Abstract
Background and aims
Doubts have been raised about efficacy of New Wilson’s index (NWI) in predicting Liver Transplant (LT) or mortality in decompensated Wilson Disease (WD) patients. APASL ACLF Research Consortium (AARC) has introduced a new score (AARC-ACLF) which has not been studied in children.
Methods
Data of all pediatric WD cases were prospectively collected and analyzed. Cox regression and Area Under Receiver Operative Curve (AUROC) analyses were used to identify best predictive score for mortality at 90 days.
Results
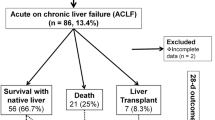
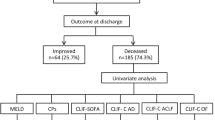
Sixty-six confirmed cases of decompensated WD, 39 (59%) improved on medical management and 27 (41%) either died (20) or were transplanted (7). Among those with NWI ≥ 11 (42/66 cases) 19 survived versus those with NWI < 11 (24/66), 4 died. NWI (HR 1.23, 95% CI 1.07–1.42, p = 0.005), AARC-ACLF (HR 1.66, 95% CI 1.34–2.05, p = 0.000) and Chronic Liver Failure-Sequential Organ Failure Assessment score also known as CLIF–SOFA (HR 1.31, 95% CI 1.13–1.50, p = 0.000) were all significantly associated with death on univariate Cox regression analysis. On comparative evaluation of the predictive scores in the present cohort, the highest positive (6.02) and lowest negative (0.09) likelihood ratios as well as highest accuracy (87.88%) revealed AARC-ACLF as the best predictor of mortality. AARC-ACLF had the best predictability with AUROC of 0.939 and the minimum standard error of 0.027. For every unit increase in AARC-ACLF score, there is likelihood of 66% increase in 90 day mortality. The optimal cutoff for the AARC-ACLF score to predict mortality was 11 or more.
Conclusion
AARC-ACLF is the best score for the prediction of mortality at 90 days in decompensated WD cases.




Similar content being viewed by others
References
Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML. Wilson’s disease. Lancet. 2007;369:397–408.
Nazer H, Ede RJ, Mowat AP, Williams R. Wilson’s disease: clinical presentation and use of prognostic index. Gut. 1986;27:1377–81.
Dhawan A, Taylor RM, Cheeseman P, De Silva P, Katsiyiannakis L, Mieli-Vergani G. Wilson’s disease in children: 37-year experience and revised King’s score for liver transplantation. Liver Transpl. 2005;11:441–8.
Fischer RT, Soltys KA, Squires RHJ, Jaffe R, Mazariegos GV, Shneider BL. Prognostic scoring indices in Wilson disease: a case series and cautionary tale. J Pediatr Gastroenterol Nutr. 2011;52:466–9.
Devarbhavi H, Singh R, Adarsh CK, Sheth K, Kiran R, Patil M. Factors that predict mortality in children with Wilson disease associated acute liver failure and comparison of Wilson disease specific prognostic indices. J Gastroenterol Hepatol. 2014;29(2):380–6.
Alam S, Lal BB, Sood V, Rawat D. Pediatric Acute-on-Chronic Liver Failure in a Specialized Liver Unit: prevalence, Profile, Outcome, and Predictive Factors. J Pediatr Gastroenterol Nutr. 2016;63(4):400–5.
Lal J, Thapa BR, Rawal P, Ratho RK, Singh K. Predictors of outcome in acute-on-chronic liver failure in children. Hepatol Int. 2011;5(2):693–7.
Jagadisan B, Srivastava A, Yachha SK, Poddar U. Acute on chronic liver disease in children from the developing world: recognition and prognosis. J Pediatr Gastroenterol Nutr. 2012;54(1):77–82.
Lal BB, Alam S, Sood V, Rawat D, Khanna R. Profile, risk factors and outcome of acute kidney injury in paediatric acute-on-chronic liver failure. Liver Int. 2018;38(10):1777–84.
Lal BB, Sood V, Khanna R, Alam S. How to identify the need for liver transplantation in pediatric acute-on-chronic liver failure? Hepatol Int 2018. https://doi.org/10.1007/s12072-018-9901-y [Ahead of print].
Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Gine`s P, For CANONIC study investigators of the EASL-CLIF Consortium, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol 2014;61(5):1038–1047.
Choudhury A, Jindal A, Maiwall R, Sharma MK, Sharma BC, Pamecha V, et.al; APASL ACLF Working Party. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int 2017;11(5):461-471.
Ferenci P, Caca K, Loudianos G, Mieli-Vergani G, Tanner S, Sternlieb I, et al. Diagnosis and phenotypic classification of Wilson disease. Liver Int. 2003;23:139–42.
Atterbury CE, Maddrey WC, Conn HO. Neomycin-sorbitol and lactulose in the treatment of acute portal-systemic encephalopathy. A controlled, double-blind clinical trial. Am J Dig Dis. 1978; 23: 398–406.
Sarin SK, Kedarisetty CK, Abbas Z, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol Int. 2014;8(4):453–71.
Socha P, Janczyk W, Dhawan A Baumann U, D’Antiga L, Tanner S, et al. Wilson’s Disease in Children: A Position Paper by the Hepatology Committee of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;66(2):334-344.
Agrawal S, Duseja A, Gupta T, Dhiman RK, Chawla Y. Simple organ failure count versus CANONIC grading system for predicting mortality in acute-on-chronic liver failure. J Gastroenterol Hepatol. 2015;30(3):575–81.
Bolia R, Srivastava A, Yachha SK, Poddar U. Pediatric CLIF-SOFA score is the best predictor of 28-day mortality in children with decompensated chronic liver disease. J Hepatol. 2018;68(3):449–55.
Petrasek J, Jirsa M, Sperl J, Kozak L, Taimr P, Spicak J, et al. Revised King’s College score for liver transplantation in adult patients with Wilson’s disease. Liver Transpl. 2007;13:55–61.
Squires RH Jr, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006;148(5):652–8.
Kathemann S, Bechmann LP, Sowa JP, Manka P, Dechêne A, Gerner P, et al. Etiology, outcome and prognostic factors of childhood acute liver failure in a German Single Center. Ann Hepatol. 2015;14(5):722–8.
Tian Y, Gong GZ, Yang X, Peng F. Diagnosis and management of fulminant Wilson’s disease: a single center’s experience. World J Pediatr. 2016;12(2):209–14.
Kaur S, Kumar P, Kumar V, Sarin SK, Kumar A. Etiology and prognostic factors of acute liver failure in children. Indian Pediatr. 2013;50(7):677–9.
Pediatric Gastroenterology Chapter of Indian Academy of Pediatrics, Bhatia V, Bavdekar A, Yachha SK; Indian Academy of Pediatrics. Management of acute liver failure in infants and children: consensus statement of the pediatric gastroenterology chapter, Indian academy of pediatrics. Indian Pediatr. 2013;50(5):477-82.
Alam S, Khanna R, Sood V, Lal BB, Rawat D. Profile and outcome of first 109 cases of paediatric acute liver failure at a specialized paediatric liver unit in India. Liver Int. 2017;37(10):1508–14.
Kegley KM, Sellers MA, Ferber MJ, Johnson MW, Joelson DW, Shrestha R. Fulminant Wilson’s disease requiring liver transplantation in one monozygotic twin despite identical genetic mutation. Am J Transplant. 2010;10(5):1325–9.
Kido J, Matsumoto S, Momosaki K, Sakamoto R, Mitsubuchi H, Inomata Y, et al. Plasma exchange and chelator therapy rescues acute liver failure in Wilson disease without liver transplantation. Hepatol Res. 2017;47(4):359–63.
Lee BH, Kim JH, Lee SY, Jin HY, Kim KJ, Lee JJ, et al. Distinct clinical courses according to presenting phenotypes and their correlations to ATP7B mutations in a large Wilson’s disease cohort. Liver Int. 2011;31:831–9.
Verma N, Pai G, Hari P, Lodha R. Plasma exchange for hemolytic crisis and acute liver failure in Wilson disease. Indian J Pediatr. 2014;81(5):498–500.
Akyildiz BN, Yildirim S, Kondolot M, Arslan D. Is plasma exchange effective in prevention of hepatic transplantation in fulminant Wilson disease with hepatic failure? J Pediatr Gastroenterol Nutr. 2011;52(6):778–80.
Piersma FE, Tanner S, Socha P et al. Controversies in diagnosing and treating Wilson disease in children—results of an international survey. Hepatology 2012; 56 (Suppl.):731A.
Santos Silva EE, Sarles J, Buts JP, et al. Successful medical treatment of severely decompensated Wilson disease. J Pediatr. 1996;128:285–7.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Seema Alam, Bikrant Bihari Lal, Vikrant Sood, Rajeev Khanna, and Guresh Kumar declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This was a retrospective study. The study was approved by the institutional ethical review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alam, S., Lal, B.B., Sood, V. et al. AARC-ACLF score: best predictor of outcome in children and adolescents with decompensated Wilson disease. Hepatol Int 13, 330–338 (2019). https://doi.org/10.1007/s12072-019-09938-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09938-3