Abstract
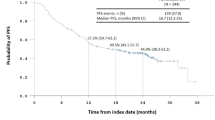
Home care medicine is a platform for providing supportive care for end-stage cancers. However, for undefined reasons, patients with hematological tumors (HTs) often fail to receive opportunities for home care. We, therefore, sought to delineate the clinical differences between solid tumors (STs) and HTs and to determine whether home care is effective for patients with HTs, as well as those with STs. We retrospectively analyzed the treatments, prognosis, and places of death of patients with STs (n = 99) and HTs (n = 20) who received palliative home care in our clinic and subsequently died between May 2016 and May 2018. Patients with HTs commonly required intravenous antibiotics, platelet transfusion, and red blood cell transfusion, while patients with STs tended to more frequently require the use of opioids. Importantly, there were no significant differences between the cohorts with respect to survival time and frequency of emergent visits to patients after their referral to us. Furthermore, most patients in both groups died at home. More than 50% of patients were not admitted to hospitals during our follow-up. Collectively, while therapeutic approaches sometimes differ, this study provides clinical evidence that palliative home care can be feasible even for patients with HTs.


Similar content being viewed by others
Abbreviations
- HTs:
-
Hematological tumors
- STs:
-
Solid tumors
- MDS:
-
Myelodysplastic syndromes
- QoL:
-
Quality of life
References
Niscola P, Tendas A, Giovannini M, Scaramucci L, Perrotti A, de Fabritiis P, et al. Caring for terminal patients in haematology: the urgent need of a new research agenda. Support Care Cancer. 2015;23:5–7.
Howell DA, Shellens R, Roman E, Garry AC, Patmore R, Howard MR. Haematological malignancy: are patients appropriately referred for specialist palliative and hospice care? A systematic review and meta-analysis of published data. Palliat Med. 2011;25:630–41.
Adachi A, Tsukada Y, Kondo S, Asakura K, Matsuki E, Kawagoe S, et al. Questionnaire survey on current status of home care and support for patients with hematological diseases. Rinsho Ketsueki. 2014;55:2262–70.
Higginson IJ, Koffman J. Public health and palliative care. Clin Geriatr Med. 2005;21:45–55.
Niscola P, de Fabritiis P, Cartoni C, Romani C, Sorrentino F, Dentamaro T, et al. Home care management of patients affected by hematologic malignancies: a review. Haematol. 2006;91:1523–9.
Niscola P, Tendas A, Giovannini M, Cupelli L, Trawinska MM, Palombi M, et al. Transfusions at home in patients with myelodysplastic syndromes. Leuk Res. 2012;36:684–8.
Howell DA, Roman E, Cox H, Smith AG, Patmore R, Garry AC, et al. Destined to die in hospital? Systematic review and meta-analysis of place of death in haematological malignancy. BMC Palliat Care. 2010;9:9.
Howell DA, Wang HI, Smith AG, Howard MR, Patmore RD, Roman E. Place of death in haematological malignancy: variations by disease sub-type and time from diagnosis to death. BMC Palliat Care. 2013;12:42.
Joske D, McGrath P. Palliative care in haematology. Intern Med J. 2007;37:589–90.
McGrath P. Palliative care for patients with hematological malignancies–if not, why not? J Palliat Care. 1999;15:24–30.
van Tiel FH, Harbers MM, Kessels AG, Schouten HC. Home care versus hospital care of patients with hematological malignancies and chemotherapy-induced cytopenia. Ann Oncol. 2005;16:195–205.
Ringdén O, Sadeghi B, Moretti G, Finnbogadottir S, Eriksson B, Mattsson J, et al. Long-term outcome in patients treated at home during the pancytopenic phase after allogeneic haematopoietic stem cell transplantation. Int J Hematol. 2018;107:478–85.
LeBlanc TW, Egan PC, Olszewski AJ. Transfusion dependence, use of hospice services, and quality of end-of-life care in leukemia. Blood. 2018;132:717–26.
Garcia D, Aguilera A, Antolin F, Arroyo JL, Lozano M, Sanroma P, et al. Home transfusion: three decades of practice at a tertiary care hospital. Transfusion. 2018;58:2309–19.
Ohashi K, Adachi A, Hosoda T. A survey on home care needs of patients with hematological diseases. Gan To Kagaku Ryoho (in press).
Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315–21.
McGrath P. Are we making progress? Not in haematology! Omega (Westport). 2002;45:331–48.
Maddocks I, Bentley L, Sheedy J. Quality of life issues in patients dying from haematological diseases. Ann Acad Med Singapore. 1994;23:244–8.
Alt-Epping B, Wulf G, Nauck F. Palliative care for patients with hematological malignancies—a case series. Ann Hematol. 2011;90:613–5.
Fadul NA, El Osta B, Dalal S, Poulter VA, Bruera E. Comparison of symptom burden among patients referred to palliative care with hematologic malignancies versus those with solid tumors. J Palliat Med. 2008;11:422–7.
Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120:1743–9.
Amano K, Morita T, Tatara R, Katayama H, Uno T, Takagi I. Association between early palliative care referrals, inpatient hospice utilization, and aggressiveness of care at the end of life. J Palliat Med. 2015;18:270–3.
Dionne-Odom JN, Azuero A, Lyons KD, Hull JG, Tosteson T, Li Z, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: outcomes From the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33:1446–52.
Acknowledgements
We thank Sachie Yamaguchi, Akiko Ryuo, Takahiro Suzuki, Jun Suzuki, Nobumasa Omura, Maki Omura, and Hironobu Hashimoto for their unselfish dedication to patient care.
Author information
Authors and Affiliations
Contributions
Study conception and design, data acquisition, and data analysis and interpretation: TI, KO, CO, SO, SO, KM, and TS. Article drafting or critical revision for important intellectual content: TI, KO, KM, and TS. Final approval of the submitted version: TI, KO, CO, SO, SO, KM, and TS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ishida, T., Ohashi, K., Okina, C. et al. Characteristics of palliative home care for patients with hematological tumors compared to those of patients with solid tumors. Int J Hematol 110, 237–243 (2019). https://doi.org/10.1007/s12185-019-02673-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-019-02673-3