Abstract
Purpose
The prognostic value of Ki-67 in triple-negative breast cancer (TNBC) is yet unclear because the cut-off points employed differ widely and its predictive effect may vary according to age. The purpose of this study was to analyze the role of Ki-67 among patients with TNBC, and determine the optimal Ki-67 cut-off point to demonstrate its prognostic relevance associated with patient age and treatment strategy.
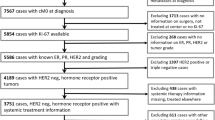
Methods/patients
201 consecutive patients treated for primary TNBC from 1999 to 2014 were analyzed. Clinicopathological characteristics and outcomes were compared between patients treated with neoadjuvant or adjuvant chemotherapy. We used time-dependent receiver operating characteristic (ROC) curve and time-dependent area under the ROC curve (AUC) to evaluate the discriminative ability of Ki-67 at 3 and 5 years of follow-up. A Ki-67 cut-off point that maximized sensibility and specificity was established. Interaction effect between age and Ki-67 on disease-free survival (DFS) and overall survival (OS) was evaluated by stratified analysis.
Results
According to the coordinates of the ROC curves, the best cut-off point for Ki-67 was 60% (high/low). In the whole group, there was not a statistically significant association between Ki-67 and OS and DFS, using a cut-off point of 60%. In multivariate analysis (COX proportional hazards regression), for DFS high Ki-67 (> 60%) was a poor prognostic factor in patients > 40 years old and a better prognostic factor among the patients < 40 years old.
Conclusion
Prognostic value of Ki-67 in TNBC, using a cut-off point of 60%, may vary depending on age.




Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC cancerbase no. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. http://globocan.iarc.fr.
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–81.
Dent R, Trudeau M, Pritchard K, Hanna WM, Hk Kahn, Sawkw CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;37:1–8.
Carey LA. Directed therapy of subtypes of triple-negative breast cancer. Oncologist. 2011;16(Suppl 1):71–8.
Rouzier R, Perou CM, Symmans WF, Ibraim N, Cristofanilli M, Anderson K, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11(16):5678–85.
Partridge AH, Hughes ME, Warner ET, Ottesen RA, Wong YN, Edge SB, et al. Subtype-dependent relationship between young age at diagnosis and breast cancer survival. J Clin Oncol. 2016;34(27):3308–14. https://doi.org/10.1200/JCO.2015.65.8013.
Radosa JC, Eaton A, Stempel M, Khander A, Liedke C, Solomayer EF, et al. Evaluation of local and distant recurrence patterns in patients with triple-negative breast cancer according to age. Ann Surg Oncol. 2016. https://doi.org/10.1245/s10434-016-5631-3.
Liedtke C, Hess KR, Karn T, Rody A, Kiesel L, Hortobagyi GN, et al. The prognostic impact of age in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2013;138(2):591–9. https://doi.org/10.1007/s10549-013-2461-x.
Sheridan W, Scott T, Caroline S, Yvonne Z, Vanesa B, David B, et al. Breast cancer in young women: have the prognostic implications of breast cancer subtypes changed over time? Breast Cancer Res Treat. 2014;147(3):617–29. https://doi.org/10.1007/s10549-014-3125-1.
Munzone E, Botteri E, Sciandivasci A, Cirigliano G, Nolè F, Mastropasqua M, et al. Prognostic value of Ki-67 labeling index in patients with node-negative, triple-negative breast cancer. Breast Cancer Res Treat. 2012;134(1):277–82. https://doi.org/10.1007/s10549-012-2040-6.
Hao S, He ZX, Yu KD, Yang WT, Shao ZM. New insights into the prognostic value of Ki-67 labeling index in patients with triple-negative breast cancer. Oncotarget. 2016;7(17):24824–31. https://doi.org/10.18632/oncotarget.8531.
Urruticoechea A, Smith IE, Dowsett M. Proliferation marker Ki-67 in early breast cancer. J Clin Oncol. 2005;23(28):7212–20.
Keam B, Sa Im, Lee KH, Han SW, Oh DY, Kim JH, et al. Ki-67 can be used for further classification of triple negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res. 2011;13:R22. https://doi.org/10.1186/bcr2834.
Wang W, Wu J, Zhang P, Fei X, Zong Y, Chen X, et al. Prognostic and predictive value of Ki-67 in triple-negative breast cancer. Oncotarget. 2016;7(21):31079–87. https://doi.org/10.18632/oncotarget.9075.
Mrklic I, Capkun V, Pogorelic Z, Tomic S. Prognostic value of Ki-67 proliferating index in triple negative breast carcinomas. Pathol Res Pract. 2013;209(5):296–301. https://doi.org/10.1016/j.prp.2013.02.012.
Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56:337–44.
Blanche P, Dartigues JF, Jacqmin-Gadda H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat Med. 2013;32:5381–97.
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, et al. Assessment of Ki-67 in breast cancer. recommendations from the international Ki-67 in breast cancer working group. J Natl Cancer Inst. 2011;103:1656–64.
Gnant M, Harbeck N, Thomssen C. St. Gallen 2011: summary of the consensus discussion. Breast Care (Basel). 2011;6(2):136–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare there is no conflict of interest.
Ethical approval
The study was approved by the Ethical Committee of HUFA. Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Informed consent
Informed consent was waived by the Clinical Research Ethics Committee because no intervention was involved and no patient identifying information was included.
Confidentiality of data
The authors declare that they have followed the protocols of their work centre on publication of patient data.
Financing
There is no source of funding.
Additional information
Zenzola and Cabezas-Quintario have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zenzola, V., Cabezas-Quintario, M.A., Arguelles, M. et al. Prognostic value of Ki-67 according to age in patients with triple-negative breast cancer. Clin Transl Oncol 20, 1448–1454 (2018). https://doi.org/10.1007/s12094-018-1877-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-1877-5