Abstract
Purpose of Review
Globally, a change has been noticed in the epidemiology of fungal infections in the intensive care units (ICUs). The current review provides an insight into the current epidemiology of emerging fungal infections with special reference to their prevalence, spectrum of pathogen, outbreaks, and emergence of antifungal resistance reported from different ICUs of the world.
Recent Findings
The ICUs across the world are witnessing multiple changes in the epidemiology of fungal infections including change in prevalence and spectrum of etiological agents, new susceptible risk groups, geographical variations, emergence of novel multi-drug resistant Candida auris, outbreak due to rare fungal species, emergence of antifungal resistance, etc. An understanding of the contemporary local epidemiology of fungal agents in ICU is essential for optimal patient management.
Summary
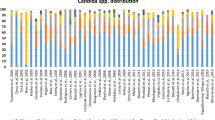
Invasive candidiasis and invasive aspergillosis continue to haunt as major pathogens in the ICU, and several new risk factors associated with these infections have surfaced up. There is a contrasting picture for the species distribution of Candida among the different countries of the world. C. auris, the yeast behaving like bacteria, has emerged as a potential threat to ICUs across the five continents. Other mycelial agents like Mucorales, Paecilomyces spp., Fusarium spp., and Cladosporium spp., although encountered infrequently, continue to be reported as serious infections in ICU. The ICUs are also vulnerable sites for fungal infection outbreaks due to several fungi including rare ones like Cryptococcus spp., Pichia anomala, and Kodamaea ohmeri.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bajwa S, Kulshrestha A. Fungal infections in intensive care unit: challenges in diagnosis and management. Ann Med Health Sci Res [Internet]. 2013;3(2):238 Available from: http://www.amhsr.org/text.asp?2013/3/2/238/113669. Accessed 9 Nov 2018.
Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A, et al. An official American Thoracic Society statement: treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011;183(1):96–128.
Blot S, Cankurtaran M, Petrovic M, Vandijck D, Lizy C, Decruyenaere J, et al. Epidemiology and outcome of nosocomial bloodstream infection in elderly critically ill patients: a comparison between middle-aged, old, and very old patients. Crit Care Med. 2009;37(5):1634–41.
Blot S, Charles P. Fungal sepsis in the ICU: are we doing better? Trends in incidence, diagnosis, and outcome. Minerva Anestesiol. 2013;79(12):1396–405.
Vincent J, Marshall J, Anzueto A, Martin CD, Gomersall C. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323–9.
Hankovszky P, Társy D, Öveges N, Molnár Z. Invasive Candida infections in the ICU: diagnosis and therapy. J Crit Care Med [Internet]. 2015;1(4):129–39 Available from:http://content.sciendo.com/view/journals/jccm/1/4/article-p129.xml. Accessed 9 Nov 2018.
Blot S, Vandewoude K. Management of invasive Candidiasis in the critically ill patients. Drugs [Internet]. 2004;64(19):2159–75 Available from:http://link.springer.com/10.1007/978-3-642-25716-2.
Meersseman W. Invasive aspergillosis in the intensive care unit. Ann N Y Acad Sci. 2012;1272:31–9. Accessed 9 Nov 2018.
Azoulay E, Timsit JF, Tafflet M, De Lassence A, Darmon M, Zahar JR, et al. Candida colonization of the respiratory tract and subsequent Pseudomonas ventilator-associated pneumonia. Chest. 2006;129(1):110–7.
Prowle JR, Echeverri JE, Ligabo EV, Sherry N, Taori GC, Crozier TM, et al. Acquired bloodstream infection in the intensive care unit: incidence and attributable mortality. Crit Care. 2011;15(2):R100.
Quenot JP, Binquet C, Kara F, Martinet O, Ganster F, Navellou JC, et al. The epidemiology of septic shock in French intensive care units: the prospective multicenter cohort EPISS study. Crit Care. 2013;17(2):R65.
Fagan RP, Edwards JR, Park BJ, Fridkin SK, Magill SS. Incidence trends in pathogen-specific central line-associated bloodstream infections in US intensive care units, 1990–2010. Infect Control Hosp Epidemiol [Internet]. 2013;34(09):893–9 Available from:https://www.cambridge.org/core/product/identifier/S0195941700033683/type/journal_article.
Lagrou K, Maertens J, Van Even E, Denning DW. Burden of serious fungal infections in Belgium. Mycoses. 2015;58(Suppl S5):1–5.
Taj-Aldeen SJ, Chandra P, Denning DW. Burden of fungal infections in Qatar. Mycoses. 2015;58:51–7.
Rodriguez-Tudela J, Alastruey-Izquierdo A, Gago S, Cuenca-Estrella M, Leon C, Miro J, et al. Burden of serious fungal infections in Spain. Clin Microbiol Infect. 2015;21(2):183–9.
Arsenijevic V, Denning DW. Estimated burden of serious human fungal diseases in Serbia. J Fungi. 2018;4(76):1–13.
Gugnani HC, Denning DW. Burden of serious fungal infections in the Dominican Republic. J Infect Public Health [Internet]. 2016;9(1):7–12. Available from:. https://doi.org/10.1016/j.jiph.2015.04.026.
Osmanov A, Denning DW. Burden of serious fungal infections in Ukraine. Mycoses. 2015;58(Suppl. S5):94–100.
Mortensen KL, Denning DW, Arendrup MC. The burden of fungal disease in Denmark. Mycoses. 2015;58:15–21.
Ruhnke M, Groll AH, Mayser P, Ullman AJ, Mendling WM, Hof H, et al. Estimated burden of fungal infections in Germany. Mycoses. 2015;58(Suppl S5):22–8.
Sinkó J, Sulyok M, Denning DW. Burden of serious fungal diseases in Hungary. Mycoses. 2015;58:29–33.
Beardsley J, Denning DW, Chau N, Yen N, Crump J, Day J. Estimating the burden of fungal diseases in Vietnam. Mycoses. 2015;58(Suppl. S5):101–6.
Riera F, Caeiro J, Denning DW. Burden of serious fungal infections in Argentina. J Fungi. 2018;4(51):1–11.
Denning DW, Gugnani HC. Burden of serious fungal infections in Trinidad and Tobago. Mycoses. 2015;58:80–4.
Chrdle A, Mallatova N, Vasakova M, Haber J, Denning DW. Burden of serious fungal infections in the Czech Republic. Mycoses. 2015;58(Suppl. S5):6–14.
Velayuthan R, Samudi C, Lakhbeer Singh H, Ng K, Shankar E, Denning D. Estimation of the burden of serious human fungal infections in Malaysia. J Fungi [Internet]. 2018;4(1):38 Available from: http://www.mdpi.com/2309-608X/4/1/38 Accessed 9 Nov 2018.
Gugnani H, Denning DW. Estimated burden of serious fungal infections in Jamaica by literature review and modelling. West Indian Med J. 2015;64(3):245–9. Accessed 9 Nov 2018.
Wadi J, Denning DW. Burden of serious fungal infections in Jordan. J Fungi. 2018;4(15):1–12.
Gangneux JP, Bougnoux ME, Hennequin C, Godet C, Chandenier J, Denning DW, et al. Estimation du poids épidémiologique des infections fongiques graves en France. J Mycol Med [Internet]. 2016;26(4):385–90. Available from:. https://doi.org/10.1016/j.mycmed.2016.11.001.
Tortorano AM, Dho G, Prigitano A, Breda G, Grancini A, Emmi V, et al. Invasive fungal infections in the intensive care unit: a multicentre, prospective, observational study in Italy (2006–2008). Mycoses. 2012;55(1):73–9.
• Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M, et al. Incidence, characteristics and outcome of ICU-acquired candidemia in India. Intensive Care Med. 2015;48(2):285–95 A first-of-its-kind systematic epidemiological study highlighting the wide variety of Candida spp. and their antifungal susceptibilities among Indian ICUs. Accessed 9 Nov 2018.
Alangaden GJ. Nosocomial fungal infections: epidemiology, infection control, and prevention. Infect Dis Clin North Am [Internet]. 2011;25(1):201–25. Available from:. https://doi.org/10.1016/j.idc.2010.11.003.
Montagna MT, Caggiano G, Lovero G, De Giglio O, Coretti C, Cuna T, et al. Epidemiology of invasive fungal infections in the intensive care unit: results of a multicenter Italian survey (AURORA Project). Infection. 2013;41(3):645–53.
Taccone FS, Van den Abeele AM, Bulpa P, Misset B, Meersseman W, Cardoso T, et al. Epidemiology of invasive aspergillosis in critically ill patients: clinical presentation, underlying conditions, and outcomes. Crit Care. 2015;19(1):1–15.
Baddley JW, Stephens JM, Ji X, Gao X, Schlamm HT, Tarallo M. Aspergillosis in Intensive Care Unit (ICU) patients: epidemiology and economic outcomes. BMC Infect Dis [Internet]. 2013;13(29):1–8 Available from: BMC Infectious Diseases.
Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerdert E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med. 2004;170(6):621–5.
Silfvast T, Takkunen O, Kolho E, Andersson LC, Rosenberg P. Characteristics of discrepancies between clinical and autopsy diagnoses in the intensive care unit: a 5-year review. Intensive Care Med. 2003;29(2):321–4. Accessed 9 Nov 2018.
Vallés J, Mesalles E, Mariscal D, Del Mar Fernández M, Peña R, Jiménez JL, et al. A 7-year study of severe hospital-acquired pneumonia requiring ICU admission. Intensive Care Med. 2003;29(11):1981–8.
• Bassetti M, Bouza E. Invasive mould infections in the ICU setting: complexities and solutions. J Antimicrob Chemother. 2017;72(January):i39–47. Elaborate review on mold infections with special reference to newer risk groups identified among ICU patients.
Poirier P, Nourrisson C, Gibold L, Chalus E, Guelon D, Descamp S, et al. Three cases of cutaneous mucormycosis with Lichtheimia spp. (ex Absidia/Mycocladus) in ICU. Possible cross-transmission in an intensive care unit between 2 cases. J Mycol Med [Internet]. 2013;23(4):265–9. Available from:. https://doi.org/10.1016/j.mycmed.2013.09.002.
Sipsas N, Kontoyiannis D. Invasive fungal infections in patients with cancer in the intensive care unit. Int J Antimicrob Agents. 2012;39(6):464–79.
Machicado JD, Younes M, Wolf DS. A rare cause of gastrointestinal bleeding in the intensive care unit. Gastroenterol Int. 2014;146(4):911,1136–7. Available from:. https://doi.org/10.1053/j.gastro.2013.11.038.
Gonçalves CL, Mota FV, Ferreira GF, Mendes JF, Pereira EC, Freitas CH, et al. Airborne fungi in an intensive care unit. Brazilian J Biol [Internet]. 2017;6984(0):265–70 Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1519-69842017005109104&lng=en&tlng=en.
Rudramurthy S, Singh G, Hallur V, Verma S, Chakrabarti A. High fungal spore burden with predominance of Aspergillus in hospital air of a tertiary care hospital in Chandigarh. Indian J Med Microbiol. 2016;34(4):529–32.
Chapman B, Slavin M, Marriott D, Halliday C, Kidd S, Arthur I, et al. Changing epidemiology of candidaemia in Australia. J Antimicrob Chemother. 2017;72(4):1103–8.
Colombo AL, Garnica M, Aranha Camargo LF, Da Cunha CA, Bandeira AC, Borghi D, et al. Candida glabrata: an emerging pathogen in Brazilian tertiary care hospitals. Med Mycol. 2013;51(1):38–44.
Goemaere B, Becker P, Van Wijngaerden E, Maertens J, Spriet I, Hendrickx M, et al. Increasing candidaemia incidence from 2004 to 2015 with a shift in epidemiology in patients preexposed to antifungals. Mycoses. 2018;61(2):127–33.
Lin S, Chen R, Zhu S, Wang H, Wang L, Zou J, et al. Candidemia in adults at a tertiary hospital in China: clinical characteristics, species distribution, resistance, and outcomes. Mycopathologia [Internet]. 2018;183(4):679–89. Available from:. https://doi.org/10.1007/s11046-018-0258-5.
Kreusch A, Karstaedt AS. Candidemia among adults in Soweto, South Africa, 1990–2007. Int J Infect Dis [Internet]. 2013;17(8):e621–3. Available from:. https://doi.org/10.1016/j.ijid.2013.02.010.
Pfaller MA, Diekema DJ, Rinaldi MG, Barnes R, Hu B, Veselov AV, et al. Results from the ARTEMIS DISK Global Antifungal Surveillance Study: a 6.5-year analysis of susceptibilities of Candida and other yeast species to fluconazole and voriconazole by standardized disk diffusion testing results from the ARTEMIS DISK Global Antifungal Surveillance Group. J Clin Microbiol. 2005;43(12):5848–59.
Davis SL, Vazquez JA, McKinnon PS. Epidemiology, risk factors, and outcomes of Candida albicans versus non-albicans candidemia in nonneutropenic patients. Ann Pharmacother. 2007;41(4):568–73.
Motoa G, Muñoz JS, Oñate J, Pallares CJ, Hernández C, Villegas MV. Epidemiología de aislamientos de Candida en unidades de cuidados intensivos en Colombia durante el período 2010–2013. Rev Iberoam Micol. 2017;34(1):17–22.
Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53(1):41–4.
Montagna MT, Lovero G, Borghi E, Amato G, Andreoni S, Campion L, et al. Candidemia in intensive care unit: a nationwide prospective observational survey (GISIA-3 study) and review of the European literature from 2000 through 2013. Eur Rev Med Pharmacol Sci. 2014;18(5):661–74. Accessed 9 Nov 2018.
Falagas ME, Roussos N, Vardakas KZ. Relative frequency of albicans and the various non-albicans Candida spp among candidemia isolates from inpatients in various parts of the world: a systematic review. Int J Infect Dis [Internet]. 2010;14(11):e954–66. Available from:. https://doi.org/10.1016/j.ijid.2010.04.006.
Meersseman W. Invasive aspergillosis in the intensive care unit. Hum Fungal Pathog 2nd Ed. 2014;12:179–89.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases form a prospective mnationwide surveillance study. Clin Infect Dis [Internet]. 2004;39(3):309–17 Available from: https://academic.oup.com/cid/article-lookup/doi/10.1086/421946.http://cid.oxfordjournals.org/content/39/3/309.long Accessed 9 Nov 2018.
Janssen J, van Schijndel RS, Clement E, Ossenkoppele G, Thijs L, Huijgens P. Outcome of ICU treatment in invasive aspergillosis. Intensive Care Med. 1996;22(12):1315–22.
Garnacho-montero J, Olaechea P, Alvarez-lerma F, Alvarez-rocha L, Galván B, Rodriguez A, et al. Epidemiology of fungal respiratory infections in the critically ill patient. Rev Esp Quim. 2013;17426(2):173–88.
Vandewoude KH, Blot SI, Benoit D, Colardyn F, Vogelaers D. Invasive aspergillosis in critically ill patients: attributable mortality and excesses in length of ICU stay and ventilator dependence. J Hosp Infect. 2004;56(4):269–76.
Blot SI, Taccone FS, Van Den Abeele AM, Bulpa P, Meersseman W, Brusselaers N, et al. A clinical algorithm to diagnose invasive pulmonary Aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2012;186(1):56–64.
Trof RJ, Beishuizen A, Debets-Ossenkopp YJ, Girbes ARJ, Groeneveld ABJ. Management of invasive pulmonary aspergillosis in non-neutropenic critically ill patients. Intensive Care Med. 2007;33(10):1694–703.
• Forsberg K, Woodworth K, Walters M, Berkow EL, Jackson B, Chiller T, et al. Candida auris: the recent emergence of a multidrug-resistant fungal pathogen. Med Mycol [Internet]. 2018;57(August):1–12 Available from: https://academic.oup.com/mmy/advance-article/doi/10.1093/mmy/myy054/5062854. An excellent review of published literature on Candida auris with special reference to its epidemiology and rapid emergence across the globe.
• Rudramurthy SM, Chakrabarti A, Paul RA, Sood P, Kaur H, Capoor MR, et al. Candida auris candidaemia in Indian ICUs: analysis of risk factors. J Antimicrob Chemother. 2017;72(6):1794–801. A one-to-one comparison of Candida auris with other Candida spp. with respect to risk factors of the ICU patients.
Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, et al. Simultaneous emergence of multidrug-resistant candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017;64(2):134–40.
Schelenz S, Hagen F, Rhodes JL, Abdolrasouli A, Chowdhary A, Hall A, et al. First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob Resist Infect Control [Internet]. 2016;5(1):1–7. Available from:. https://doi.org/10.1186/s13756-016-0132-5.
Biswal M, Rudramurthy SM, Jain N, Shamanth AS, Sharma D, Jain K, et al. Controlling a possible outbreak of Candida auris infection: lessons learnt from multiple interventions. J Hosp Infect [Internet]. 2017;97(4):363–70. Available from:. https://doi.org/10.1016/j.jhin.2017.09.009.
Lipke AB, Mihas AA. Non-decompensated cirrhosis as a risk factor for invasive aspergillosis: a case report and review of the immune dysfunction of cirrhosis. Am J Med Sci [Internet]. 2007;334(4):314–6. Available from:. https://doi.org/10.1097/MAJ.0b013e318068d79c.
Glöckner A, Karthaus M. Current aspects of invasive candidiasis and aspergillosis in adult intensive care patients. Mycoses. 2011;54(5):420–33.
Shorr AF, Lazarus DR, Sherner JH, Jackson WL, Morrel M, Fraser VJ, et al. Do clinical features allow for accurate prediction of fungal pathogenesis in bloodstream infections? Potential implications of the increasing prevalence of non-albicans candidemia. Crit Care Med. 2007;35(4):1077–83.
Trofa D, Gacser A, Nosanchuk J. Candida parapsilosis: an emerging fungal pathogen. Clin Microbiol Rev. 2008;21:606–25.
Magill SS, Swoboda SM, Shields CE, Colantuoni EA, Fothergill AW, Merz WG, et al. The epidemiology of candida colonization and invasive candidiasis in a surgical intensive care unit where fluconazole prophylaxis is utilized: follow-up to a randomized clinical trial. Ann Surg. 2009;249(4):657–65.
Dimopoulos G, Piagnerelli M, Berré J, Salmon I, Vincent JL. Post mortem examination in the intensive care unit: still useful? Intensive Care Med. 2004;30(11):2080–5.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, et al. Defining Opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis [Internet]. 2002;34(1):7–14 Available from: https://academic.oup.com/cid/article-lookup/doi/10.1086/323335.
Garnacho-Montero J, Amaya-Villar R. A validated clinical approach for the management of aspergillosis in critically ill patients: ready, steady, go! Crit Care. 2006;10(2):2–3.
Hartemink KJ, Paul MA, Spijkstra JJ, Girbes ARJ, Polderman KH. Immunoparalysis as a cause for invasive aspergillosis? Intensive Care Med. 2003;29(11):2068–71.
Samarakoon P, Soubani A. Invasive pulmonary aspergillosis in patients with COPD: a report of five cases and systematic review of the literature P. Chronic Resp Dis [Internet]. 2008;5(2):19–27 Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=2247706.
Prodanovic H, Cracco C, Massard J, Barrault C, Thabut D, Duguet A, et al. Invasive pulmonary aspergillosis in patients with decompensated cirrhosis: case series. BMC Gastroenterol. 2007;7:1–4.
Peláez T, Muñoz P, Guinea J, Valerio M, Giannella M, Klaassen CHW, et al. Outbreak of invasive aspergillosis after major heart surgery caused by spores in the air of the intensive care unit. Clin Infect Dis. 2012;54(3):24–31.
Chakrabarti A, Singh K, Narang A, Singhi S, Batra R, Rao KLN, et al. Outbreak of Pichia anomala infection in the pediatric service of a tertiary-care center in Northern India. J Clin Microbiol. 2001;39(5):1702–6.
Chakrabarti A, Rudramurthy SM, Kale P, Hariprasath P, Dhaliwal M, Singhi S, et al. Epidemiological study of a large cluster of fungaemia cases due to Kodamaea ohmeri in an Indian tertiary care centre. Clin Microbiol Infect. 2014;20(2):83–9.
Chowdhary A, Becker K, Fegeler W, Gugnani H, Kapoor L, Randhawa V, et al. An outbreak of candidemia due to Candida tropicalis in a neonatal intensive care unit. Mycoses. 2003;46(8):287–92.
Vallabhaneni S, Haselow D, Lloyd S, Lockhart S, Moulton-meissner H, Lester L, et al. Cluster of Cryptococcus neoformans infections in intensive care unit, Arkansas, USA, 2013. Emerg Infect Dis. 2015;21(10):1719–24.
Torres-Narbona M, Guinea J, Martínez-Alarcón J, Muñoz P, Gadea I, Bouza E. Impact of zygomycosis on microbiology workload: a survey study in Spain. J Clin Microbiol. 2007;45(6):2051–3.
Schaffer K, FitzGerald S, Commane M, Maguiness A, Fenelon L. A pseudo-outbreak of Fusarium solani in an intensive care unit associated with bronchoscopy. J Hosp Infect. 2008;69(4):398–400.
Singh N, Belen O, Léger MM, Campos JM. Cluster of trichosporon mucoides in children associated with a faulty bronchoscope. Pediatr Infect Dis J. 2003;22(7):609–12.
Jackson L, Klotz SA, Normand RE. A pseudoepidemic of sporothrix cyanescens pneumonia occurring during renovation of a bronchoscopy suite. Med Mycol. 1990;28(6):455–9.
Hrabovský V, Takáčová V, Schréterová E, Pastvová L, Hrabovská Z, Čurová K, et al. Distribution and antifungal susceptibility of yeasts isolates from intensive care unit patients. Folia Microbiol (Praha). 2017;62(6):525–30.
Alimehr S, Shekari Ebrahim Abad H, Fallah F, Rahbar M, Mohammadzadeh M, Vossoghian S, et al. Candida infection in the intensive care unit: a study of antifungal susceptibility pattern of Candida species in Milad hospital, Tehran, Iran. J Mycol Med [Internet]. 2015;25(4):e113–7. Available from:. https://doi.org/10.1016/j.mycmed.2015.09.005.
Sasso M, Roger C, Sasso M, Poujol H, Barbar S, Lefrant JY, et al. Changes in the distribution of colonising and infecting Candida spp. isolates, antifungal drug consumption and susceptibility in a French intensive care unit: a 10-year study. Mycoses. 2017;60(12):770–80.
Pfaller MA, Messer SA, Moet GJ, Jones RN, Castanheira M. Candida bloodstream infections: comparison of species distribution and resistance to echinocandin and azole antifungal agents in Intensive Care Unit (ICU) and non-ICU settings in the SENTRY Antimicrobial Surveillance Program (2008–2009). Int J Antimicrob Agents [Internet]. 2011;38(1):65–9. Available from:. https://doi.org/10.1016/j.ijantimicag.2011.02.016.
Doi AM, Pignatari ACC, Edmond MB, Marra AR, Camargo LFA, Siqueira RA, et al. Epidemiology and microbiologic characterization of nosocomial Candidemia from a Brazilian National Surveillance Program. PLoS One. 2016;11(1):e0146909. Accessed 9 Nov 2018.
• Mencarini J, Mantengoli E, Tofani L, Riccobono E, Fornaini R, Bartalesi F, et al. Evaluation of candidemia and antifungal consumption in a large tertiary care Italian hospital over a 12-year period. Infection [Internet]. 2018;46(4):469–76. https://doi.org/10.1007/s15010-018-1139-z Available from: A compilation of Candida species distribution and their susceptibilities in Italian ICUs over a decade.
Liu W, Tan J, Sun J, Xu Z, Li M, Yang Q, et al. Invasive candidiasis in intensive care units in China: in vitro antifungal susceptibility in the China-SCAN study. J Antimicrob Chemother. 2014;69(1):162–7.
Eyre DW, Sheppard AE, Madder H, Moir I, Moroney R, Quan TP, et al. A Candida auris outbreak and its control in an intensive care setting. N Engl J Med [Internet]. 2018;379(14):1322–31 Available from: http://www.nejm.org/doi/10.1056/NEJMoa1714373.
Fuhren J, Voskuil WS, Boel CHE, Haas PJA, Hagen F, Meis JF, et al. High prevalence of azole resistance in Aspergillus fumigatus isolates from high-risk patients. J Antimicrob Chemother. 2015;70(10):2894–8.
van der Linden JWM, Arendrup MC, Warris A, Lagrou K, Pelloux H, Hauser PM, et al. Prospective multicenter international surveillance of azole resistance in Aspergillus fumigatus. Emerg Infect Dis. 2015;21(6):1041–4.
Van Paassen J, Russcher A, Int’ Veld-Van Wingerden AW, Verweij PE, Kuijper EJ. Emerging aspergillosis by azole-resistant Aspergillus fumigatus at an intensive care unit in the Netherlands, 2010 to 2013. Eur Secur. 2016;21(30):1–9.
Archimedes D, Carolina A, Souza R, Colombo AL. Revisiting species distribution and antifungal susceptibility of Candida bloodstream isolates from Latin American medical centers. J Fungi [Internet]. 2017;3(4):24 Available from:http://www.mdpi.com/2309-608X/3/2/24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Clinical Pathology
Rights and permissions
About this article
Cite this article
Chakrabarti, A., Sharma, M. Epidemiology of Emerging Fungal Infections in ICU. Curr Fungal Infect Rep 13, 1–10 (2019). https://doi.org/10.1007/s12281-019-0334-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-0334-4