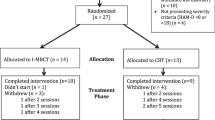
Cognitive-Behavioral Therapy (CBT) has a significant adjunctive effect in the treatment of Major Depressive Disorder (MDD), however its use as monotherapy in group-based approaches is less explored. We assessed the responses of distinct psychophysiological domains after a group-based CBT (gCBT, 16 weeks) intervention in drug-free patients with mild-moderate MDD (n = 20; women = 11) and compared them with a healthy control group (n = 25, women = 13). The treatment resulted in 65% of response and 55% of remission rates. Significant reductions in depressive and anxiety symptoms and increase in self-esteem and sleep quality were observed as gCBT responses. Moreover, after treatment, patients regulated their previously deregulated salivary cortisol awakening response and sleep quality toward healthy parameters. These improvements were correlated among themselves and dependent of remission outcome. Remitted patients showed larger improvements than non-remitted for all psychophysiological domains, except for serum cortisol that significantly changed only for no-remitted patients after gCBT but did not reached controls levels. Further, better baseline sleep quality was predictor of remission. The psychophysiological changes found support the use of gCBT as monotherapy treatment for mild-moderate MDD, corroborate the importance of the observation of the patients in theirs whole sociopsychophysiological condition since they are related to remission outcome and then stimulate further studies of validation of clinical protocols that work on all of these psychophysiological domains studied.
Trial Registration U1111–1215-4472. Registered 21 August 2018, http://www.ensaiosclinicos.gov.br/rg/RBR-3npbf8/





Similar content being viewed by others
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
American Psychiatric Association. (2014). DSM-5: Manual diagnóstico e estatístico de transtornos mentais. Porto Alegre, RS: Artmed Editora.
Baardseth, T. P., Goldberg, S. B., Pace, B. T., Wislocki, A. P., Frost, N. D., Siddiqui, J. R., Lindemann, A. M., Kivlighan III, D. M., Laska, K. M., del Re, A. C., Minami, T., & Wampold, B. E. (2013). Cognitive-behavioral therapy versus other therapies: Redux. Clinical Psychology Review, 33(3), 395–405. https://doi.org/10.1016/j.cpr.2013.01.004.
Beck, J. (2011). Cognitive behavior therapy: Basics and beyond. New York, NY: The Guilford Press.
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. https://doi.org/10.1037/0022-006X.56.6.893.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Bertolazi, A. N., Fagondes, S. C., Hoff, L. S., Dartora, E. G., da Silva Miozzo, I. C., de Barba, M. E. F., & Menna Barreto, S. S. (2011). Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Medicine, 12(1), 70–75. https://doi.org/10.1016/j.sleep.2010.04.020.
Bieling, P. J., McCabe, R. E., & Antony, M. M. (2006). Cognitive-behavioral therapy in groups. New York, NY: The Guilford press.
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357–1366. https://doi.org/10.1016/S0140-6736(17)32802-7.
Cunha, J. A. (2001). Manual da versão em português das Escalas Beck. São Paulo, SP: Casa do Psicólogo.
Davey, C. G., Chanen, A. M., Hetrick, S. E., Cotton, S. M., Ratheesh, A., Amminger, G. P., Koutsogiannis, J., Phelan, M., Mullen, E., Harrison, B. J., Rice, S., Parker, A. G., Dean, O. M., Weller, A., Kerr, M., Quinn, A. L., Catania, L., Kazantzis, N., McGorry, P. D., & Berk, M. (2019). The addition of fluoxetine to cognitive behavioural therapy for youth depression (YoDA-C): A randomised, double-blind, placebo-controlled, multicentre clinical trial. The Lancet Psychiatry, 6(9), 735–744. https://doi.org/10.1016/S2215-0366(19)30215-9.
de Azevedo Cardoso, T., Mondin, T. C., Spessato, B. C., de Avila Quevedo, L., de Mattos Souza, L. D., da Silva, R. A., & Jansen, K. (2014). The impact of anxious symptoms in the remission of depressive symptoms in a clinical trial for depression: Follow-up of six months. Journal of Affective Disorders, 168, 331–336. https://doi.org/10.1016/j.jad.2014.03.034.
Dean, J., & Keshavan, M. (2017). The neurobiology of depression: An integrated view. Asian Journal of Psychiatry., 27, 101–111. https://doi.org/10.1016/j.ajp.2017.01.025.
Dedovic, K., & Ngiam, J. (2015). The cortisol awakening response and major depression: Examining the evidence. Neuropsychiatric Disease and Treatment, 11, 1181–1189. https://doi.org/10.2147/NDT.S62289.
Dunlop, B. W., LoParo, D., Kinkead, B., Mletzko-Crowe, T., Cole, S. P., Nemeroff, C. B., Mayberg, H. S., & Craighead, W. E. (2019). Benefits of sequentially adding cognitive-behavioral therapy or antidepressant medication for adults with nonremitting depression. American Journal of Psychiatry, 176(4), 275–286. https://doi.org/10.1176/appi.ajp.2018.18091075.
Fernandes, B. S., Williams, L. M., Steiner, J., Leboyer, M., Carvalho, A. F., & Berk, M. (2017). The new field of ‘precision psychiatry’. BMC Medicine, 15(1), 80. https://doi.org/10.1186/s12916-017-0849-x.
Fischer, S., Strawbridge, R., Vives, A. H., & Cleare, A. J. (2017). Cortisol as a predictor of psychological therapy response in depressive disorders: Systematic review and meta-analysis. British Journal of Psychiatry, 210(2), 105–109. https://doi.org/10.1192/bjp.bp.115.180653.
Galvão-Coelho, N. L., Silva, H. P. A., & de Sousa, M. B. C. (2015). Resposta ao estresse: II. Resiliência e vulnerabilidade. Estudos de Psicologia, 20(2), 72–81. https://doi.org/10.5935/1678-4669.20150009.
Gomes-Oliveira, M. H., Gorenstein, C., Neto, F. L., Andrade, L. H., & Wang, Y. P. (2012). Validation of the Brazilian Portuguese version of the Beck depression inventory-II in a community sample. Revista Brasileira de Psiquiatria, 34(4), 389–394. https://doi.org/10.1016/j.rbp.2012.03.005.
Guidi, J., Brakemeier, E. L., Bockting, C. L. H., Cosci, F., Cuijpers, P., Jarrett, R. B., Linden, M., Marks, I., Peretti, C. S., Rafanelli, C., Rief, W., Schneider, S., Schnyder, U., Sensky, T., Tomba, E., Vazquez, C., Vieta, E., Zipfel, S., Wright, J. H., & Fava, G. A. (2018). Methodological recommendations for trials of psychological interventions. Psychotherapy and Psychosomatics. https://doi.org/10.1159/000490574.
Haller, H., Anheyer, D., Cramer, H., & Dobos, G. (2019). Complementary therapies for clinical depression: An overview of systematic reviews. BMJ Open, 9, e028527. https://doi.org/10.1136/bmjopen-2018-028527.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. https://doi.org/10.1136/jnnp.23.1.56.
He, C., Gong, L., Yin, Y., Yuan, Y., Zhang, H., Lv, L., Zhang, X., Soares, J. C., Zhang, H., Xie, C., & Zhang, Z. (2019). Amygdala connectivity mediates the association between anxiety and depression in patients with major depressive disorder. Brain Imaging and Behavior, 13(4), 1146–1159. https://doi.org/10.1007/s11682-018-9923-z.
Holland, J. M., Schatzberg, A. F., O’Hara, R., Marquett, R. M., & Gallagher-Thompson, D. (2013). Pretreatment cortisol levels predict posttreatment outcomes among older adults with depression in cognitive behavioral therapy. Psychiatry Research, 210(2), 444–450. https://doi.org/10.1016/j.psychres.2013.07.033.
Howland, R. H. (2008). Sequenced treatment alternatives to relieve depression (STAR*D). Journal of Psychosocial Nursing and Mental Health Services, 46(9), 21–24. https://doi.org/10.3928/02793695-20080901-06.
Hutz, C. S., & Zanon, C. (2011). Revision of the adaptation, validation, and normatization of the Roserberg self-esteem scale. Avaliação Psicológica, 10(1), 41–9.
Kennis, M., Gerritsen, L., van Dalen, M., Williams, A., Cuijpers, P., & Bockting, C. (2020). Prospective biomarkers of major depressive disorder: A systematic review and meta-analysis. Molecular Psychiatry, 25(2), 321–338. https://doi.org/10.1038/s41380-019-0585-z.
Kolubinski, D. C., Frings, D., Nikčević, A. V., Lawrence, J. A., & Spada, M. M. (2018). A systematic review and meta-analysis of CBT interventions based on the Fennell model of low self-esteem. Psychiatry Research, 267, 296–305. https://doi.org/10.1016/j.psychres.2018.06.025.
LeMoult, J., & Joormann, J. (2014). Depressive rumination alters cortisol decline in major depressive disorder. Biological Psychology, 100, 50–55. https://doi.org/10.1016/j.biopsycho.2014.05.001.
Li, J.-M., Zhang, Y., Su, W.-J., Liu, L.-L., Gong, H., Peng, W., & Jiang, C.-L. (2018). Cognitive behavioral therapy for treatment-resistant depression: A systematic review and meta-analysis. Psychiatry Research, 268, 243–250. https://doi.org/10.1016/j.psychres.2018.07.020.
Liu, Q., He, H., Yang, J., Feng, X., Zhao, F., & Lyu, J. (2020). Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. Journal of Psychiatric Research, 126, 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002.
Lopez-Duran, N. L., Kovacs, M., & George, C. J. (2009). Hypothalamic–pituitary–adrenal axis dysregulation in depressed children and adolescents: A meta-analysis. Psychoneuroendocrinology, 34(9), 1272–1283. https://doi.org/10.1016/j.psyneuen.2009.03.016.
McEvoy, P. M., Burgess, M. M., & Nathan, P. (2014). The relationship between interpersonal problems, therapeutic alliance, and outcomes following group and individual cognitive behaviour therapy. Journal of Affective Disorders., 157, 25–32. https://doi.org/10.1016/j.jad.2013.12.038.
Nyer, M., Farabaugh, A., Fehling, K., Soskin, D., Holt, D., Papakostas, G. I., Pedrelli, P., Fava, M., Pisoni, A., Vitolo, O., & Mischoulon, D. (2013). Relationship between sleep disturbance and depression, anxiety, and functioning in college students. Depression and Anxiety., 30, 873–880. https://doi.org/10.1002/da.22064.
Ohayon, M. M., & Roth, T. (2003). Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research, 37(1), 9–15. https://doi.org/10.1016/S0022-3956(02)00052-3.
Pompili, M., Innamorati, M., Lamis, D. A., Erbuto, D., Venturini, P., Ricci, F., Serafini, G., Amore, M., & Girardi, P. (2014). The associations among childhood maltreatment, “male depression” and suicide risk in psychiatric patients. Psychiatry Research, 220(1–2), 571–578. https://doi.org/10.1016/j.psychres.2014.07.056.
Rosenberg, M. (1979). Conceiving the self. New York, NY: Basic.
Santiago, G, T, P., de Menezes Galvão, A, C., de Almeida, R, N., Mota-Rolim, S, A., Palhano-Fontes, F., Maia-de-Oliveira, J, P., de Araújo D, B., Lobão-Soares B., Galvão-Coelho N, L. (2020). Changes in Cortisol but Not in Brain-Derived Neurotrophic Factor Modulate the Association Between Sleep Disturbances and Major Depression. Frontiers in Behavioral Neuroscience, 14. https://doi.org/10.3389/fnbeh.2020.00044
Sbarra, D. A., & Allen, J. J. B. (2009). Decomposing depression: On the prospective and reciprocal dynamics of mood and sleep disturbances. Journal of Abnormal Psychology, 118(1), 171–182. https://doi.org/10.1037/a0014375.
Schaub, A., Goldmann, U., Mueser, T. K., Goerigk, S., Hautzinger, M., Roth, E., Charypar, M., Engel, R., & Möller, H. J. (2018). Efficacy of extended clinical management, group CBT, and group plus individual CBT for major depression: Results of a two-year follow-up study. Journal of Affective Disorders, 238, 570–578. https://doi.org/10.1016/j.jad.2018.05.081.
Schüle, C. (2007). Neuroendocrinological mechanisms of actions of antidepressant drugs. Journal of Neuroendocrinology, 19(3), 213–226. https://doi.org/10.1111/j.1365-2826.2006.01516.x.
Serafini, G., Gonda, X., Canepa, G., Pompili, M., Rihmer, Z., Amore, M., & Engel-Yeger, B. (2017). Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. Journal of Affective Disorders., 210, 249–257. https://doi.org/10.1016/j.jad.2016.12.019.
Sowislo, J. F., & Orth, U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin, 139(1), 213–240. https://doi.org/10.1037/a0028931.
Thimm, J. C., & Antonsen, L. (2014). Effectiveness of cognitive behavioral group therapy for depression in routine practice. BMC Psychiatry, 14, 292. https://doi.org/10.1186/s12888-014-0292-x.
Wüst, S., Wolf, J., Hellhammer, D. H., Federenko, I., Schommer, N., & Kirschbaum, C. (2000). The cortisol awakening response-normal values and confounds. Noise and health, 2(7), 79.
Acknowledgments
The authors are thankful to all volunteers for this study and to Federal University of Rio Grande do Norte, Brazil, for institutional support.
Author Agreement Statement
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
Funding
This study was funded by National Science and Technology Institute for Translational Medicine (INCT-TM Fapesp 2014/50891–1; CNPq 465458/2014–9). NLGC is supported by CAPES Foundation from Brazilian Ministry of Education (Research Fellowship 88887.466701/2019–00) National Science and Technology Institute for Translational Medicine (INCT-TM Fapesp 2014/50891–1; CNPq 465458/2014–9). The funder did not have any role in the design of the study, collection, analysis, and interpretation of data and in drafting the manuscript.
Author information
Authors and Affiliations
Contributions
NLGC, YMV and NGS planned the clinical trial; ACLL did volunteers screening; YMV conducted treatment; ACMG and GMSJ carried out statistical analysis; all authors contributed to the manuscript.
Corresponding author
Ethics declarations
Disclosure of Potential Conflicts of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
All procedures were approved by the ethical committee of the Federal University of Rio Grande do Norte, Brazil (#2628,202) and was in accordance with the 1964 Declaration of Helsinki, revised in 2008.
Consent to Participate
Participants became aware of the study procedures and provided informed written consent prior to participation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Varela, Y.M., de Almeida, R.N., Galvão, A.d. et al. Psychophysiological responses to group cognitive-behavioral therapy in depressive patients. Curr Psychol 42, 592–601 (2023). https://doi.org/10.1007/s12144-020-01324-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-020-01324-9