Abstract
To determine the relative frequency and change of malignant lymphoma in Korea according to the 4th World Health Organization (WHO) classification and compare with previous reports. Between 2015 and 2016, 7737 new patients with malignant lymphoma were enrolled from 31 institutes, with their clinicopathologic information obtained, and evaluated for the relative frequency of lymphoma subtypes. The relative frequency of non-Hodgkin lymphoma (NHL) was 94.8%, and that of Hodgkin lymphoma (HL) was 5.2%. B cell lymphomas accounted for 83.1% of all NHLs; T/natural killer (NK) cell lymphomas, 16.4%; and immunodeficiency-associated lymphoproliferative disorders, 0.5%. The most common NHL subtypes were diffuse large B cell (41.5%), extranodal marginal zone (MALT, 19.8%), follicular (7.5%), NK/ T cell (4.2%), and peripheral T cell lymphomas, not otherwise specific (PTCL, NOS, 3.4%). Nodular sclerosis was the predominant HL subtype (48.5%), followed by mixed cellularity (28.7%), lymphocyte-rich (6.8%), lymphocyte-depleted (1.5%), lymphocyte-predominant (2.8%), and unclassified HL (11.8%). Compared with a previous report, increased B cell lymphomas (77.6–83.1%) and slightly decreased NK/T cell lymphomas and PTCL were observed. The incidence of follicular lymphoma increased by more than 2.5-fold (2.9–7.5%). Incidence rates of newly diagnosed lymphomas were lower for HL and higher for extranodal NHL, MALT, and nasal type NK/T cell lymphomas in Korea than those in Western countries. A slight increase in the relative frequency of B cell lymphoma and a prominent increase in follicular lymphoma may be attributed to refined diagnostic criteria and Westernized disease patterns.
Similar content being viewed by others
Background and aim
Malignant lymphoma represents a diverse group of malignant lymphoid neoplasms comprising B, T, and natural killer (NK) cell lineage. The most recent World Health Organization (WHO) classification divides lymphoid neoplasms into more than 30 lymphoma entities based on the characteristics of neoplastic cells including morphology, immunophenotype, clinical findings (e.g., location of the lesion), and genetic changes [1]. The frequency of malignant lymphoma subtypes varies between geographic regions. The overall incidence of malignant lymphoma in Korea accounts for 2.2% based on the Korean national cancer statistics [2, 3]. Compared with Western countries, Asian regions report higher rates of T cell lymphoma and lower rates of follicular lymphoma (FL) and Hodgkin lymphoma (HL) [4,5,6,7,8]. Due to a novel therapeutic strategy and classification, a periodic survey based on new molecular targets for their diagnosis and treatment is mandatory. Because the frequency of each subtype provides fundamental information for malignant lymphoma research, the Hematopathology Study Group of the Korean Society of Pathologists carried out three nationwide studies: based on the Working Formulation in 1992, based on the revised European-American lymphoma (REAL) classification in 1998, and based on the WHO and determined according to the relative frequency of malignant lymphoma in 2011 [4,5,6].
Methods
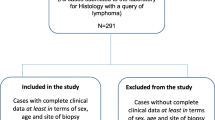
Between 2015 and 2016, this study enrolled patients newly diagnosed with malignant lymphoma and categorized into subtypes according to the 2008 WHO classification system, at 31 hospitals in Korea. All study participants were regular members of a Korean Study Group of Hematopathology. Cases with ambiguous diagnosis (e.g., malignant lymphoma, B cell phenotype) or duplicated cases due to hospital transfer were excluded. Parameters such as age, sex, and site of involvement were also obtained. Results were compared with those of the previously reported Korean studies. Statistical analysis was performed using the SPSS ver. 23.0 software (SPSS, Chicago, Illinois, USA). All procedures were approved by the respective institutional review boards of participating institutions.
Results
General features
Of the 8158 patients with lymphoid neoplasm enrolled between 2015 and 2016, 421 were excluded because of duplication (e.g., multiple site biopsies in a patient or transfer to another hospital) or ambiguity of diagnosis. The subtype distribution among 7737 study participants was as follows: 6095 (78.8%) had B cell lymphoma, 1206 (15.6%) had T/NK cell lymphoma, 400 (5.2%) had HL, and 36 (0.5%) had immunodeficiency-associated lymphoproliferative disorders (IDs). The overall male-to-female (MF) ratio of the patients was 1.3. Most lymphomas were predominant in men, with MF ratios of 1.3 for B cell lymphomas, 1.7 for T cell lymphomas, and 1.8 for HL. Among 7522 patients with available biopsy sites, 4782 (63.6%) occurred in extranodal sites and 2740 (36.4%) in the lymph nodes.
The most common lymphoma in Korean patients was diffuse large B cell lymphoma (DLBCL, 2680 patients, 34.6%), followed by extranodal marginal zone B cell lymphoma (MALT, 1455 patients, 18.8%), FL (549 patients, 7.1%), nasal type NK/T cell lymphoma (ENKTL, 310 patients, 4.0%), and peripheral T cell lymphoma, not otherwise specified (PTCL, NOS, 251 patients, 3.2%) (Table 1).
The age distribution was also evaluated among all patients with malignant lymphoma. The mean age of all patients was 58.6 years, with a subtype age distribution of 58.5 years for B cell lymphoma, 54 years for T cell lymphoma, and 42.7 years for HL. In contrast, ID was most prevalent (30.56%) in young patients aged ≤ 20 years (Fig. 1).
Age distribution of patients with malignant lymphoma in Korea. Each lymphoma is represented by a stacked bar graph according to age group. Lymphoma was most prevalent between the ages of 40 and 80 years. In HL lymphoma, 40% occurred in the 20–40 age. Immunodeficiency-associated LPD was frequent in children under 20 years of age. HL, Hodgkin lymphoma; B-NHL, B cell non-Hodgkin lymphoma; T-NHL, T cell non-Hodgkin lymphoma; ID, immunodeficiency-associated lymphoproliferative disorder
Anatomical sites of tissue sampling for lymphoid neoplasms
The distribution of diagnosis according to the anatomical site was evaluated in 7689 patients with malignant lymphoma. Among them, 4945 and 2744 patients were diagnosed with extranodal and nodal lymphomas, respectively. The most common subtype of extranodal lymphoma was extranodal DLBCL (39.7%), followed by extranodal MALT (29.1%), whereas nodal DLBCL (38.8%) and FL (14.6%) were the most common nodal lymphomas. The MF ratio was 1.4 for nodal lymphomas and 1.3 for extranodal lymphomas. Patients with nodal and extranodal lymphomas had a mean age of 56.8 and 56.9 years, respectively (Table 2). Commonly involved anatomical regions in the extranodal site were the gastrointestinal tract (35.7%), bone and soft tissue (10%), Waldeyer’s ring (7.1%), and the central nervous system (7.0%). MALT was the most common lymphoma of the gastrointestinal tract and eye, whereas ENKTL was the most common lymphoma of the nasal region (Table 3).
Subtype distribution of lymphoid neoplasms
B cell lymphoma
B cell lymphomas accounted for 83.1% of all NHL. DLBCL was the most common lymphoma in Korea (34.6%), followed by extranodal MALT (18.8%) and FL (7.1%). Among DLBCL subtypes, primary DLBCL in the central nervous system was the most common (278 patients; 9.1% of DLBCL and 3.6% of all malignant lymphomas). A total of 67 patients had Epstein-Barr virus (EBV)–positive DLBCL of the elderly comprised 67 cases (2.2% of DLBCL subtypes). Rare B cell lymphomas, e.g., primary effusion lymphoma and splenic marginal zone lymphoma were also observed.
Nodal and extranodal sites were differentiated, and the disease status was determined. The most common lymphoma for both sites was DLBCL (38.8% of nodal sites and 39.7% of extranodal sites). Extranodal MALT was the second most common extranodal B cell lymphoma (29.1%), and FL was the second most common nodal lymphoma (14.6%).
T cell lymphoma
The most common T cell lymphoma in Korea is ENKTL, followed by PTCL, NOS (3.2%), and angioimmunoblastic T cell lymphoma (AITL, 2.4%). Type 2 enteropathy-associated T cell lymphoma was more common in Korea (42 patients, 0.5%) compared with Western countries. This T cell lymphoma subtype was recently re-named as monomorphic epitheliotropic intestinal T cell lymphoma in the 2016 WHO classification. Rare T cell lymphomas, e.g., subcutaneous panniculitis-like T cell lymphoma, systemic EBV-positive childhood T-lymphoproliferative disorder, and hydroa vacciniforme–like lymphomas, were also observed.
The most frequent nodal T cell lymphoma was AITL (6.6%), followed by PTCL, NOS (5.8%), and T lymphoblastic lymphoma (1.9%). ENKTL (6.0%) was the most frequent extranodal T cell lymphoma, followed by PTCL (1.9%) and mycosis fungoides/Sezary syndrome (MF/SS, 1.3%).
HL
Classic HL (cHL) accounts for 97.5% of all HLs. Patients with HL, nodal sclerosis (NSHL, mean age 35.8 years) were younger than those with other subtypes such as mixed cellularity type (MCHL, 50.4 years). The incidence of NSHL was similar between men and women (MF ratio: 1.4). MCHL comprised approximately 25% of cHL with an M/F ratio of 2.6. HL mostly occurs in the lymph nodes (341/398 cases), with NSHL identified as the most common subtype (55% of all HL patients), followed by MCHL.
Comparing the current epidemiological data with the past prevalence data
The result in this study was compared with that in previous Korean reports [3,4,5,6], and an increasing trend on the total number of lymphomas in Korea was identified. According to reports of the Korean Statistical Office, a central organization for statistics under the Ministry of Strategy and Finance, 119 patients had HL in 1999, which increased to 271 in 2015. Similar increases were observed for the incidence of NHL, with 2088 patients in 1999 compared with 4396 in 2015 [2]. This trend becomes even more obvious when comparing the previous Korean data and that of other countries (Table 4).
The HL-to-NHL ratio cases did not change significantly. Among patients with HL, the incidence of NSHL increased and NLPHL decreased, whereas the incidence of B cell lymphoma increased in the patients with NHL. A similar tendency was also reported in other Korean studies [3]. DLBCL has been the most common B cell lymphoma subtype; however, its incidence is lower than that in decreased to previous studies. The proportion of DLBCL is also lower than that in previous studies (42.7% in 2011, 34.6% in 2017). In the case of extranodal MALT (18.8%), the second most common B cell lymphoma in Korea, the proportion was not markedly changed when compared with the rate observed in 1997 (16.7%) and 2001(19.0%). The most dramatic change in the incidence of B cell lymphomas was a 2.5-fold increase in FL. The overall incidence of FL in Korea is approximately 7%; however, the absolute incidence of FL was significantly higher compared with that in previous studies.
The frequency of ENKTL and PTCL, NOS has been decreased in this study. The ENKTL proportion was even higher in Korean studies conducted around 10 years ago (6.3–8.7%) than that in this study [3, 5]; therefore, the incidence of ENKTL appears to have declined during the last decade. However, the incidence of AITL increased (1.63% in 2011; 2.43% in 2017).
Discussion
Studies on malignant lymphoma have been consistently conducted in Korea during the last 20 years, and reports on Korean lymphoma distribution are regularly published. This study was conducted to investigate the distribution of malignant lymphoma subtypes in Korea between 2015 and 2016. The total number of lymphomas increased relative to previous studies, even though the numbers of patients’ contributing institutes remained similar [3]. These findings indicate that the incidence of malignant lymphoma is increasing in the Korean population. This is in agreement with figures obtained by the Korea National Statistical Office showing that the incidence of lymphomas in Koreans is increasing from 4.3 cases in 2000 to 6.0 in 2015 in 100,000 people [2]. The most recent Korean cohort revealed annual age-standardized incidence rates of 0.46 (HL), 6.60 (B cell lymphoma), and 0.95 (T/NK) in 100,000 people [7]. Considering that the incidence of lymphoma is influenced by various environmental factors, further research is necessary to determine the cause of these changes in the incidence and distribution pattern of lymphoma in Korea.
FL is a relatively common lymphoma in Western countries [9, 11,12,13,14]. In this study, we found that the prevalence of FL was also increased in Korea. A recent report also showed an increasing prevalence of FL in Japan, with 6% between 1996 and 2000, 18.3% between 2000 and 2006, and 22.4% between 2007 and 2014 [15]. The age of onset for FL was also found to be lower (52–54 years) in Asian countries than that in international studies (59 years) [16]. The mean age of onset for FL was found to be 52.7 years in this study, which is similar to the 52.5 years reported in other Korean studies [6], 54 years in Southwest China [17], and 52 years in Eastern India [18]. Although the cause of this observation remains unclear, the prevalence of FL in Eastern countries tends to be increasing. Therefore, careful pathological evaluation considering the effects of updated FL classification is increasingly important.
The frequency of ENKTL has been decreased in this study. Previous studies showed that ENKTL was more frequent in Korea than in Western countries [3, 5, 6]. In a study conducted in the USA, ENKTL proportion was reported as 0.21–1.67% depending on race [9], whereas it was 4% in this study and therefore higher than that reported in the USA. The ENKTL proportion was even higher in Korean studies conducted about 10 years ago (6.3–8.7%) than this study [4, 7]; therefore, ENKTL appears to have declined in the last decade. This observed trend is consistent with other Korean studies reported in 2010 [7]; however, the exact cause for this decline has not been determined yet.
Sixty-seven patients with EBV-positive DLBCL of the elderly were included in this study (2.2% of DLBCL subtypes). A Japanese study reported a 6.9% rate of EBV-positive DLBCL in immunocompetent patients with large B cell lymphoproliferative disorder patients older than 60 years, and poor prognostic outcomes were also reported [10]. Although regional differences were observed in the EBV prevalence, the number of patients with EBV-positive DLBCL in this study was higher than that in a Japanese study. Because EBV-positive DLBCL has a poor prognosis, more active EBV screening will be required in Korea, particularly in the elderly.
Moreover, the proportion of extranodal MALT among patients with B cell lymphoma is higher than in Korea than that in other countries, whereas ENKTL showed a higher prevalence among T cell lymphomas. The overall distribution of malignant lymphoma types identified in this study was similar to the results of previous Korean studies; however, certain remarkable changes, such as increased FL and AITL incidence, were observed.
Some Eastern countries, such as Japan, Hong Kong, and Korea, showed similar malignant lymphoma subtype distribution with that of Western countries [9]. Europe and the USA report a higher frequency of HL, chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), DLBCL, FL, and plasma cell neoplasm, whereas Eastern countries show higher frequency of T cell lymphomas including NK/T cell lymphoma.
In Korea, bone marrow specimens are occasionally not referred to the pathology department. Therefore, we could not determine the exact distribution pattern of lymphocytic neoplasms involving the bone marrow such as lymphoblastic lymphomas, SLL, or plasmacytoma. Nevertheless, this large-scale study provides the most recent data on the lymphoma occurrence in Korea, including about 80% of all patients obtained for the Korean national cancer statistics [2].
In this study, HL rates were lower and extranodal MALT and ENKTL rates were higher in Korean patients with lymphoma than those in Western countries. Slight changes in the relative frequency of B cell lymphoma, but not T cell lymphomas, were observed. Increased FL incidence can likely be attributed to refined diagnostic criteria and Westernized disease patterns. Although this study has several limitations, e.g., difficulty of comparing the eras of lymphoma classification, this study provides significant findings as it includes majority of patients with lymphoma and reports the actual incidence of malignant lymphoma subtypes in Korea; this data will be fundamental for future studies on lymphoma.
References
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al (2008) WHO classification of tumours of haematopoietic and lymphoid tissues, 4th edn. IARC Press Lyon
Korea, S.; Available from: http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv
Lee H, Park HJ, Park E-H, Ju HY, Oh C-M, Kong HJ et al (2018) Nationwide statistical analysis of lymphoid malignancies in Korea. Cancer Res Treat 50(1):222–238
Kim, J.M., et al., WHO classification of malignant lymphomas in Korea: report of the third nationwide study. Korean J Pathol, 2011. 45(45): p. 254-260
Kim JM, Ko YH, Lee SS, Huh J, Kang CS, Kim CW, Kang YK, Go JH, Kim MK, Kim WS, Kim YJ, Kim HJ, Kim HK, Nam JH, Moon HB, Park CK, Park TI, Oh YH, Lee DW, Lee JS, Lee J, Lee H, Lim SC, Jang KY, Chang HK, Jeon YK, Jung HR, Cho MS, Cha HJ, Choi SJ, Han JH, Hong SH, Kim I (2011) WHO classification of malignant lymphomas in Korea: report of the third nationwide study. Korean J Pathol 45(3):254–260
Kim CW, Cho I, Ko YH, Cho H, Yang WI, Kwon GY et al (1992) Clinicopathologic and immunophenotypic study of non-Hodgkin’s lymphoma in Korea. Lymphoreticular study group of the Korean society of pathologists. J Korean Med Sci 7:193–198
Yoon SO, Suh C, Lee DH, Chi HS, Park CJ, Jang SS, Shin HR, Park BH, Huh J (2010) Distribution of lymphoid neoplasms in the Republic of Korea: analysis of 5318 cases according to the World Health Organization classification. Am J Hematol 85(10):760–764
Intragumtornchai T, Bunworasate U, Wudhikarn K, Lekhakula A, Julamanee J, Chansung K et al (2018) Non-Hodgkin lymphoma in South East Asia: an analysis of the histopathology, clinical features, and survival from Thailand. Hematol Oncol 36(1):28–36
Al-Hamadani M et al (2015) Non-Hodgkin lymphoma subtype distribution, geodemographic patterns, and survival in the US: a longitudinal analysis of the National Cancer Data Base from 1998 to 2011. Am J Hematol 90(9):790–795
Oyama T, Yamamoto K, Asano N, Oshiro A, Suzuki R, Kagami Y, Morishima Y, Takeuchi K, Izumo T, Mori S, Ohshima K, Suzumiya J, Nakamura N, Abe M, Ichimura K, Sato Y, Yoshino T, Naoe T, Shimoyama Y, Kamiya Y, Kinoshita T, Nakamura S (2007) Age-related EBV-associated B-cell lymphoproliferative disorders constitute a distinct clinicopathologic group: a study of 96 patients. Clin Cancer Res 13(17):5124–5132
Monabati A, Safaei A, Noori S, Mokhtari M, Vahedi A (2016) Subtype distribution of lymphomas in south of Iran, analysis of 1085 cases based on World Health Organization classification. Ann Hematol 95(4):613–618
Aoki R, Karube K, Sugita Y, Nomura Y, Shimizu K, Kimura Y, Hashikawa K, Suefuji N, Kikuchi M, Ohshima K (2008) Distribution of malignant lymphoma in Japan: analysis of 2260 cases, 2001-.2006. Pathol Int 58(3):174–182
Sun J, Yang Q, Lu Z, He M, Gao L, Zhu M, Sun L, Wei L, Li M, Liu C, Zheng J, Liu W, Li G, Chen J (2012) Distribution of lymphoid neoplasms in China: analysis of 4,638 cases according to the World Health Organization classification. Am J Clin Pathol 138(3):429–434
Chuang S-S, Chen SW, Chang ST, Kuo YT (2017) Lymphoma in Taiwan: review of 1347 neoplasms from a single institution according to the 2016 revision of the World Health Organization classification. J Formos Med Assoc 116(8):620–625
Muto R, Miyoshi H, Sato K, Furuta T, Muta H, Kwamoto K, Yanagida E, Yamada K, Ohshima K (2018) Epidermiology and secular trned of malignant lymphoma in Japan: Analyisis of 9426 cases according to the World Health Organization classification. Cancer Med 7:5843–5858
No authors listed (1997) The non-Hodgkin's lymphoma classification project. A clinical evaluation of the international lymphoma study group classification of non-Hogkin's lymphoma. Blood. 89:3909–3918
Yang QP, Zhang WY, Yu JB, Zhao S, Xu H, Wang WY et al (2011) Subtype distribution of lymphomas in Southwest China: analysis of 6,382 cases using WHO classification in a single institution. Dignostic Pathol 6:77
Monadal SK, Manal PK, Samanta TK, Chakaborty S, Roy SD, Roy S (2013) Malignant lymphoma in Estern India: a retrospective analysis of 455 cases according to WHO classification. Indian J Med Paediatr Oncol 34:242–246
Acknowledgments
This work was supported by the 2017 study group supporting program of the Korean Society of Pathologists.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were approved by the respective institutional review boards of participating institutions.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was supported by 2017’ Study group Supporting Program of Korean Society of Pathologists. The above co-authors are members of Korean Society of Hematopathology.
Rights and permissions
About this article
Cite this article
Jung, HR., Huh, J., Ko, YH. et al. Classification of malignant lymphoma subtypes in Korean patients: a report of the 4th nationwide study. J Hematopathol 12, 173–181 (2019). https://doi.org/10.1007/s12308-019-00369-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-019-00369-5