Abstract
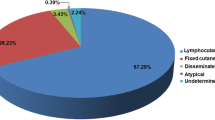
Sporotrichosis, a disease caused by the saprophytic, dimorphic fungus Sporothrix schenckii, is currently diagnosed worldwide, especially in some tropical and subtropical areas. The infection usually occurs after traumatic inoculation of soil, plants, and organic matter containing the fungus. Certain activities, such as floriculture, agriculture, mining, and wood exploitation, and zoonotic transmission are associated with the mycosis. In humans, the disease is limited to skin, subcutaneous tissue, and the proximal lymphatic. It occurs commonly as lymphocutaneous or fixed lesions predominantly affect the upper limbs and face, the latter location is frequent in children. However, sporotrichosis in children is uncommonly seen. Data about the disease on this specific group of patients is scanty. The gold standard for diagnosis is culture. Nevertheless, there are other recently added methods (serological, histopathological, and molecular) useful for an accurate diagnosis. Itraconazole is the first choice of treatment for sporotrichosis; however, potassium iodide is also an effective option, mainly in children.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mahajan VK. Sporotrichosis: an overview and therapeutic options. Dermatol Res Pract. 2014;2014, 272376. This review paper gives an overview of the disease.
McGuinness SL, Boyd R, Kidd S, McLeod C, Krause VL, Ralph AP. Epidemiological investigation of an outbreak of cutaneous sporotrichosis, Northern Territory. Australia BMC Infect Dis. 2016;16(1):16.
Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53(1):3–14. This paper shows a clear distribution of the disease worldwide.
Marimon R, Gené J, Cano J, Trilles L, Dos Santos LM, Guarro J. Molecular phylogeny of Sporothrix schenckii. J Clin Microbiol. 2006;44(9):3251–6.
Sanchotene KO, Madrid IM, Klafke GB, Bergamashi M, Della Terra PP, Rodrigues AM, et al. Sporothrix brasiliensis outbreaks and the rapid emergence of feline sporotrichosis. Mycoses. 2015;58(11):652–8.
Gremião ID, Menezes RC, Schubach TM, Figueiredo AB, Cavalcanti MC, Pereira SA. Feline sporotrichosis: epidemiological and clinical aspects. Med Mycol. 2015;53(1):15–21.
Barros MB, Costa DL, Schubach TM, do Valle AC, Lorenzi NP, Teixeira JL, et al. Endemic of zoonotic sporotrichosis: profile of cases in children. Pediatr Infect Dis J. 2008;27(3):246–50.
Govender NP, Maphanga TG, Zulu TG, Patel J, Walaza S, Jacobs C, et al. An outbreak of lymphocutaneous sporotrichosis among mine-workers in South Africa. PLoS Negl Trop Dis. 2015;9(9), e0004096.
Alves SH, Boettcher CS, Oliveira DC, Tronco-Alves GR, Sgaria MA, Thadeu P, et al. Sporothrix schenckii associated with armadillo hunting in Southern Brazil: epidemiological and antifungal susceptibility profiles. Rev Soc Bras Med Trop. 2010;43(5):523–5.
Ramírez Soto MC. Sporotrichosis: the story of an endemic region in Peru over 28 Years (1985 to 2012). PLoS One 2015; 10(6):e0127924. This paper shows clearly the risk factors for sporotrichosis in an endemic region.
Song Y, Li SS, Zhong SX, Liu YY, Yao L, Huo SS. Report of 457 sporotrichosis cases from Jilin province, northeast China, a serious endemic region. J Eur Acad Dermatol Venereol. 2013;27(3):313–8.
Ursini F, Russo E, Leporini C, Calabria M, Bruno C, Tripolino C, et al. Lymphocutaneous Sporotrichosis during treatment with Anti-TNF-Alpha Monotherapy. Case Rep Rheumatol. 2015;2015:614504.
Teixeira Mde M, Rodrigues AM, Tsui CK, de Almeida LG, Van Diepeningen AD, van den Ende BG, et al. Asexual propagation of a virulent clone complex in a human and feline outbreak of sporotrichosis. Eukaryotic Cell. 2015;14(2):158–69.
Rodrigues AM, de Hoog GS, de Camargo ZP. Molecular diagnosis of pathogenic sporothrix species. PLoS Negl Trop Dis. 2015;9(12), e0004190. This paper describes the virulence factors for disease development.
Rodrigues AM, de Hoog GS, de Cássia PD, Brihante RS, Sidrim JJ, Gadelha MF, et al. Genetic diversity and antifungal susceptibility profiles in causative agents of sporotrichosis. BMC Infect Dis. 2014;14:219.
Rodrigues AM, de Hoog S, de Camargo ZP. Emergence of pathogenicity in the Sporothrix schenckii complex. Med Mycol. 2013;51(4):405–12.
Schechtman RC. Sporotrichosis: Part I. Skinmed. 2010;8(4):216–20.
Almeida-Paes R, de Oliveira LC, Oliveira MM, Gutierrez-Galhardo MC, Nosanchuk JD, Zancopé-Oliveira RM. Phenotypic characteristics associated with virulence of clinical isolates from the Sporothrix complex. Biomed Res Int. 2015;2015:212308. This paper describes the virulence factors for disease development.
Freitas DF, Santos SS, Almeida-Paes R, de Oliveira MM, do Valle AC, Gutierrez-Galhardo MC, et al. Increase in virulence of Sporothrix brasiliensis over five years in a patient with chronic disseminated sporotrichosis. Virulence. 2015;6(2):112–20.
Mario DA, Santos RC, Denardi LB, Vaucher Rde A, Santurio JM, Alves SH. Interference of melanin in the susceptibility profile of Sporothrix species to amphotericin B. Rev Iberoam Micol. 2016;33(1):21–5.
de Albornoz MB, Mendoza M, de Torres ED. Growth temperatures of isolates of Sporothrix schenckii from disseminated and fixed cutaneous lesions of sporotrichosis. Mycopathologia. 1986;95(2):81–3.
Kwon-Chung KJ. Comparison of isolates of Sporothrix schenckii obtained from fixed cutaneous lesions with isolates from other types of lesions. J Infect Dis. 1979;139(4):424–31.
Fernandes KS, Mathews HL, Lopes Bezerra LM. Differences in virulence of Sporothrix schenckii conidia related to culture conditions and cell-wall components. J Med Microbiol. 1999;48(2):195–203.
Almeida SR. Therapeutic monoclonal antibody for sporotrichosis. Front Microbiol. 2012;3:409.
Nascimento RC, Espíndola NM, Castro RA, Teixeira PA, Loureiro y Penha CV, Lopes-Bezerra LM, et al. Passive immunization with monoclonal antibody against a 70-kDa putative adhesin of Sporothrix schenckii induces protection in murine sporotrichosis. Eur J Immunol. 2008;38(11):3080–9.
Moreira JA, Freitas DF, Lamas CC. The impact of sporotrichosis in HIV-infected patients: a systematic review. Infection. 2015;43(3):267–76.
Tachibana T, Matsuyama T, Mitsuyama M. Involvement of CD4+ T cells and macrophages in acquired protection against infection with Sporothrix schenckii in mice. Med Mycol. 1999;37(6):397–404.
Barros MB, de Almeida PR, Schubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011;24(4):633–54.
Takenaka M, Yoshizaki A, Utani A, Nishimoto K. A survey of 165 sporotrichosis cases examined in Nagasaki prefecture from 1951 to 2012. Mycoses. 2014;57(5):294–8.
da Rosa AC, Scroferneker ML, Vettorato R, Gervini RL, Vettorato G, Weber A. Epidemiology of sporotrichosis: a study of 304 cases in Brazil. J Am Acad Dermatol. 2005;52(3 Pt 1):451–9.
Freitas DF, Lima IA, Curi CL, Jordão L, Zancopé-Oliveira RM, Valle AC, et al. Acute dacryocystitis: another clinical manifestation of sporotrichosis. Mem Inst Oswaldo Cruz. 2014;109(2):262–4.
Ramírez Soto MC. Sporotrichosis in the ocular adnexa: 21 cases in an endemic area in Peru and review of the literature. Am J Ophthalmol. 2016;162:173–9. e3.
Verma S, Verma GK, Singh G, Kanga A, Shanker V, Singh D, et al. Sporotrichosis in sub-Himalayan India. PLoS Negl Trop Dis. 2012;6(6), e1673.
Costa RO, Bernardes-Engemann AR, Azulay-Abulafia L, Benvenuto F, Neves Mde L, Lopes-Bezerra LM. Sporotrichosis in pregnancy: case reports of 5 patients in a zoonotic epidemic in Rio de Janeiro. Brazil An Bras Derm. 2011;86(5):995–8.
Bonifaz A, Saúl A, Paredes-Solis V, Fierro L, Rosales A, Palacios C, et al. Sporotrichosis in childhood: clinical and therapeutic experience in 25 patients. Pediatr Dermatol. 2007;24(4):369–72. This paper shows clearly the clinical spectrum for sporotrichosis in children.
Hernández PR, Borregales TE, de Garcia MM, Sauerteig E, Salfelder K. Symmetrical deforming cutaneous sporotrichosis of long duration. Mycoses. 1992;35(1–2):43–5.
Lopes-Bezerra LM. Sporothrix schenckii cell wall peptidorhamnomannans. Front Microbiol. 2011;2:243.
López-Romero E, Reyes-Montes Mdel R, Pérez-Torres A, Ruiz-Baca E, Villagómez-Castro JC, Mora-Montes HM, et al. Sporothrix schenckii complex and sporotrichosis, an emerging health problem. Future Microbiol. 2011;6(1):85–102.
Schechtman RC. Sporotrichosis: Part II. Skinmed. 2010;8(5):275–80.
Bonifaz A, Rojas-Padilla R, Tirado-Sánchez A. Sporotrichosis. The state of the art. In Medical Mycology: Current Trends and Future Prospects. Mehdi Razzaghi-Abyaneh, Masoomeh Shams-Ghahfarokhi, Mahendra Rai Eds. CRC Press, 2015. Pp. 234–53.
Quintella LP, Passos SR, do Vale AC, Galhardo MC, Barros MB, Cuzzi T, et al. Histopathology of cutaneous sporotrichosis in Rio de Janeiro: a series of 119 consecutive cases. J Cutan Pathol. 2011;38(1):25–32.
Liu X, Zhang Z, Hou B, Wang D, Sun T, Li F, et al. Rapid identification of Sporothrix schenckii in biopsy tissue by PCR. J Eur Acad Dermatol Venereol. 2013;27(12):1491–7.
Feeney KT, Arthur IH, Whittle AJ, Altman SA, Speers DJ. Outbreak of sporotrichosis, Western Australia. Emerg Infect Dis. 2007;13(8):1228–31.
Mata-Essayag S, Delgado A, Colella MT, Landaeta-Nezer ME, Rosello A, Perez de Salazar C, et al. Epidemiology of sporotrichosis in Venezuela. Int J Dermatol. 2013;52(8):974–80.
Song Y, Yao L, Zhong SX, Tian YP, Liu YY, Li SS. Infant sporotrichosis in northeast China: a report of 15 cases. Int J Dermatol. 2011;50(5):522–9.
Falqueto A, Bravim Maifrede S, Araujo RM. Unusual clinical presentation of sporotrichosis in three members of one family. Int J Dermatol. 2012;51(4):434–8.
Lee H, Kim do Y, Lee KH, Choi JS, Suh MK. Deformity of the earlobe caused by fixed cutaneous sporotrichosis in a pediatric patient. Int J Dermatol. 2015;54(5):e187–9.
Mahajan VK, Sharma NL, Sharma RC, Gupta ML, Garg G, Kanga AK. Cutaneous sporotrichosis in Himachal Pradesh. India Mycoses. 2005;48(1):25–31.
Tang MM, Tang JJ, Gill P, Chang CC, Baba R. Cutaneous sporotrichosis: a six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol. 2012;51(6):702–8.
Tlougan BE, Podjasek JO, Patel SP, Nguyen XH, Hansen RC. Neonatal sporotrichosis. Pediatr Dermatol. 2009;26(5):563–5.
Vásquez-del-Mercado E, Arenas R, Padilla-Desgarenes C. Sporotrichosis. Clin Dermatol. 2012;30(4):437–43.
Macedo PM, Lopes-Bezerra LM, Bernardes-Engemann AR, Orofino-Costa R. New posology of potassium iodide for the treatment of cutaneous sporotrichosis: study of efficacy and safety in 102 patients. J Eur Acad Dermatol Venereol. 2015;29(4):719–24. This paper clearly describes the protocol for using potassium iodide.
Cabezas C, Bustamante B, Holgado W, Begue RE. Treatment of cutaneous sporotrichosis with one daily dose of potassium iodide. Pediatr Infect Dis J. 1996;15(4):352–4.
Yamada K, Zaitz C, Framil VM, Muramatu LH. Cutaneous sporotrichosis treatment with potassium iodide: a 24 year experience in São Paulo State, Brazil. Rev Inst Med Trop Sao Paulo. 2011;53(2):89–93.
Agarwal S, Gopal K, Umesh, Kumar B. Sporotrichosis in Uttarakhand (India): a report of nine cases. Int J Dermatol. 2008;47(4):367–71.
Ishida K, de Castro RA, Borba Dos Santos LP, Quintella LP, Lopes-Bezerra LM, Rozental S. Amphotericin B, alone or followed by itraconazole therapy, is effective in the control of experimental disseminated sporotrichosis by Sporothrix brasiliensis. Med Mycol. 2015;53(1):34–41.
Ellis D. Amphotericin B: spectrum and resistance. J Antimicrob Chemother. 2002;49 Suppl 1:7–10.
Mario DN, Guarro J, Santurio JM, Alves SH, Capilla J. In vitro and in vivo efficacy of Amphotericin B combined with posaconazole against experimental disseminated Sporotrichosis. Antimicrob Agents Chemother. 2015;59(8):5018–21.
Kauffman CA, Bustamante B, Chapman SW, Pappas PG, Infectious Diseases Society of America. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(10):1255–65. This paper shows a practice guideline for treating sporotrichosis.
de Lima Barros MB, Schubach AO, de Vasconcellos Carvalhaes de Oliveira R, Martins EB, Teixeira JL, Wanke B. Treatment of cutaneous sporotrichosis with itraconazole—study of 645 patients. Clin Infect Dis. 2011;52(12):e200–6.
Fernández-Silva F, Capilla J, Mayayo E, Guarro J. Modest efficacy of voriconazole against murine infections by Sporothrix schenckii and lack of efficacy against Sporothrix brasiliensis. Mycoses. 2014;57(2):121–4.
Gutierrez-Galhardo MC, Zancopé-Oliveira RM, Monzón A, Rodriguez-Tudela JL, Cuenca-Estrella M. Antifungal susceptibility profile in vitro of Sporothrix schenckii in two growth phases and by two methods: microdilution and E-test. Mycoses. 2010;53(3):227–31.
Borba-Santos LP, Rodrigues AM, Gagini TB, Fernandes GF, Castro R, de Camargo ZP, et al. Susceptibility of Sporothrix brasiliensis isolates to amphotericin B, azoles, and terbinafine. Med Mycol. 2015;53(2):178–88.
Francesconi G, Francesconi do Valle AC, Passos SL, de Lima Barros MB, de Almeida Paes R, Curi AL, et al. Comparative study of 250 mg/day terbinafine and 100 mg/day itraconazole for the treatment of cutaneous sporotrichosis. Mycopathologia. 2011;171(5):349–54.
Bargman H. Successful treatment of cutaneous sporotrichosis with liquid nitrogen: report of three cases. Mycoses. 1995;38(7–8):285–7.
Lloret A, Hartmann K, Pennisi MG, Ferrer L, Addie D, Belák S, et al. Sporotrichosis in cats: ABCD guidelines on prevention and management. J Feline Med Surg. 2013;15:619–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tirado-Sánchez Andrés and Alexandro Bonifaz declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Fungal Infections of Skin and Subcutaneous Tissue
Rights and permissions
About this article
Cite this article
Tirado-Sánchez, A., Bonifaz, A. Sporotrichosis in Children: an Update. Curr Fungal Infect Rep 10, 107–116 (2016). https://doi.org/10.1007/s12281-016-0259-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-016-0259-0