Abstract
Anticonvulsant administration is the standard of care for prevention of busulfan-induced seizures (BIS) in hematopoietic stem cell transplantation (HSCT). While valproate interacts with other drugs, including carbapenem antibiotics, levetiracetam has no known clinically significant interactions. Only a few reports have discussed the use of levetiracetam for the prevention of BIS in HSCT recipients. This retrospective study aimed to evaluate the efficacy and safety of valproate and levetiracetam for BIS prophylaxis in adult HSCT recipients. We identified patients who received valproate or levetiracetam to prevent BIS at the National Cancer Center Hospital from December 2015 to November 2017. Ninety-one patients were analyzed (valproate group 45; levetiracetam group 46). No BIS occurred in either group. The pattern of anticonvulsant-related adverse events was similar in both groups, except for a higher incidence of rash in the valproate group. Carbapenem antibiotics were more frequently used in the levetiracetam group than in the valproate group. In conclusion, valproate and levetiracetam are effective and safe for the prophylaxis of BIS. Levetiracetam may be more useful in patients colonized with extended-spectrum beta-lactamase-producing bacteria due to its lack of any clinically significant drug–drug interactions.
Similar content being viewed by others
References
Vassal G, Deroussent A, Hartmann O, Challine D, Benhamou E, Valteau-Couanet D, et al. Dose-dependent neurotoxicity of high-dose busulfan in children: a clinical and pharmacological study. Cancer Res. 1990;50:6203–7.
Hassan M, Oberg G, Ehrsson H, Ehrnebo M, Wallin I, Smedmyr B, et al. Pharmacokinetic and metabolic studies of high-dose busulphan in adults. Eur J Clin Pharmacol. 1989;36:525–30.
Vassal G, Gouyette A, Hartmann O, Pico JL, Lemerle J. Pharmacokinetics of high-dose busulfan in children. Cancer Chemother Pharmacol. 1989;24:386–90.
Meloni G, Raucci U, Pinto RM, Spalice A, Vignetti M, Iannetti P. Pretransplant conditioning with busulfan and cyclophosphamide in acute leukemia patients: neurological and electroencephalographic prospective study. Ann Oncol. 1992;3:145–8.
Kobayashi R, Watanabe N, Iguchi A, Cho Y, Yoshida M, Arioka H, et al. Electroencephalogram abnormality and high-dose busulfan in conditioning regimens for stem cell transplantation. Bone Marrow Transpl. 1998;21:217–20.
Santos GW. Busulfan (Bu) and cyclophosphamide (Cy) for marrow transplantation. Bone Marrow Transpl. 1989;4(Suppl 1):236–9.
Eberly AL, Anderson GD, Bubalo JS, McCune JS. Optimal prevention of seizures induced by high-dose busulfan. Pharmacotherapy. 2008;28:1502–10.
De La Camara R, Tomas JF, Figuera A, Berberana M, Fernandez-Ranada JM. High dose busulfan and seizures. Bone Marrow Transpl. 1991;7:363–4.
Soni S, Skeens M, Termuhlen AM, Bajwa RP, Gross TG, Pai V. Levetiracetam for busulfan-induced seizure prophylaxis in children undergoing hematopoietic stem cell transplantation. Pediatr Blood Cancer. 2012;59:762–4.
Saito AM, Kami M, Mori S, Kanda Y, Suzuki R, Mineishi S, et al. Prospective phase II trial to evaluate the complications and kinetics of chimerism induction following allogeneic hematopoietic stem cell transplantation with fludarabine and busulfan. Am J Hematol. 2007;82:873–80.
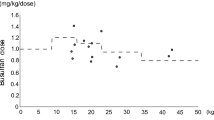
Takamatsu Y, Sasaki N, Eto T, Nagafuji K, Abe Y, Choi I, et al. Individual dose adjustment of oral busulfan using a test dose in hematopoietic stem cell transplantation. Int J Hematol. 2007;86:261–8.
de Jonge ME, Huitema AD, van Dam SM, Beijnen JH, Rodenhuis S. Significant induction of cyclophosphamide and thiotepa metabolism by phenytoin. Cancer Chemother Pharmacol. 2005;55:507–10.
McCune JS, Batchelder A, Deeg HJ, Gooley T, Cole S, Phillips B, et al. Cyclophosphamide following targeted oral busulfan as conditioning for hematopoietic cell transplantation: pharmacokinetics, liver toxicity, and mortality. Biol Blood Marrow Transpl. 2007;13:853–62.
Clause D, Decleire PY, Vanbinst R, Soyer A, Hantson P. Pharmacokinetic interaction between valproic acid and meropenem. Intensive Care Med. 2005;31:1293–4.
Desai J. Perspectives on interactions between antiepileptic drugs (AEDs) and antimicrobial agents. Epilepsia. 2008;49(Suppl 6):47–9.
Kwon JC, Kim SH, Choi JK, Cho SY, Park YJ, Park SH, et al. Epidemiology and clinical features of bloodstream infections in hematology wards: one year experience at the catholic blood and marrow transplantation center. Infect Chemother. 2013;45:51–61.
Mikulska M, Del Bono V, Raiola AM, Bruno B, Gualandi F, Occhini D, et al. Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transpl. 2009;15:47–53.
Choeyprasert W, Hongeng S, Anurathapan U, Pakakasama S. Bacteremia during neutropenic episodes in children undergoing hematopoietic stem cell transplantation with ciprofloxacin and penicillin prophylaxis. Int J Hematol. 2017;105:213–20.
Floeter AE, McCune JS. Levetiracetam for the prevention of busulfan-induced seizures in pediatric hematopoietic cell transplantation recipients. J Oncol Pharm Pract. 2017;23:344–9.
Akiyama K, Kume T, Fukaya M, Shiki I, Enami T, Tatara R, et al. Comparison of levetiracetam with phenytoin for the prevention of intravenous busulfan-induced seizures in hematopoietic cell transplantation recipients. Cancer Chemother Pharmacol. 2018;82:717–21.
Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, et al. Venoocclusive disease of the liver following bone marrow transplantation. Transpl. 1987;44:778–83.
Mendu DR, Soldin SJ. Simultaneous determination of levetiracetam and its acid metabolite (ucb L057) in serum/plasma by liquid chromatography tandem mass spectrometry. Clin Biochem. 2010;43:485–9.
Marcus R, Goldman J. Convulsions due to high-dose busulphan. Lancet. 1984;324:1463.
Beelen DW, Quabeck K, Graeven U, Sayer HG, Mahmoud HK, Schaefer UW. Acute toxicity and first clinical results of intensive postinduction therapy using a modified busulfan and cyclophosphamide regimen with autologous bone marrow rescue in first remission of acute myeloid leukemia. Blood. 1989;74:1507–16.
Grigg AP, Shepherd JD, Phillips GL. Busulphan and phenytoin. Ann Intern Med. 1989;111:1049–50.
Sheridan WP, Boyd AW, Green MD, Russell DM, Thomas RJ, McGrath KM, et al. High-dose chemotherapy with busulphan and cyclophosphamide and bone-marrow transplantation for drug-sensitive malignancies in adults: a preliminary report. Med J Aust. 1989;151:379–86.
Murphy CP, Harden EA, Thompson JM. Generalized seizures secondary to high-dose busulfan therapy. Ann Pharmacother. 1992;26:30–1.
Atra A, Whelan JS, Calvagna V, Shankar AG, Ashley S, Shepherd V, et al. High-dose busulphan/melphalan with autologous stem cell rescue in Ewing’s sarcoma. Bone Marrow Transpl. 1997;20:843–6.
Russell JA, Tran HT, Quinlan D, Chaudhry A, Duggan P, Brown C, et al. Once-daily intravenous busulfan given with fludarabine as conditioning for allogeneic stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Biol Blood Marrow Transpl. 2002;8:468–76.
Chan KW, Mullen CA, Worth LL, Choroszy M, Koontz S, Tran H, et al. Lorazepam for seizure prophylaxis during high-dose busulfan administration. Bone Marrow Transpl. 2002;29:963–5.
Schwarer AP, Opat SS, Watson AL, Cole-Sinclair MF. Clobazam for seizure prophylaxis during busulfan chemotherapy. Lancet. 1995;346:1238.
Hassan M, Oberg G, Bjorkholm M, Wallin I, Lindgren M. Influence of prophylactic anticonvulsant therapy on high-dose busulphan kinetics. Cancer Chemother Pharmacol. 1993;33:181–6.
Shaw PJ, Scharping CE, Brian RJ, Earl JW. Busulfan pharmacokinetics using a single daily high-dose regimen in children with acute leukemia. Blood. 1994;84:2357–62.
Zwaveling J, Bredius RG, Cremers SC, Ball LM, Lankester AC, Teepe-Twiss IM, et al. Intravenous busulfan in children prior to stem cell transplantation: study of pharmacokinetics in association with early clinical outcome and toxicity. Bone Marrow Transpl. 2005;35:17–23.
Meloni G, Nasta L, Pinto RM, Spalice A, Raucci U, Iannetti P. Clonazepam prophylaxis and busulfan-related myoclonic epilepsy in autografted acute leukemia patients. Haematologica. 1995;80:532–4.
Nanau RM, Neuman MG. Adverse drug reactions induced by valproic acid. Clin Biochem. 2013;46:1323–38.
Buoli M, Serati M, Botturi A, Altamura AC. The risk of thrombocytopenia during valproic acid therapy: a critical summary of available clinical data. Drugs R&D. 2018;18:1–5.
Brodie MJ, Perucca E, Ryvlin P, Ben-Menachem E, Meencke HJ. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Neurology. 2007;68:402–8.
Peyrl A, Weichert N, Kuhl JS, Ebell W, Hernaiz Driever P. Levetiracetam as a possible cause of secondary graft failure after allogenic hematopoietic stem cell transplantation. Eur J Paediatr Neurol. 2015;19:75–7.
Slattery JT, Kalhorn TF, McDonald GB, Lambert K, Buckner CD, Bensinger WI, et al. Conditioning regimen-dependent disposition of cyclophosphamide and hydroxycyclophosphamide in human marrow transplantation patients. J Clin Oncol. 1996;14:1484–94.
Kangarloo SB, Naveed F, Ng ES, Chaudhry MA, Wu J, Bahlis NJ, et al. Development and validation of a test dose strategy for once-daily i.v. busulfan: importance of fixed infusion rate dosing. Biol Blood Marrow Transpl. 2012;18:295–301.
Madden T, de Lima M, Thapar N, Nguyen J, Roberson S, Couriel D, et al. Pharmacokinetics of once-daily IV busulfan as part of pretransplantation preparative regimens: a comparison with an every 6-hour dosing schedule. Biol Blood Marrow Transpl. 2007;13:56–64.
Ren S, Yang JS, Kalhorn TF, Slattery JT. Oxidation of cyclophosphamide to 4-hydroxycyclophosphamide and deschloroethylcyclophosphamide in human liver microsomes. Cancer Res. 1997;57:4229–35.
Anderson GD. A mechanistic approach to antiepileptic drug interactions. Ann Pharmacother. 1998;32:554–63.
Otoul C, De Smedt H, Stockis A. Lack of pharmacokinetic interaction of levetiracetam on carbamazepine, valproic acid, topiramate, and lamotrigine in children with epilepsy. Epilepsia. 2007;48:2111–5.
Chong Y, Yakushiji H, Ito Y, Kamimura T. Clinical and molecular epidemiology of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a long-term study from Japan. Eur J Clin Microbiol Infect Dis. 2011;30:83–7.
Patsalos PN, Berry DJ, Bourgeois BF, Cloyd JC, Glauser TA, Johannessen SI, et al. Antiepileptic drugs–best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring, ILAE Commission on Therapeutic Strategies. Epilepsia. 2008;49:1239–76.
Yazal Erdem A, Azik F, Tavil B, Teber S, Tunc B, Uckan D. Busulfan triggers epileptic seizures under levetiracetam and valproic acid therapy. Pediatr Transpl. 2014;18:412–3.
Author information
Authors and Affiliations
Contributions
TN, TT, TF, and HT designed the study. TN and TT performed the statistical analysis. KK, YN, HH, AI, YI, SK, and SWK reviewed the results. All authors wrote and critically revised the manuscript for important intellectual content, and approved the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakashima, T., Tanaka, T., Koido, K. et al. Comparison of valproate and levetiracetam for the prevention of busulfan-induced seizures in hematopoietic stem cell transplantation. Int J Hematol 109, 694–699 (2019). https://doi.org/10.1007/s12185-019-02637-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-019-02637-7