis from strategic frontal white matter infarction with crossed cerebellar diaschisis. Stroke. 2006;37(1):e1–2.
Gorman MJ, Dafer R, Levine SR. Ataxic hemiparesis: critical appraisal of a lacunar syndrome. Stroke. 1998;29(12):2549–55.
Szilagyi G, Vas A, Kerenyi L, Nagy Z, Csiba L, Gulyas B. Correlation between crossed cerebellar diaschisis and clinical neurological scales. Acta Neurol Scand. 2012;125:373–81.
Goldsberry G, Mitra D, MacDonald D, Patay Z. Accelerated myelination with motor system involvement in a neonate with immediate postnatal onset of seizures and hemimegalencephaly. Epilepsy Behav. 2011;22(2):391–4.
Park CH, Chang WH, Ohn SH, Kim ST, Bang OY, Pascual-Leone A, et al. Longitudinal changes of resting-state functional connectivity during motor recovery after stroke. Stroke. 2011;42(5):1357–62.
Inman CS, James GA, Hamann S, Rajendra JK, Pagnoni G, Butler AJ. Altered resting-state effective connectivity of fronto-parietal motor control systems on the primary motor network following stroke. Neuroimage. 2012;59(1):227–37.
Acknowledgments
The authors thank Cherise M. Guess for reviewing and editing the manuscript.
Conflict of Interest
AB received partial financial support for this research from OSI Pharmaceuticals and Genentech ZP, CP, YL, MS, AB, and RJO received partial support from the US National Institutes of Health Cancer Center Support (CORE) Grant P30 CA21765 and the American Lebanese Syrian Associated Charities (ALSAC) while conducting this research.
The other authors declare no conflict of interest with regard to the subject matter presented in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patay, Z., Parra, C., Hawk, H. et al. Quantitative Longitudinal Evaluation of Diaschisis-Related Cerebellar Perfusion and Diffusion Parameters in Patients with Supratentorial Hemispheric High-Grade Gliomas After Surgery. Cerebellum 13, 580–587 (2014). https://doi.org/10.1007/s12311-014-0575-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-014-0575-2