Abstract
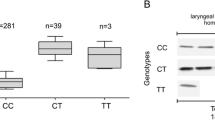
Basal cell carcinoma - BCC is considered a multifactorial neoplasm involving genetic, epigenetic and environmental factors. Where UVB radiation is considered the main physical agent involved in BCC carcinogenesis. The Brazil and state of Paraíba are exposed to high levels of UVB rays. The mismatch repair - MMR is important DNA repair mechanisms to maintain replication fidelity. Therefore, single nucleotide polymorphisms (SNPs) in genes encoding proteins involved in MMR may be potential molecular markers of susceptibility to BCC. The objective of this study was to evaluate and describe for the first time the SNPs rs560246973, rs2303425 and rs565410865 and risk of developing BCC. The present study analyzed 100 samples of paraffin-embedded tissue from patients with histopathological diagnosis of BCC and 100 control samples. The results were obtained by genotyping method, Dideoxy Unique Allele Specific – PCR (DSASP). The SNPs rs2303425 were not associated with Basal Cell Carcinoma. However, the SNPs rs560246973 and rs565410865 was shown to be associated with the development of BCC when compared to control samples (P < 0.0001). The SNPs rs565410865 was also statistical significance between the genotypes of and the age group (p = 0.0027) and tumor location (p = 0,0191). The result suggests that SNPs rs2303425 and rs565410865 are associated with susceptibility to the development of BCC in the Brazilian population and may be considered as potential molecular markers for BCC.




Similar content being viewed by others
References
Nikolaou V, Stratigos AJ, Tsao H (2012) Hereditary Nonmelanoma skin cancer. Semin Cutan Med Surg 31:204–210
DePry JL, Reed KB, Cook-Norris RH et al (2011) Iatrogenic immunosuppression and cutaneous malignancy. Clin Dermatol 29:602–613
Lichter MD, Karagas MR, Mott LA et al (2000) Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. Arch Dermatol 136:1007–1011
Noubissi FK, Kim T, Kawahara TN et al (2014) Role of CRD-BP in the growth of human basal cell carcinoma cells. J Investig Dermatol 134:1718–1724
Zink BS (2014) Câncer de pele: a importância do seu diagnóstico, tratamento e prevenção Revista HUPE 13:76–83
Kim S, Misra A (2007) SNP genotyping: technologies and biomedical applications. Annu Rev Biomed Eng 9:289–320
Dizdaroglu M (2015) Oxidatively induced DNA damage and its repair in cancer. Mutat Res 763:212–245
Erie DA, Weninger KR (2014) Single molecule studies of DNA mismatch repair. DNA repair 20:71–81
Mjelle R, Hegre SA, Aas PA et al (2015) Cell cycle regulation of human DNA repair and chromatin remodeling genes. DNA repair 30:53–67
Reyes GX, Schmidt TT, Kolodner RD et al (2015) New insights into the mechanism of DNA mismatch repair. Chromosoma. doi:10.1007/s00412-015-0514-0
Smith CE, Mendillo ML, Bowen N et al (2013) Dominant mutations in S. cerevisiae PMS1 identify the Mlh1-Pms1 endonuclease active site and an exonuclease 1-independent mismatch repair pathway. PLoS Genet. doi:10.1371/journal.pgen.1003869
Stojic L, Brun R, Jiricny J (2004) Mismatch repair and DNA damage signalling. DNA Repair 3:1091–1101
Han HJ, Maruyama M, Baba S et al (1995) Genomic structure of human mismatch repair gene, hMLH1, and its mutation analysis in patients with hereditary non-polyposis colorectal cancer (HNPCC). Hum Mol Genet 4:237–242
Fukuhara S, Chang I, Mitsui Y et al (2014) DNA mismatch repair gene MLH1 induces apoptosis in prostate cancer cells. Oncotarget 5:11297–11307
Fishel R, Lescoe MK, Rao MR et al (1993) The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 75:1027–1038
Kolodner RD, Hall NR, Lipford J et al (1994) Structure of the human MSH2 locus and analysis of two Muir-Torre kindreds for msh2 mutations. Genomics 24:516–526
Xiao XQ, Gong WD, Wang SZ et al (2012) Polymorphisms of mismatch repair gene hMLH1 and hMSH2 and risk of gastric cancer in a Chinese population. Oncol Lett 3:591–598
Sun MZ, Ju HX, Zhou ZW et al (2014) Single nucleotide polymorphisms of DNA mismatch repair genes MSH2 and MLH1 confer susceptibility to esophageal cancer. Int J Clin Exp Med 7:2329–2333
Smith TR, Levine EA, Freimanis RI et al (2008) Polygenic model of DNA repair genetic polymorphisms in human breast cancer risk. Carcinogenesis. doi:10.1093/carcin/bgn193
Mrkonjic M, Raptis S, Green RC et al (2007) MSH2− 118T> C and MSH6− 159C> T promoter polymorphisms and the risk of colorectal cancer. Carcinogenesis 28:2575–2580
Slováková P, Majerová L, Matáková T et al (2015) Mismatch repair Gene polymorphisms and association with lung cancer development. In: lung cancer and autoimmune disorders. Adv Exp Med Biol 833:15–22
Nishi R, Okuda Y, Watanabe E et al (2005) Centrin 2 stimulates nucleotide excision repair by interacting with Xeroderma Pigmentosum group C protein. Mol Cell Biol. doi:10.1128/MCB.25.13.5664-5674
Lima EM, Lopes OS, Soares LF et al (2015) Dideoxy single allele-specific PCR - DSASP new method to discrimination allelic. Braz Arch Biol Technol 58:414–420
Birch-Johansen F, Jensen A, Mortensen L et al (2010) Trends in the incidence of nonmelanoma skin cancer in Denmark 1978–2007: rapid incidence increase among young Danish women. Int J Cancer. doi:10.1002/ijc.25411
Smolarz B, Makowska M, Samulak D et al (2015) Gly322Asp and Asn127Ser single nucleotide polymorphisms (SNPs) of hMSH2 mismatch repair gene and the risk of triple-negative breast cancer in polish women. Familial Cancer. doi:10.1007/s10689-014-9746-z
Srivastava K, Srivastava A, Mittal B (2010) Polymorphisms in ERCC2, MSH2, and OGG1 DNA repair genes and gallbladder cancer risk in a population of northern India. Cancer 116:3160–3169
Hsieh YC, Cho EC, Tu SH et al (2017) MSH2 rs2303425 polymorphism is associated with early-onset breast cancer in Taiwan. Ann Surg Oncol. doi:10.1245/s10434-016-5168-5
Dahlman-Wright K, Qiao Y, Jonsson P et al (2012) Interplay between AP-1 and estrogen receptor α in regulating gene expression and proliferation networks in breast cancer cells. Carcinogenesis. doi:10.1093/carcin/bgs223
Ru Lee W, Chen CC, Liu S et al (2006) 17b-estradiol (E2) induces cdc25A Gene expression in breast cancer cells by genomic and non-genomic pathways. J Cell Biochem 99:209–220
Miyamoto T, Shiozawa T, Kashima H et al (2006) Estrogen up-regulates mismatch repair activity in normal and malignant endometrial glandular cells. Endocrinology 147:4863–4870
van der Klift HM, Jansen AM, van der Steenstraten N et al (2015) Splicing analysis for exonic and intronic mismatch repair gene variants associated with lynch syndrome confirms high concordance between minigene assays and patient RNA analyses. Mol Genet Genomic Med. doi:10.1002/mgg3.145
Wibom C, Sjöström S, Henriksson R et al (2012) DNA-repair gene variants are associated with glioblastoma survival. Acta Oncol. doi:10.3109/0284186X.2011.616284
Ward AJ, Cooper TA (2010) NIH public access. J Pathol 220:152–163
Zahary MN, Kaur G, Abu Hassan MR et al (2012) Germline mutation analysis of MLH1 and MSH2 in malaysian lynch syndrome patients. World J Gastroenterol. doi:10.3748/wjg.v18.i8.814
Langeberg WJ, Kwon EM, Koopmeiners JS et al (2010) Population-based study of the association of variants in mismatch repair genes with prostate cancer risk and outcomes. Cancer Epidemiol Biomark Prev. doi:10.1158/1055-9965.EPI-09-0800
Acknowledgements
The authors would like to thank Jimmy Johnson for proofreading the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Funding
This work was supported by grants of CAPES, CNPq and Clinica Dermatológica Santa Catarina; João Pessoa - PB – Brasil.
Ethical Approval
The present study is part of the thematic project approved by the Ethics Committee of the University Hospital Lauro Wanderley - UFPB under the code CAAE: 36,522,614.2.3001.5883.
Rights and permissions
About this article
Cite this article
da Silva Calixto, P., Lopes, O.S., dos Santos Maia, M. et al. Single-Nucleotide Polymorphisms of the MSH2 and MLH1 Genes, Potential Molecular Markers for Susceptibility to the Development of Basal Cell Carcinoma in the Brazilian Population. Pathol. Oncol. Res. 24, 489–496 (2018). https://doi.org/10.1007/s12253-017-0265-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-017-0265-8