Abstract
Background
Patients with lower socioeconomic status (SES), ethnic minorities and elevated neutrophil–lymphocyte ratio (NLR) have been suggested to have worse outcomes in hepatocellular carcinoma (HCC). However, how changes in NLR after intervention relate to survival has not been elucidated.
Objectives
We evaluated the association of NLR with overall survival (OS) and progression-free survival (PFS) in a large institutional cohort of HCC.
Methods
We reviewed all patients diagnosed with HCC between 2005–2016. The association between elevated NLR (> 4) and survival was examined with univariable and multivariable Cox regression.
Results
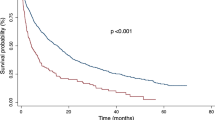
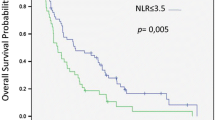
We identified 991 patients diagnosed with HCC. Lower SES and Hispanic and non-Hispanic Black ethnicity were significantly associated with lower NLR (p = 0.015 and 0.019, respectively). Elevated NLR, but not SES or ethnicity, was an independent predictor of worse OS (HR = 1.66, p < 0.001) and PFS (HR = 1.25, p = 0.032). The median OS in patients with elevated NLR was 8 months, compared to 42 months in patients with normal NLR. Patients with elevated NLR unresponsive to treatment and those with NLR that became elevated after treatment had significantly worse 3-year OS (47% and 44%, respectively), compared to patients whose NLR remained normal or normalized after treatment (72% and 80%, respectively; p < 0.01).
Conclusions
Our study showed that elevated NLR, but not SES or ethnicity, is an independent prognostic marker for OS and PFS in patients with HCC. NLR trends following intervention were highly predictive of outcome. NLR is easy to obtain and would provide valuable information to clinicians in evaluating prognosis and monitoring response after procedures.


Similar content being viewed by others
References
Cancer Facts & Figures 2019. American Cancer Society. 2019.
El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365(12):1118–27.
Jaiswal M, LaRusso NF, Burgart LJ, Gores GJ. Inflammatory cytokines induce DNA damage and inhibit DNA repair in cholangiocarcinoma cells by a nitric oxide-dependent mechanism. Can Res. 2000;60(1):184–90.
Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15(2):425–30.
Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res BCR. 2017;19(1):2.
Sharaiha RZ, Halazun KJ, Mirza F, Port JL, Lee PC, Neugut AI, et al. Elevated preoperative neutrophil:lymphocyte ratio as a predictor of postoperative disease recurrence in esophageal cancer. Ann Surg Oncol. 2011;18(12):3362–9.
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005;91(3):181–4.
Shimada H, Takiguchi N, Kainuma O, Soda H, Ikeda A, Cho A, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer. 2010;13(3):170–6.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Fushiya N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107(6):988–93.
Sullivan KM, Groeschl RT, Turaga KK, Tsai S, Christians KK, White SB, et al. Neutrophil-to-lymphocyte ratio as a predictor of outcomes for patients with hepatocellular carcinoma: a Western perspective. J Surg Oncol. 2014;109(2):95–7.
Shen Y, Guo H, Wu T, Lu Q, Nan KJ, Lv Y, et al. Lower education and household income contribute to advanced disease, less treatment received and poorer prognosis in patients with hepatocellular carcinoma. J Cancer. 2017;8(15):3070–7.
Wang S, Sun H, Xie Z, Li J, Hong G, Li D, et al. Improved survival of patients with hepatocellular carcinoma and disparities by age, race, and socioeconomic status by decade, 1983–2012. Oncotarget. 2016;7(37):59820–33.
Jones PD, Diaz C, Wang D, Gonzalez-Diaz J, Martin P, Kobetz E. The impact of race on survival after hepatocellular carcinoma in a diverse American population. Dig Dis Sci. 2018;63(2):515–28.
Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS ONE. 2014;9(11):e112361.
Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124.
Aparo S, Goel S, Lin D, Ohri N, Schwartz JM, Lo Y, et al. Survival analysis of hispanics in a cohort of patients with hepatocellular carcinoma. Cancer. 2014;120(23):3683–90.
Tran PN, Taylor TH, Klempner SJ, Zell JA. The impact of gender, race, socioeconomic status, and treatment on outcomes in esophageal cancer: a population-based analysis. J Carcinog. 2017;16:3.
Svennevig JL, Lunde OC, Holter J, Bjorgsvik D. Lymphoid infiltration and prognosis in colorectal carcinoma. Br J Cancer. 1984;49(3):375–7.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Ohtani H. Focus on TILs: prognostic significance of tumor infiltrating lymphocytes in human colorectal cancer. Cancer Immun. 2007;7:4.
Chen TM, Lin CC, Huang PT, Wen CF. Neutrophil-to-lymphocyte ratio associated with mortality in early hepatocellular carcinoma patients after radiofrequency ablation. J Gastroenterol Hepatol. 2012;27(3):553–61.
Ridker PM, MacFadyen JG, Thuren T, Everett BM, Libby P, Glynn RJ, et al. Effect of interleukin-1beta inhibition with canakinumab on incident lung cancer in patients with atherosclerosis: exploratory results from a randomised, double-blind, placebo-controlled trial. Lancet. 2017;390(10105):1833–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yifei Zhang, N. Patrik Brodin, Nitin Ohri, Santiago Thibaud, Andreas Kaubisch, Milan Kinkhabwala, Madhur Garg, Chandan Guha and Rafi Kabarriti declare that they have no conflict of interest.
Ethical approval
The study protocol has been approved by the institute’s committee on human research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Brodin, N.P., Ohri, N. et al. Association between neutrophil–lymphocyte ratio, socioeconomic status, and ethnic minority with treatment outcome in hepatocellular carcinoma. Hepatol Int 13, 609–617 (2019). https://doi.org/10.1007/s12072-019-09965-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09965-0