Abstract
Background
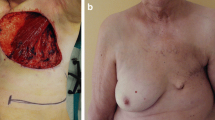
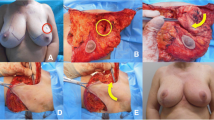
Oncoplastic breast conserving surgery had been challenged to achieve both of local control and the cosmetic appearance of preserved breast. We developed the lateral thoracoaxillar dermal-fat flap (LTDF) as an oncoplastic procedure to fill the defect of breast-conserving surgery in 1999.
Methods
A total of 2338 breast cancer patients underwent surgery from January, 2000 to December, 2017. Mastectomy was performed in 706 patients (30%), and breast conservative surgery (BCS) was performed in 1634 patients (70%). The LTDF was adopted in 487/1634 (30%) of BCS cases to fill the large defect left by partial resection. we divided all patients into 3 groups: breast total mastectomy (BT group), the breast partial resection (BP) with LTDF (LTDF group), and Bp without LTDF (BP group) and compared the clinical characteristics, and recurrence rate.
Results
The Indications for LTDF increased up to 40% in 2010, while they decreased to 20%–30% in the most recent period, in accordance with the frequency of breast reconstruction increased. Patients who underwent BP + LTDF (LTDF group) included significantly higher proportions of stage II diseases and cases treated by neoadjuvant chemotherapy than those in BP or BT groups.. We found no marked difference of local recurrence and distant metastases between the LTDF and Bp groups. However, the rate of distant metastasis was significantly higher in BT group than in the Bp or LTDF group. Concerning the complications of LTDF, we experienced a few complications of Grade 3–4 requiring surgical management, namely one case of dislocation of the LTDF, three cases of bleeding, and five cases each of skin necrosis and fat necrosis.
Conclusions
We reported satisfying long-term outcomes of 487 cases treated by LTDF. LTDF is a suitable oncoplastic technique for BCS.



Similar content being viewed by others
References
Fisher B, Anderson S, Redmond CK, Wolmark N, Wickerham DL, Cronin WM. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995;333:1456–61.
Anderson SJ, Wapnir I, Dignam JJ, Fisher B, Mamounas EP, Jeong JH, et al. Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five National Surgical Adjuvant Breast and Bowel Project protocols of node-negative breast cancer. J Clin Oncol. 2009;27:2466–73.
Fisher B, Bryant J, Dignam JJ, Wickerham DL, Mamounas EP, Fisher ER, et al. Tamoxifen, radiation therapy, or both for prevention of ipsilateral breast tumor recurrence after lumpectomy in women with invasive breast cancers of one centimeter or less. J Clin Oncol. 2002;20:4141–9.
Fisher B, Jeong JH, Anderson S, Wolmark N. Treatment of axillary lymph node-negative, estrogen receptor-negative breast cancer: updated findings from National Surgical Adjuvant Breast and Bowel Project clinical trials. J Natl Cancer Inst. 2004;96:1823–31.
Nakamura S, Kenjo H, Nishio T, Kazama T, Doi O, Suzuki K. Efficacy of 3D-MR mammography for breast conserving surgery after neoadjuvant chemotherapy. Breast Cancer. 2002;9:15–9.
Solin LJ, Orel SG, Hwang WT, Harris EE, Schnall MD. Relationship of breast magnetic resonance imaging to outcome after breast-conservation treatment with radiation for women with early-stage invasive breast carcinoma or ductal carcinoma in situ. J Clin Oncol. 2008;26:386–91.
Morrow M, Harris JR, Schnitt SJ. Surgical margins in lumpectomy for breast cancer–bigger is not better. N Engl J Med. 2012;367:79–82.
Azu M, Abrahamse P, Katz SJ, Jagsi R, Morrow M. What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol. 2010;17:558–63.
Masetti R, Di Leone A, Franceschini G, Magno S, Terribile D, Fabbri MC, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer: an overview. Breast J. 2006;12:174-80.
Clough KB, Lewis JS, Couturaud B, Fitoussi A, Nos C, Falcou MC. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg. 2003;237:26–34.
Petit JY, Rietjens M, Garusi C, Greuze M, Perry C. Integration of plastic surgery in the course of breast-conserving surgery for cancer to improve cosmetic results and radicality of tumor excision. Recent Results Cancer Res. 1998;152:202–11.
Kobayashi K, Nakagomi H. Oncoplastic breast conservingsurgery using Lateral thoracoaxillar dermal-fat flap. Pepers. 2011;52,41–46 (in Japanese).
Nakagomi H, Furuya K, Hinata M, Kobayashi K, Ohmori M, Kobayashi K. Lateral thoracoaxillar dermal-fat flap as an oncoplastic technique for breast conserving surgery. Jpn J Breast Cancer 2009;3,363–367 (in Japanese)
Noguchi M, Inokuchi M. “Moving window” operation for breast-conserving surgery. Breast Cancer. 2010;17:56–60.
Takeda M, Ishida T, Ohnuki K, Suzuki A, Kiyohara H, Moriya T, et al. Breast conserving surgery with primary volume replacement using a lateral tissue flap. Breast Cancer. 2005;12:16–20.
Ogawa T, Hanamura N, Yamashita M, Kimura H, Kashikura Y. Long-term results of breast volume replacement using an inframammary adipofascial flap after breast-conserving surgery. Breast Cancer. 2014;21:635–40.
Nakada H, Inoue M, Furuya K, Watanabe H, Ikegame K, Nakayama Y, et al. Fat necrosis after breast-conserving oncoplastic surgery. Breast Cancer. 2019;26:125–30.
Evans DG, Ingham SL, Baildam A, Ross GL, Lalloo F, Buchan I, et al. Contralateral mastectomy improves survival in women with BRCA1/2-associated breast cancer. Breast Cancer Res Treat. 2013;140:135–42.
Early Breast Cancer Trialists’. Collaborative G, Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011; 378: 1707–16.
Acknowledgements
This study was approved by the institutional review board at Yamanashi Central Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakagomi, H., Inoue, M., Nakada, H. et al. Lateral thoracoaxillar dermal-fat flap for breast conserving surgery: the changes of the indication and long-term results. Breast Cancer 26, 595–601 (2019). https://doi.org/10.1007/s12282-019-00959-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-019-00959-2