Abstract
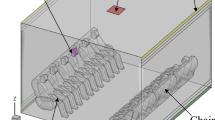
Infection is a major cause of death for the immunocompromised patients whose immune mechanisms are deficient. The most effective way of protecting these patients is the total environment protection such as protective isolation room (PIR). Unidirectional airflow ventilation is usually used in PIR. The supply air velocity in PIR can affect not only the cleanliness level of the room and total environment protection effects to the patients, but also the energy consumption and initial equipment investment of the room. Computational fluid dynamics (CFD) program is used to simulate the airflow field and the concentration distribution of the particles from human body and breathing. Three scenarios when the manikin is standing, sitting and lying are investigated in this study. The intensities of supply airflow with different velocities and the upward airflow induced by thermal plume with different postures are compared. The qualitative and quantitative analysis of the simulation results show that the required supply air velocity to control the thermal plume and particle dispersion from human body and breathing is at least 0.25 m/s when the manikin is standing or sitting, and 0.2 m/s when the manikin is lying.
Article PDF
Similar content being viewed by others
References
Balocco C, Petrone G, Cammarata G (2012). Assessing the effects of sliding doors on an operating theatre climate. Building Simulation, 5: 73–83.
Barnes RA, Rogers TR (1989). Control of an outbreak of nosocomial aspergillosis by laminar air-flow isolation. Journal of Hospital Infection, 14: 89–94.
Bolashikov ZD, Melikov AK, Kierat W, Popiolek Z, Brand M (2012). Exposure of health care workers and occupants to coughed airborne pathogens in a double-bed hospital patient room with overhead mixing ventilation. HVAC&R Research, 18: 602–615.
Chen C, Zhao B, Yang X, Li Y (2011). Role of two-way airflow owing to temperature difference in severe acute respiratory syndrome transmission: Revisiting the largest nosocomial severe acute respiratory syndrome outbreak in Hong Kong. Journal of the Royal Society Interface, 8: 699–710.
Chen F, Yu S, Lai A (2006). Modeling particle distribution and deposition in indoor environments with a new drift-flux model. Atmospheric Environment, 40: 357–367.
Chen Q (1995). Comparison of different k–epsilon models for indoor air flow computations. Numerical Heat Transfer Part B: Fundamentals, 28: 353–369.
Chow TT, Wang J (2012). Dynamic simulation on impact of surgeon bending movement on bacteria-carrying particles distribution in operating theatre. Building and Environment, 57: 68–80.
Chow TT, Yang XY (2005). Ventilation performance in the operating theatre against airborne infection: Numerical study on an ultraclean system. Journal of Hospital Infection, 59: 138–147.
Chow TT, Zhang L, Bai W (2006). The integrated effect of medical lamp position and diffuser discharge velocity on ultra-clean ventilation performance in an operating theatre. Indoor and Built Environment, 15: 315–331.
Clark RP, Toy N (1975). Natural convection around the human head. Journal of Physiology, 244: 283–293.
Deevy M, Sinai Y, Everitt P, Voigt L, Gobeau N (2008). Modelling the effect of an occupant on displacement ventilation with computational fluid dynamics. Energy and Buildings, 40: 255–264.
Dygert RK, Dang TQ, Russo JS, Khalifa HE (2009). Modelling of the human body to study the personal micro environment. ASHRAE Transactions, 115 (2): 407–420.
Fenelon LE (1995). Protective isolation: Who needs it? Journal of Hospital Infection, 30 (Supplement): 218–222.
FLUENT (2005). FLUENT Version 6.2. Lebanon, NH, USA: Fluent Inc.
Friberg S, Ardnor B, Lundholm R, Friberg B (2003). The addition of a mobile ultra-clean exponential laminar airflow screen to conventional operating room ventilation reduces bacterial contamination to operating box levels. Journal of Hospital Infection, 55: 92–97.
GB 50457-2008 (2009). Code for Design of Pharmaceutical Industry Clean Room. Beijing: China Planning Press. (in Chinese)
Ge Q, Li X, Inthavong K, Tu J (2013). Numerical study of the effects of human body heat on particle transport and inhalation in indoor environment. Building and Environment, 59: 1–9.
Ghia U, Konangi S, Kishore A, Gressel M, Mead K, Earnest G (2012). Assessment of health-care worker exposure to pandemic flu in hospital rooms. ASHRAE Transactions, 118(1): 442–449.
Gregory FP, Marghi RM, Willianm TW (2007). Potential for airborne contamination in turbulent-and unidirectional-airflow compounding aseptic isolators. American Journal of Health-System Pharmacy, 64: 622–631.
Gupta JK, Lin CH, Chen Q (2010). Characterizing exhaled airflow from breathing and talking. Indoor Air, 20: 31–39.
Halthway EA, Noakes CJ, Sleigh PA, Fletcher LA (2011). CFD simulation of airborne pathogen transport due to human activities. Building and Environment, 46: 2500–2511.
Homma H, Yakiyama M (1988). Examination of free convection around occupant's body caused by its metabolic heat. ASHRAE Transactions, 94(1): 104–124.
Incropera F, DeWitt D (1990). Fundamentals of Heat and Mass Transfer. New York: John Wiley and Sons.
International Organization for Standardization (ISO) (1999). ISO 14644-1, Cleanrooms and Associate Controlled Environments—Part 1—Classification of Air Cleanliness. Arlington Heights, IL, USA: The Institute of Environmental Sciences and Technology (IEST).
Jackie S, Russo H, Ezzat K (2010). CFD assessment of intake fraction in the indoor environment. Building and Environment, 45: 1968–1975.
Johnson AE, Fletcher B, Saunders CJ (1996). Air movement around a worker in a low-speed flow field. Annals of Occupational Hygiene, 40: 57–64.
Johnson DL, Lynch RA, Mead KR (2009). Containment effectiveness of expedient patient isolation units. American Journal of Infection Control, 37: 94–100.
Leung WT, Sze-To GN, Chao CYH, Yu SCT, Kwan JKC (2013). Study on the interzonal migration of airborne infectious particles in an isolation ward using benign bacteria. Indoor Air, 23: 148–161.
Lewis HE, Foster AR, Mullan BJ, Cox RN, Clark RP (1969). Aerodynamics of the human microenvironment. Lancet, 322: 1273–1277.
Li X, Inthavong K, Ge Q, Tu J (2013). Numerical investigation of particle transport and inhalation using standing thermal manikins. Building and Environment, 60: 116–125.
Licina D, Melikov A, Sekhar C, Tham KW (2015). Human convective boundary layer and its interaction with room ventilation flow. Indoor Air, 25: 21–35.
Licina D, Pantelic J, Melikov A, Sekhar C, Tham KW (2014). Experimental investigation of the human convective boundary layer in a quiescent indoor environment. Building and Environment, 75: 79–91.
Liu J, Wang H, Wen W (2009). Numerical simulation on a horizontal airflow for airborne particles control in hospital operating room. Building and Environment, 44: 2284–2289.
McFadden ER, Pichurko BM, Bowman HF, Ingenito E, Burns S, Dowling N, Solway J (1985). Thermal mapping of the airways in humans. Journal of Applied Physiology, 58: 564–570.
Memarzadeh F, Xu W (2012). Role of air changes per hour (ACH) in possible transmission of airborne infections. Building Simulation, 5: 15–28.
Murakami S, Zeng J, Hayashi T (1999). CFD analysis of wind environment around a human body. Journal of Wind Engineering and Industrial Aerodynamics, 83: 393–408.
Passweg JR, Rowlings PA, Atkinson KA, Barrett AJ, Gale RP, Gratwohl A, Jacobsen N, Klein JP, Ljungman P, Russell JA, Schaefer UW, Sobocinski KA, Vossen JM, Zhang MJ, Horowitz MM (1998). Influence of protective isolation on outcome of allogeneic bone marrow transplantation for leukemia. Bone Marrow Transplantation, 21: 1231–1238.
Qian H, Li Y (2010). Removal of exhaled particles by ventilation and deposition in a multibed airborne infection isolation room. Indoor Air, 20: 284–297.
Rouaud O, Havet M (2002). Computation of the airflow in a pilot scale clean room using k–e turbulence models. International Journal of Refrigeration, 25: 351–361.
Salmanzadeh M, Zahedi G, Ahmadi G, Marr DR, Glauser M (2012). Computational modeling of effects of thermal plume adjacent to body on the indoor airflow and particle transport. Journal of Aerosol Science, 53: 29–39.
Schlesinger A, Paul M, Gafter-Gvili A, Rubinovitch B, Leibovici L (2009). Infection-control interventions for cancer patients after chemotherapy: A systematic review and meta-analysis. The Lancet Infectious Diseases, 9: 97–107.
Smith LM, Reynolds WC (1992). On the Yakhot-Orszag renormalization group method for deriving turbulence statistics and models. Physics of Fluids A: Fluid Dynamics, 4: 364–390.
Storb R, Prentice RL, Buckner CD, Clift RA, Appelbaum F, Deeg J, Doney K, Hansen JA, Mason M, Sanders JE, Singer J, Sullivan KM, Witherspoon, RP, Thomas ED (1983). Graft versus host disease and survival in patients with aplastic anaemia treated by marrow grafts from HLA-identical siblings-Beneficial effect of a protective environment. New England Journal of Medicine, 308: 302–307.
Tang JW, Nicolle A, Pantelic J, Klettner CA, Su R, Kalliomaki P, Saarinen P, Koskela H, Reijula K, Mustakallio P, Cheong DKW, Sekhar C, Tham KW (2013). Different types of door-opening motions as contributing factors to containment failures in hospital isolation rooms. PLOS ONE, 8(6): e66663. doi:https://doi.org/10.1371/journal.pone.0066663.
Tung Y-C, Hu S-C, Tsai T-I, Chang I-L (2009a). An experimental study on ventilation efficiency of isolation room. Building and Environment, 44: 271–279.
Tung Y-C, Shih Y-C, Hu S-C (2009b). Numerical study on the dispersion of airborne contaminants from an isolation room in the case of door opening. Applied Thermal Engineering, 29: 1544–1551.
Voelker C, Maempel S, Kornadt O (2014). Measuring the human body’s microclimate using a thermal manikin. Indoor Air, 24: 567–579.
Yakhot V, Orszag SA (1986). Renormalization group analysis of turbulence I. Base theory. Journal of Scientific Computing, 1: 3–51.
Yakhot V, Orszag SA, Thangam S, Gatski TB, Speziale CG (1992). Development of turbulence models for shear flows by a double expansion technique. Physics of Fluids A: Fluid Dynamics, 4: 1510–1520.
Yakhot V, Smith LM (1992). The renormalization group, the e–expansion and derivation of turbulence models. Journal of Scientific Computing, 7: 35–61.
Yang C (2012). Research of particles and droplets transmission characteristics and ventilation control strategy in laminar airflow ward. PhD Thesis, Tsinghua University, China. (in Chinese)
Yang B, Melikov A, Sekhar C (2009a). Performance evaluation of ceiling mounted personalized ventilation system. ASHRAE Transactions, 115(2): 395–406.
Yang C, Yang X, Xu T, Sun L, Gong W (2009b). Optimization of bathroom ventilation design for an ISO Class 5 clean ward. Building Simulation, 2: 133–142.
Zhang T, Yin S, Wang S (2011). Quantify impacted scope of human expired air under different head postures and varying exhalation rates. Building and Environment, 46: 1928–1936.
Zhao B, Wu J (2005). Numerical investigation of particle diffusion in a clean room. Indoor and Built Environment, 14: 469–479.
Zoon WAC, Loomans MGLC, Hensen JLM (2011). Testing the effectiveness of operating room ventilation with regard to removal of airborne bacteria. Building and Environment, 46: 2570–2577.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, C., Yang, X. & Zhao, B. The ventilation needed to control thermal plume and particle dispersion from manikins in a unidirectional ventilated protective isolation room. Build. Simul. 8, 551–565 (2015). https://doi.org/10.1007/s12273-014-0227-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12273-014-0227-6