Abstract
Purpose of Review
Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) can increase the susceptibility of individuals to contracting mucormycosis through several mechanisms. Nowadays, coronavirus disease (COVID-19)-associated mucormycosis (CAM) is a serious public health concern, particularly in developing countries. This meta-analysis aims to identify the risk factors that affect the mortality rate of patients with CAM.
Recent Findings
We systematically searched PubMed, Google Scholar, Scopus, Cochrane library, and preprint databases using pertinent keywords and the reference lists of the included relevant articles from inception till October 27, 2021. In order to reduce the effects of small-scale studies, we only selected cross-sectional, case–control, and cohort studies and case series with at least four patients. We identified 26 articles that included 821 patients with CAM. The effect size (ES) of mortality rate was 28% (95% confidence interval (CI) 20%–38%; I2 =82.28%; p for Cochran Q<0.001). The CAM patients with a history of comorbidities other than diabetes (malignancies, transplant, or renal failure), mechanical ventilation due to COVID-19, pulmonary and cerebral mucormycosis, and those who only received medical treatment for mucormycosis had the highest mortality rate.
Summary
Coronavirus disease (COVID-19)-associated mucormycosis (CAM) is a major public health problem, particularly in developing countries. Severe COVID-19 infection, history of mechanical ventilation, early CAM, comorbidities other than diabetes (malignancies, transplant, or renal failure), pulmonary and rhino-orbito-cerebral mucormycosis, and delivering only medical treatment for mucormycosis were the worst prognostic factors in CAM patients. Identifying the mortality-related risk factors in CAM patients may help reduce the mortality rate by implementing optimized treatment approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A novel coronavirus (Severe Acute Respiratory Syndrome-Coronavirus-2:SARS-CoV-2) arose from China in late 2019 and rapidly spread worldwide and caused a sustained pandemic [1]. Mucormycosis is an invasive fungal infection that primarily affects individuals with a history of diabetes, neutropenia, hematologic malignancies, or chronic treatment with steroid/immunosuppressive drugs [2]. Thus far, hundreds of cases of coronavirus disease (COVID-19)-associated mucormycosis (CAM) have been reported in the literature [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. The causal relationship between COVID-19 and mucormycosis is still under debate; however, COVID-19 can promote the development of mucormycosis through several proposed mechanisms, including hypoxia, acidosis, hyperglycemia, cytokine storms, altered immune response, lymphopenia, endothelialitis, administration of systemic steroids/immunosuppressive drugs such as tocilizumab (anti-interleukin-6) and broad-spectrum antibiotics, impaired phagocytic activity, increased free iron and ferritin, overexpression of glucose-regulated protein 78(GRP 78), and Mucorales ligand spore coat protein homologs (Cot-H) [40,41,42]. Considering the widespread usage of systemic corticosteroids in the severely affected COVID-19 individuals and the pathogenic role of COVID-19 and steroids in the development of fungal infection, the prevalence of mucormycosis has rapidly risen in the years 2020–2021 compared with the previous years. Given the remarkable morbidity and mortality of CAM, it has become a paramount health concern, particularly in developing countries. In this study, we aimed to investigate the mortality rate in individuals with CAM and identify the mortality-related risk factors in these patients.
Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guideline [43] was used to perform our systematic review. The study protocol was registered in the international prospective register of systematic reviews (PROSPERO) (registration number: CRD42021279722). Besides, the ethics committee and institutional review board of Shiraz University of Medical Sciences reviewed and approved this study protocol (Approval No# IR.sums.med.rec.1400.452).
Literature Search Strategy
Two independent reviewers (HB and HK) performed a comprehensive systematic review from inception till October 27, 2021. The search was performed on PubMed, Scopus, Google Scholar, Cochrane library, and preprint (bioRxiv, medRxiv) databases. We searched using keywords, including (“mucormycosis” OR “phycomycosis” OR “mucorales” OR “zygomycosis” OR “mucor” OR “rhizopus” OR “rhizomucor” OR “cunninghamella” OR “lichtheimia” OR “cokeromyces” OR “actinomucor” OR “saksenaea” OR “apophysomyces” OR “syncephalastrum”) AND ( “COVID-19” OR “COVID” OR “2019 nCOV” OR “2019 novel coronavirus” OR “SARS-COV-2” OR “SARS-COV 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”). The reference lists of the selected articles and previous reviews were checked, and relevant studies were also included.
Study Selection
Eligibility Criteria
-
1-
Case series with at least four reported patients diagnosed with CAM, cross-sectional, case–control, and cohort studies.
-
2-
Patients with a confirmed diagnosis of COVID-19 (positive real-time polymerase chain reaction (RT-PCR) or antigen for SARS-CoV-2) either before or at the time of evolution of mucormycosis symptoms and signs. The interval between these two infections should not be more than three months.
-
3-
Histopathologic or microbiologic documentation of mucormycosis infection (proven cases of mucormycosis according to (EORTC/MSGERC) consensus [44].
-
4-
No language limitation.
Exclusion Criteria
-
1-
Systematic reviews, narrative reviews, editorials, commentary, and case reports.
-
2-
Case series with less than four patients (some studies reported four or more cases but proven CAM without other fungal co-infections were registered in fewer than four cases and were hence excluded).
-
3-
Patients without an established diagnosis of COVID-19 or mucormycosis.
-
4-
Patients with fungal infections other than mucormycosis or mixed fungal disease.
-
5-
Mortality rate not reported.
The characteristics of excluded studies are provided in Supplementary Table 1.
Data Extraction
Three independent investigators (HB, ZB, and SK) reviewed the searched articles and screened them, considering duplication and meeting the eligibility criteria as mentioned earlier. Any inconsistencies between the investigators’ findings were discussed with a senior reviewer (VRO) until an agreement was achieved. We collected the following data from the included articles: study characteristics; demographic data including age and sex; history of diabetes and other comorbidities (hematological malignancies, other types of malignancies, kidney disease, chronic liver disease, renal transplant, asthma and chronic obstructive pulmonary disease (COPD), neutropenia, human immunodeficiency virus (HIV), or tuberculosis); history of poor glycemic control (HbA1C≥10%) or diabetic ketoacidosis (DKA) during admission; severity of COVID-19 infection; history of mechanical ventilation due to COVID-19; the interval between COVID-19 and development of symptoms/signs related to mucormycosis (in pulmonary mucormycosis where the symptoms/signs related to mucormycosis overlap the COVID-19, the interval between the documented diagnosis of COVID-19 and mucormycosis was considered as a timeframe); history of steroid administration for COVID-19; clinical syndrome types of mucormycosis; treatment regimen of mucormycosis; and outcome (alive, or died). The severity of COVID-19 was determined according to World Health Organization (WHO) criteria [45]. We classified patients with mild or moderate severity as a non-severe group and those with severe or critical as a severe group. Moreover, we categorized patients with ≤7 days and >7-day intervals between COVID-19 and development of mucormycosis symptoms/signs as early and late CAM, respectively [46, 47]. We differentiated the clinical syndrome types of rhino-orbito-cerebral mucormycosis according to the guidelines for the diagnosis, staging, and management of rhino-orbito-cerebral mucormycosis in the setting of COVID-19 [48]: sinonasal/oronasal (involvement of nasal cavities (stage 1) with or without paranasal sinuses and/or palate/oral cavity(stage 2)); rhino-orbital/orbital (ROM) (involvement of nasolacrimal duct, eyeball, extraocular muscles, orbital cavity, central retinal artery/ophthalmic artery occlusion, or superior ophthalmic vein thrombosis with or without nasal cavities/paranasal sinuses(stage 3)); rhino-orbito-cerebral/rhino-cerebral(ROCM) (involvement of nasal cavities/paranasal sinuses and cavernous sinus, cavernous sinus thrombosis, internal carotid artery occlusion, brain parenchyma (infarct or abscess), skull base or dura mater with or without orbital cavity/extraocular muscles (stage 4)).
Quality Assessment of Study and Risk of Bias
The quality and risk of bias of case–control, cross-sectional, and case series studies were assessed using the Joanna Briggs Institute (JBI) critical appraisal checklists [49, 50]. We tried to avoid selection bias by contacting the corresponding authors for each manuscript in which the mortality-related prognostic variables and outcomes were not identified. In order to alleviate the effects of small-scale studies, we only included observational studies with four or more reported patients.
Outcome Measures
The primary outcome measure was the mortality-related risk factors for coronavirus disease (COVID-19)-associated mucormycosis. Secondary outcome measures consisted of the demographic, clinical characteristics, and mortality rate of patients with CAM.
Statistical Analysis
All statistical analyses were performed using STATA version 11.0 (Stata Corp., College Station, TX). Heterogeneity was evaluated using Cochran’s Q test and the I2statistic. I2 (>50%) with Cochrane’s Q test (p < 0.1) showed the presence of significant heterogeneity across the included articles. The mortality pooled prevalence with 95% confidence intervals (95% CIs) was estimated as summary effect size (ES). The MetaProp function using the random-effects model (DerSimonian–Laird method) was used to pool prevalence of mortality, and CIs were computed based on exact binomial procedures (Clopper–Pearson). For pooling outcomes with 0% or 100% across primary studies, Freeman–Tukey double arcsine transformation stabilized the variances. We performed additional analyses, including subgroup analyses by age (>55 years, ≤55 years); sex (male, female); history of diabetes and other comorbidities (positive, negative); history of poor glycemic control (HbA1C≥10%) or diabetic ketoacidosis (DKA) during admission (positive, negative); severity of COVID-19 infection (non-severe, severe); history of mechanical ventilation due to COVID-19 (positive, negative); the interval between COVID-19 and development of symptoms/signs related to mucormycosis (early CAM, late CAM); history of steroid administration for COVID-19 (positive, negative); clinical syndrome types of mucormycosis (sino-nasal/oronasal, ROM, ROCM, or pulmonary); treatment regimen of mucormycosis (only anti-fungal treatment, antifungal+ surgical debridement) to detect the source of heterogeneity based on some of moderators variables.
Results
Study Selection
The PRISMA flowchart (Fig. 1) demonstrated our search strategy for this review. The present investigation included 26 case series, cross-sectional, and case–control studies for the systematic review and meta-analysis, and the pooled data are extracted from 821 patients with CAM [6, 19, 27, 46, 51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Of these 26 studies, the case series, cross-sectional, and case–control studies were 18, 6, and 2, respectively. Twenty studies were reported from India, two from Iran, two from Egypt, one from Mexico, and one from Turkey. All of the included articles were written in the English language.
Quality Assessment of Study
The quality of the studies was evaluated according to JBI critical appraisal tools [49, 50]. The risk of bias assessment results of the included studies is summarized in Supplementary Table 2, Supplementary Table 3, and Supplementary Table 4. Overall, all of the included studies had acceptable quality and risk of bias.
Patients’ Demographics and Clinical Characteristics
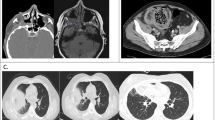
The mean age of the patients was 51±11years. The other demographic data and clinical characteristics of the included patients are shown in Table 1. CAM was more common amongst males than females, with a male/female ratio of 2.87. The most prevalent comorbidity in CAM patients was diabetes 646/821(78.7%), and 85 of these cases (13.2%) had new-onset diabetes. The median time of the interval between COVID-19 and evolution of mucormycosis symptoms and signs was about 15 days (range 0–50 days). The use of the immunosuppressive drug (tocilizumab) in addition to glucocorticoids was present in 17/792 patients (2.1%).
Quantitative Synthesis of Mortality-Related Risk Factors in CAM Patients
The meta-analysis of the studies showed that the overall mortality rate in patients with CAM was 28% (95% CI 20%–38%; I2 =82.28%; p for Cochran Q<0.001) (Fig. 2). The number of patients, mortality rate and ES, overall and each subgroup heterogeneity, and significance of differences in mortality rate between each subgroup are shown in Table 2. Our results showed that overall statistical heterogeneity for all variables is more than 50%, although some subgroups had statistical heterogeneity of less than 50%. Taking these findings into account, the heterogeneity of the existing data about patients with CAM who were included in our study is high. As shown in Table 2, there were no statistically significant differences between the ES of the mortality rate of subgroups considering age, sex, history of diabetes, history of DKA or poor glycemic control, or history of steroid administration for COVID-19. However, significant differences were observed between the ES of the mortality rate in patients with CAM regarding history of comorbidities other than diabetes (75%; 95%CI 52%–93%; I2=11.01%; p for Cochran Q=0.34 in the positive subgroup), pvalue;<0.001; the severity of COVID-19 infection (52%; 95%CI 29%-74%; I2=71.40%; p for Cochran Q<0.001 in the severe subgroup), pvalue=0.01; history of mechanical ventilation due to COVID-19(94%; 95%CI 76%–100%; I2= 30.86%; p for Cochran Q=0.16 in the positive subgroup), pvalue<0.001; the interval between COVID-19 and mucormycosis (64%; 95%CI 47%–80%; I2=2.99%; p for Cochran Q=0.42 in the early CAM subgroup), pvalue<0.001; clinical syndrome types of mucormycosis (67%;95%CI 40%–90%; I2 =66.78%; p for Cochran Q=0 and 71%; 95%CI 22%-100%; I2=0; p for Cochran Q=0.52 in the ROCM and pulmonary subgroups, respectively), pvalue<0.001; and treatment regimen of mucormycosis (91%;95%CI 63%–100%;I2= 3.02%; p for Cochran Q=0.41 in the only medical treatment subgroup), pvalue<0.001. The patients with a positive history of mechanical ventilation, comorbidities other than diabetes, pulmonary mucormycosis and ROCM, and those who only received medical treatment for mucormycosis had the highest ES of mortality rate followed by early CAM and severe COVID-19 infection.
The CAM patients with comorbidities other than diabetes had significantly higher mortality rates in comparison with those with diabetes (75%; 95%CI 52%–93% versus (vs.) 24%; 95%CI 13%–37%) p value<0.001.
Our analysis showed that pulmonary mucormycosis and ROCM had a significantly higher mortality rate than ROM and sino-nasal subgroups. However, the difference between the ES of mortality of pulmonary and ROCM subgroups was not statistically significant (pvalue=0.77). Besides, we merged ROM, sino-nasal, and ROCM subgroups and considered them as a non-pulmonary subgroup. Pulmonary mucormycosis showed significantly higher mortality rate in comparison to non-pulmonary subgroup (71%; 95%CI 22%-100%; I2=0; p for Cochran Q=0.52 vs. 28%; 95%CI 17%–40%; I2=76.13%; p for Cochran Q<0.001) p value=0.038.
Discussion
In developing countries, diabetes mellitus is the most common underlying cause of mucormycosis[73]; however, in developed countries, hematologic malignancies and transplants play a major predisposing role [74]. Similarly, in our study, as the included articles are reported from India, Iran, Egypt, Mexico, and Turkey, the most prevalent risk factor for contracting mucormycosis is diabetes mellitus. The underlying disease determines the clinical presentation of mucormycosis (i.e., diabetes predisposes patients more to rhino-orbital mucormycosis, while patients with hematologic malignancies and transplants are more commonly present with pulmonary, disseminated, and gastrointestinal mucormycosis). Therefore, the most common clinical presentation of mucormycosis differs between developed and developing countries depending on the prevalence of the various comorbidities or risk factors. Pulmonary is the most frequent type of mucormycosis in western countries; however, in developing countries, rhino-orbital is the most prevalent type [74, 75]. In our study, similar to the previous reports [73, 75], ROM is the most common type of mucormycosis, followed by ROCM, sinonasal/oronasal, and pulmonary.
To the best of our knowledge, few systematic reviews concerning the mortality rate of patients with CAM and identifying its related risk factors have been reported in the literature so far [47, 62, 76]. In our review, the overall mortality rate of CAM is 28%, which varies from 28% to 71%, considering the clinical syndrome types of mucormycosis. As all of the included studies are reported from developing countries, the overall mortality rate in our study is similar to the mortality rate of non-pulmonary (ROM, sino-nasal, and ROCM) mucormycosis. Our results are similar to the prior report of the case fatality rate of mucormycosis without COVID-19 [2]. Similarly, Patel et al. [46] showed no significant differences between the 6-week and 12-week mortality rates of patients with CAM and non-CAM. However, subgroup analysis of the ES of the mortality rate in our study regarding the time interval between COVID-19 and mucormycosis demonstrated that early vs. late CAM had statistically different mortality rates (64%vs.26%). Further studies are warranted to clarify the exact correlation between mortality rates of CAM patients and the time interval between COVID-19 and mucormycosis. The patients with comorbidities other than diabetes, history of mechanical ventilation, ROCM and pulmonary mucormycosis, and those who only received medical treatment for mucormycosis had the highest mortality rate in our review. However, age, sex, and history of diabetes had no significant effect on mortality rate, similar to Pal et al. [76] suggestions.
The ES of mortality rate in patients with comorbidities other than diabetes, including hematological malignancies, other types of malignancies, kidney disease, chronic liver disease, renal transplant, asthma and chronic obstructive pulmonary disease(COPD), neutropenia, human immunodeficiency virus (HIV), or tuberculosis is significantly higher than those with diabetes (75% vs. 24%). Similarly, Turner et al. [77] showed that the mortality rate of patients with diabetes and mucormycosis was lower than those with other comorbidities. One possible reason for this finding is that, as earlier mentioned, pulmonary, disseminated, and gastrointestinal mucormycosis with a worse prognosis than rhino-orbital are more prevalent in the presence of malignancies, transplantation, or neutropenia.
Severely-ill COVID-19 patients are at a higher risk of developing secondary fungal infections, including aspergillosis, candidiasis, cryptococcosis, mucormycosis, and a greater fatality rate than non-severe cases, through more severe alterations in the immune responses [78,79,80,81], consistent with our findings. In contrast, Pal et al. [76] suggested that COVID-19 severity had no prognostic effect on the mortality rate. They included only 51 patients in their analysis of the effect of severity of COVID-19 on the mortality of CAM patients. Surprisingly, the number of patients with CAM in the mild–moderate group was more than those in the severe-critical group (38 vs.13), and the mortality rate in the earlier group was higher than the latter (50% vs.31%) in their study. However, this difference was not statistically significant. The small sample size might affect the findings of Pal et al.; consequently, further studies with a higher sample size are necessary to substantiate the exact effect of severity of COVID-19 on the mortality of CAM patients. The history of mechanical ventilation due to COVID-19 had the worst prognostic effect, and most of the patients with a history of mechanical ventilation died, similar to the previous report [82]. It could be explained by the fact that mechanically ventilated individuals are more acutely ill. Besides, delay in the diagnosis and/or surgical debridement due to the poor general medical condition might contribute to the higher mortality rates in mechanically ventilated individuals. Therefore, in mechanically ventilated patients, meticulous and regular examination and screening for the presence of signs/symptoms related to mucormycosis and performing surgical debridement if indicated, at an appropriate time, are mandatory to reduce the mortality in these patients.
Similar to our findings, Hoenigl et al. [83] suggested that pulmonary mucormycosis had a significantly higher mortality rate than rhino-orbital mucormycosis; however, the difference between pulmonary and ROCM was not statistically significant. In contrast, Riad et al. [62] showed that patients with pulmonary mucormycosis had a significantly higher mortality rate than those with cerebral involvement. The small sample size of ROCM (22 patients) might affect the findings of Riad et al. It seems that mucormycosis with cerebral involvement, pulmonary, gastrointestinal, and disseminated renders the worst prognosis; however, cutaneous and sino-nasal are associated with the most favorable outcome [84]. Besides, in our review, the differences between the ES of the mortality rate of pulmonary and non-pulmonary mucormycosis were statistically significant, consistent with Pal et al. [76] and Garg et al. [85] reports.
Our results showed that ROCM and delivering only medical treatment to the patients with CAM are associated with worse prognosis, which is consistent with Turner et al.’s [77] findings; therefore, a timely diagnosis and aggressive medical and surgical treatment in a sinus mucormycosis subtype is a crucial step for preventing from extension of infection to the cerebrum and reducing the mortality rate of these patients.
Limitations
The limitations of our study are as follows: 1- We performed this meta-analysis through a comprehensive systematic search; however, most of the existing studies about patients with CAM are case reports, case series, and cross-sectional without control subjects. Further high-quality cohort and case–control studies are warranted to accurately identify the mortality-related risk factors in CAM patients. 2- There was significant heterogeneity in the reporting data. To alleviate the effect of this heterogeneity on our results, we categorized each variable into subgroups and performed subgroup analysis. 3- A few included studies reported mortality rates as a whole and did not mention the exact mortality rates in each subgroup of the variables; consequently, we excluded these data from our meta-analysis.
Conclusion
This study is a meta-analysis concerning mortality-related risk factors in patients with CAM. The present study showed that history of comorbidities other than diabetes (malignancies, transplant, or renal failure), the severe COVID-19, history of mechanical ventilation, early CAM, pulmonary mucormycosis and ROCM, and delivering only medical treatment are the worst prognostic factors and are associated with a high mortality rate. Identifying the mortality-related risk factors in CAM patients may help reduce the mortality rate of patients with mucormycosis during the COVID-19 pandemic by implementing a more aggressive therapeutic approach when one or more of these predisposing factors are present.
References
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9.
Serris A, Danion F, Lanternier F. Disease entities in mucormycosis. J Fungi (Basel). 2019;5(1):23.
Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med. 2021;42:264. e5–8.
Mehta S, Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus. 2020;12(9):e10726.
Mekonnen ZK, Ashraf DC, Jankowski T, Grob SR, Vagefi MR, Kersten RC, et al. Acute invasive rhino-orbital mucormycosis in a patient with COVID-19-associated acute respiratory distress syndrome. Ophthalmic Plast Reconstr Surg. 2021;37(2):e40.
Sen M, Lahane S, Lahane TP, Parekh R, Honavar SG. Mucor in a viral land: a tale of two pathogens. Indian J Ophthalmol. 2021;69(2):244–52.
Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–7.
Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): case report and systematic review of literature. Mycopathologia. 2021;186(2):289–98.
Pasero D, Sanna S, Liperi C, Piredda D, Branca GP, Casadio L, et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection. 2021;49(5):1055–60.
Ahmadikia K, Hashemi SJ, Khodavaisy S, Getso MI, Alijani N, Badali H, et al. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: A case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 2021;64(8):798–808.
Alekseyev K, Didenko L, Chaudhry B. Rhinocerebral mucormycosis and COVID-19 pneumonia. J Med Cases. 2021;12(3):85–9.
Dallalzadeh LO, Ozzello DJ, Liu CY, Kikkawa DO, Korn BS. Secondary infection with rhino-orbital cerebral mucormycosis associated with COVID-19. Orbit. 2021;1–4. https://doi.org/10.1080/01676830.2021.1903044.
Kanwar A, Jordan A, Olewiler S, Wehberg K, Cortes M, Jackson BR. A fatal case of Rhizopus azygosporus pneumonia following COVID-19. J Fungi (Basel). 2021;7(3):174.
Karimi-Galougahi M, Arastou S, Haseli S. editors. Fulminant mucormycosis complicating coronavirus disease 2019 (COVID-19). Int Forum Allergy Rhinol. 2021;11(6):1029–30.
Maini A, Tomar G, Khanna D, KiniY MH, Bhagyasree V. Sino-orbital mucormycosis in a COVID-19 patient: A case report. Int J Surg Case Rep. 2021;82:105957.
Moorthy A, Gaikwad R, Krishna S, Hegde R, Tripathi K, Kale PG, et al. SARS-CoV-2, uncontrolled diabetes and corticosteroids-an unholy trinity in invasive fungal infections of the maxillofacial region? a retrospective, multi-centric analysis. J Maxillofac Oral Surg. 2021;20(3):418–25.
Revannavar SM, Supriya P, Samaga L, Vineeth V. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep. 2021;14(4):e241663.
Saldanha M, Reddy R, Vincent MJ. Title of the article: paranasal mucormycosis in COVID-19 patient. Indian J Otolaryngol Head Neck Surg. 2021;1–4. https://doi.org/10.1007/s12070-021-02574-0.
Sarkar S, Gokhale T, Choudhury SS, Deb AK. COVID-19 and orbital mucormycosis. Indian J Ophthalmol. 2021;69(4):1002–4.
Veisi A, Bagheri A, Eshaghi M, Rikhtehgar MH, Rezaei Kanavi M, Farjad R. Rhino-orbital mucormycosis during steroid therapy in COVID-19 patients: a case report. Eur J Ophthalmol. 2021;32(4):NP11–6 11206721211009450.
Verma DK, Bali RK. COVID-19 and mucormycosis of the craniofacial skeleton: Causal, contributory or coincidental? J Maxillofac Oral Surg. 2021;20(2):165–6.
Waizel-Haiat S, Guerrero-Paz JA, Sanchez-Hurtado L, Calleja-Alarcon S, Romero-Gutierrez L. A case of fatal rhino-orbital mucormycosis associated with new onset diabetic ketoacidosis and COVID-19. Cureus. 2021;13(2):e13163.
Zurl C, Hoenigl M, Schulz E, Hatzl S, Gorkiewicz G, Krause R, et al. Autopsy proven pulmonary mucormycosis due to Rhizopus microsporus in a critically ill COVID-19 patient with underlying hematological malignancy. J Fungi (Basel). 2021;7(2):88.
Placik DA, Taylor WL, Wnuk NM. Bronchopleural fistula development in the setting of novel therapies for acute respiratory distress syndrome in SARS-CoV-2 pneumonia. Radiol Case Rep. 2020;15(11):2378–81.
do Monte Junior ES, dos Santos MEL, Ribeiro IB, de Oliveira Luz G, Baba ER, Hirsch BS, et al. Rare and fatal gastrointestinal mucormycosis (Zygomycosis) in a COVID-19 patient: a case report. Clin Endosc. 2020;53(6):746–9.
Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe. 2020;1(6):e245–e53.
Garg R, Bharangar S, Gupta S, Bhardwaj S. Post Covid-19 infection presenting as rhino-orbital mycosis. Indian J Otolaryngol Head Neck Surg. 2021;1–8. https://doi.org/10.1007/s12070-021-02722-6.
Nasir N, Farooqi J, Mahmood SF, Jabeen K. COVID-19 associated mucormycosis: a life-threatening complication in patients admitted with severe to critical COVID-19 from Pakistan. Clin Microbiol Infect. 2021; 27(11):1704-1707. S1198-743X(21)00433-X.
Fernández-García O, Guerrero-Torres L, Roman-Montes CM, Rangel-Cordero A, Martínez-Gamboa A, Ponce-de-León A, et al. Isolation of Rhizopus microsporus and Lichtheimia corymbifera from tracheal aspirates of two immunocompetent critically ill patients with COVID-19. Med Mycol Case Rep. 2021;33:32–7.
Ostovan VR, Rezapanah S, Behzadi Z, Hosseini L, Jahangiri R, Anbardar MH, et al. Coronavirus disease (COVID-19) complicated by rhino-orbital-cerebral mucormycosis presenting with neurovascular thrombosis: a case report and review of literature. J Neuro-Oncol. 2021;27(4):644–9.
Jain M, Tyagi R, Tyagi R, Jain G. Post-COVID-19 gastrointestinal invasive mucormycosis. Indian J Surg. 2022;84(3):545–7.
Tabarsi P, Khalili N, Pourabdollah M, Sharifynia S, Naeini AS, Ghorbani J, et al. COVID-19 associated rhinosinusitis mucormycosis due to Rhizopus oryzae: A rare but potentially fatal infection occurring after treatment with corticosteroids. Am J Trop Med Hyg. 2021;105(2):449–53.
Eswaran S, Balan SK, Saravanam PK. Acute fulminant mucormycosis triggered by covid 19 infection in a young patient. Indian J Otolaryngol Head Neck Surg. 2021;1–5. https://doi.org/10.1007/s12070-021-02689-4.
Shakir M, Maan MHA, Waheed S. Mucormycosis in a patient with COVID-19 with uncontrolled diabetes. BMJ Case Rep. 2021;14(7):e245343.
Khatri A, Chang K-M, Berlinrut I, Wallach F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient–case report and review of literature. J Mycol Med. 2021;31(2):101125.
Arana C, Cuevas Ramírez RE, Xipell M, Casals J, Moreno A, Herrera S, et al. Mucormycosis associated with covid19 in two kidney transplant patients. Transpl Infect Dis. 2021;23(4):e13652.
Kaur H, Kanaujia R, Rudramurthy SM. Rhizopus homothallicus: An emerging pathogen in era of COVID-19 associated mucormycosis. Indian J Med Microbiol. 2021;S0255-0857(21):04137–2.
Rao R, Shetty AP, Nagesh CP. Orbital infarction syndrome secondary to rhino-orbital mucormycosis in a case of COVID-19: Clinico-radiological features. Indian J Ophthalmol. 2021;69(6):1627–30.
Sargin F, Akbulut M, Karaduman S, Sungurtekin H. Severe rhinocerebral mucormycosis case developed after COVID 19. J Bacteriol Parasitol. 2021;12(1):1000386.
Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15(4):102146.
Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620–9.
Gumashta J, Gumashta R. COVID19 associated mucormycosis: Is GRP78 a possible link? J Infect Public Health. 2021;14(10):1351–7.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2020;71(6):1367–76.
World Health Organization. Clinical management of COVID-19: interim guidance. Geneva: World Health Organization; 2020.
Patel A, Agarwal R, Rudramurthy SM, Shevkani M, Xess I, Sharma R, et al. Multicenter epidemiologic study of Coronavirus disease–associated mucormycosis, India. Emerg Infect Dis. 2021;27(9):2349–59.
Muthu V, Rudramurthy SM, Chakrabarti A, Agarwal R. Epidemiology and pathophysiology of COVID-19-associated mucormycosis: India Versus the Rest of the World. Mycopathologia. 2021;186(6):739–54.
Honavar SG. Code Mucor:Guidelines for the diagnosis, staging and management of rhino-orbito-cerebral mucormycosis in the setting of COVID-19. Indian J Ophthalmol. 2021;69(6):1361–5.
Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–33.
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Joanna Briggs Institute Reviewer’s Manual. Adelaide: The Joanna Briggs Institute; 2020.
Mishra Y, Prashar M, Sharma D, Kumar VP, Tilak T. Diabetes, COVID 19 and mucormycosis: Clinical spectrum and outcome in a tertiary care medical center in western India. Diabetes Metab Syndr. 2021;15(4):102196.
Kumari A, Rao NP, Patnaik U, Malik V, Tevatia MS, Thakur S, et al. Management outcomes of mucormycosis in COVID-19 patients: A preliminary report from a tertiary care hospital. Med J Armed Forces India. 2021;77:S289–S95.
Nair AG, Adulkar NG, D’Cunha L, Rao PR, Bradoo RA, Bapaye MM, et al. Rhino-orbital mucormycosis following COVID-19 in previously non-diabetic, immunocompetent patients. Orbit. 2021;40(6):499–504.
Pakdel F, Ahmadikia K, Salehi M, Tabari A, Jafari R, Mehrparvar G, et al. Mucormycosis in patients with COVID-19: A cross-sectional descriptive multicentre study fromIran. Mycoses. 2021;64(10):1238–52.
Bayram N, Ozsaygılı C, Sav H, Tekin Y, Gundogan M, Pangal E, et al. Susceptibility of severe COVID-19 patients to rhino-orbital mucormycosis fungal infection in different clinical manifestations. Jpn J Ophthalmol. 2021;65(4):515–25.
Joshi AR, Muthe MM, Patankar SH, Athawale A, Achhapalia Y. CT and MRI findings of invasive mucormycosis in the setting of COVID-19: experience from a single center in India. AJR AM J Roentgenol. 2021;217(6):1431–2.
Avatef Fazeli M, Rezaei L, Javadirad E, Iranfar K, Khosravi A, Amini Saman J, et al. Increased incidence of rhino-orbital mucormycosis in an educational therapeutic hospital during the COVID-19 pandemic in western Iran: An observational study. Mycoses. 2021. https://doi.org/10.1111/myc.13351.
Singh Y, Ganesh V, Kumar S, Patel N, Aggarwala R, Soni KD, et al. Coronavirus disease-associated mucormycosis from a tertiary care hospital in India: A case series. Cureus. 2021;13(7):e16152.
Arjun R, Felix V, Niyas V, Kumar M, Krishnan R, Mohan V, et al. COVID-19-associated rhino-orbital mucormycosis: a single-centre experience of 10 cases. QJM. 2021;114(11):831–4 hcab176.
Swain SK, Jena PP, Das S, Gupta A. COVID-19 associated mucormycosis in head and neck region: our experiences at a tertiary care teaching hospital of eastern India. Siriraj Med J. 2021;73(7):423–8.
Nehara HR, Puri I, Singhal V, Ih S, Bishnoi BR, Sirohi P. Rhinocerebral mucormycosis in COVID-19 patient with diabetes a deadly trio: Case series from the north-western part of India. Indian J Med Microbiol. 2021;39(3):380–3.
Riad A, Shabaan AA, Issa J, Ibrahim S, Amer H, Mansy Y, et al. COVID-19-associated mucormycosis (Cam): Case-series and global analysis of mortality risk factors. J Fungi(Basel). 2021;7(10):837.
Yadav S, Sharma A, Kothari N, Bhatia PK, Goyal S, Goyal A. Mucormycosis: A case series of patients admitted in non-covid-19 intensive care unit of a tertiary care center during the second wave. Indian J Crit Care Med. 2021;25(10):1191–4.
Pal P, Chatterjee N, Ghosh S, Ray BK, Mukhopadhyay P, Bhunia K, et al. Covid associated mucormycosis: A study on the spectrum of clinical, biochemical and radiological findings in a series of ten patients. J Assoc Physicians India. 2021;69(10):17–23.
Ashour MM, Abdelaziz TT, Ashour DM, Askoura A, Saleh MI, Mahmoud MS. Imaging spectrum of acute invasive fungal rhino-orbital-cerebral sinusitis in COVID-19 patients: A case series and a review of literature. (2021). J Neuroradiol. 2021;48(5):319–24.
Guzmán-Castro S, Chora-Hernandez LD, Trujillo-Alonso G, Calvo-Villalobos I, Sanchez-Rangel A, Ferrer-Alpuin E, et al. COVID-19-associated mucormycosis, diabetes and steroid therapy: Experience in a single centre in Western Mexico. Mycoses. 2021. https://doi.org/10.1111/myc.13383.
Sk S, Jena PP, Lenka S. COVID-19 associated mucormycosis in head and neck region of children during current pandemic: Our experiences. Pediatr Pol. 2021;96(3):162–7.
Gupta R, Kesavadev J, Krishnan G, Agarwal S, Saboo B, Shah M, et al. COVID-19 associated mucormycosis: A descriptive multisite study from India. Diabetes Metab Syndr. 2021;15(6):102322.
Bhanuprasad K, Manesh A, Devasagayam E, Varghese L, Cherian LM, Kurien R, et al. Risk factors associated with the mucormycosis epidemic during the COVID-19 pandemic. Int J Infect Dis. 2021;111:267–70.
Pradhan P, Shaikh Z, Mishra A, Preetam C, Parida PK, Sarkar S, et al. Predisposing factors of rhino-orbital-cerebral mucormycosis in patients with COVID 19 infection. Indian. J Otolaryngol Head Neck Surg. 2021:1–7.
Zirpe K, Pote P, Deshmukh A, Gurav SK, Tiwari AM, Suryawanshi P. A Retrospective Analysis of Risk Factors of COVID-19 Associated Mucormycosis and Mortality Predictors: A Single-Center Study. Cureus. 2021;13(10):e18718.
Muthu V, Kumar M, Paul RA, Zohmangaihi D, Choudhary H, Rudramurthy SM, et al. Is there an association between zinc and COVID-19-associated mucormycosis? Results of an experimental and clinical study. Mycoses. 2021;64(10):1291–7.
Patel A, Kaur H, Xess I, Michael J, Savio J, Rudramurthy S, et al. A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect. 2020;26(7):944. e9–e15.
Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, Lagrou K, et al. Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17(12):1859–67.
Bala K, Chander J, Handa U, Punia RS, Attri AK. A prospective study of mucormycosis in north India: experience from a tertiary care hospital. Med Mycol. 2015;53(3):248–57.
Pal R, Singh B, Bhadada SK, Banerjee M, Bhogal RS, Hage N, et al. COVID-19-associated mucormycosis: An updated systematic review of literature. Mycoses. 2021. https://doi.org/10.1111/myc.13338.
Turner JH, Soudry E, Nayak JV, Hwang PH. Survival outcomes inacute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope. 2013;123(5):1112–8.
Bhatt K, Agolli A, Patel MH, Garimella R, Devi M, Garcia E, et al. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discoveries (Craiova). 2021;9(1):e126.
Hocková B, Riad A, Valky J, Šulajová Z, Stebel A, Slávik R, et al. Oral complications of ICU patients with COVID-19: Case-Series and review of two hundred ten cases. J Clin Med. 2021;10(4):581.
Riad A, Gomaa E, Hockova B, Klugar M. Oral candidiasis of COVID-19 patients: Case report and review of evidence. J Cosmet Dermatol. 2021 Jun;20(6):1580–4.
Peng J, Wang Q, Mei H, Zheng H, Liang G, She X, et al. Fungal co-infection in COVID-19 patients: evidence from a systematic review and meta-analysis. Aging (Albany NY). 2021;13(6):7745–57.
Meawed TE, Ahmed SM, Mowafy SM, Samir GM, Anis RH. Bacterial and fungal ventilator associated pneumonia in critically ill COVID-19 patients during the second wave. J Infect Public Health. 2021;14(10):1375–80.
Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux JP, et al. The emergence of COVID-19 associated mucormycosis: analysis of cases from 18 countries. Lancet Microbe. 2022;3(7):e543–52.
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634–53.
Garg M, Prabhakar N, Muthu V, Farookh S, Kaur H, Suri V, et al. CT findings of COVID-19-associated pulmonary mucormycosis: A case series and literature review. Radiology. 2021;302(1):214–7. 211583. https://doi.org/10.1148/radiol.2021211583.
Author information
Authors and Affiliations
Contributions
VRO contributed to study conception, design, data extraction, analysis and interpretation, and writing the first draft and critique of the manuscript. RT contributed to study design, analysis, interpretation, and writing the first draft and critique of the manuscript. HB contributed to study conception, design, conducting the study searches, data extraction, and writing the first draft of the manuscript. ZB and SK contributed to study conception, design, data extraction and writing the first draft of the manuscript. HK contributed to study conception, design, conducting the study searches and writing the first draft of the manuscript. ABH, MM, and MG contributed to study conception, design and the review and critique of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on COVID-19 and Fungal Infections
Supplementary Information
ESM 1
(DOCX 55 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ostovan, V.R., Tabrizi, R., Bazrafshan, H. et al. Mortality-Related Risk Factors for Coronavirus Disease (COVID-19)-Associated Mucormycosis: a systematic review and meta-analysis. Curr Fungal Infect Rep 16, 143–153 (2022). https://doi.org/10.1007/s12281-022-00440-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-022-00440-2