Abstract
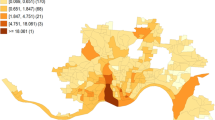
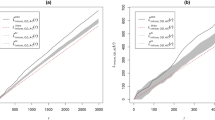
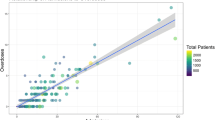
Using a combination of data derived from the U.S. Census Bureau, the Substance Abuse and Mental Health Service Administration’s Behavioral Health Systems Locator and the Boston Police Department’s Incident Reports, this study examines the spatio-temporal distribution of calls for medical assistance following a heroin-related injury between 2015 and 2018. As well, an examination is conducted regarding the accessibility of Health Care Centers (HCCs) in relation to individuals in need of medical assistance. Distance-based measures of spatial association, including nearest neighbor and K-function analysis, were used to determine the clustering of calls at various spatial scales. Structural neighborhood characteristics (i.e., distance to the closest HCC) and physical and social vulnerability were used to predict the rate of calls for a heroin-related injury per 1,000 persons in the city of Boston using a spatial autoregressive model. HCC catchment areas for the set of medical emergency calls were created using Voronoi tessellations. Results showed that the average nearest neighbor distance (NND) of each call for medical assistance was approximately 187 m or .12 miles. Calls for assistance became more probable and increasingly more spatially concentrated over the study period. The K-function analysis revealed that the calls clustered at different spatial scales and in proximity to HCCs. Average distance to the nearest HCC and Household/Disability vulnerability were significantly associated with the census tract call rate per 1,000 persons. The average travel distance between the calls for medical assistance and the nearest HCC was 941 m, or just over a half-mile. Policy implications for the provision, through HCCs, of a focused and comprehensive community-based support system in a large urban city for individuals with serious drug problems are discussed in context.









Similar content being viewed by others
Notes
The code is available at https://github.com/Robinlovelace/Creating-maps-in-R/blob/master/vignettes/clustersG.R
Spatstat does not provide the ability to perform such calculations however Mathew Peeples graciously provided the code necessary to perform this analysis (see http:\\www.mattpeeples.net).
References
Annual Surveillance Report of Drug-Related risks and Outcomes (2017). Atlanta: Centers for Disease Control and Prevention; 31 Aug 2017 [accessed 29 Jun 2019].
Adrian Baddeley, Ege Rubak, Rolf Turner (2015). Spatial point patterns: Methodology and applications with R. London: Chapman and Hall/CRC Press, 2015. URL http://www.crcpress.com/Spatial-Point-Patterns-Methodology-and-Applications-with-R/Baddeley-Rubak-Turner/9781482210200/. Accessed June 2019.
Arcury, T. A., Preisser, J. S., Gesler, W. M., & Powers, J. M. (2005). Access to transportation and health care utilization in a rural region. The Journal of Rural Health, 21(1), 31–38.
Barnard, M., & McKeganey, N. (2004). The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction, 99(5), 552–559.
Bevan, A., & Lake, M. (2016). Intensities, interactions, and uncertainties: Some new approaches to archaeological distributions Computational approaches to archaeological spaces (pp. 27–52): Routledge.
Choate, C. (2015). A Spatial Statistical Analysis of the Effect of Gentlemen's Clubs on Crime in the City of Los Angeles(doctoral dissertation, California State University, Northridge).
Ciccarone D. (2018) The triple wave epidemic: Opioids, heroin and fentanyl: Supply issues and public health consequences. Before the committee on foreign affairs, subcommittee on Africa, Global Health, global human rights, and international organizations, United sates house of representatives. Hearing: Tackling fentanyl: The China connection September 6.
Cooper, H. L., Bossak, B., Tempalski, B., Des Jarlais, D. C., & Friedman, S. R. (2009). Geographic approaches to quantifying the risk environment: Drug-related law enforcement and access to syringe exchange programmes. International Journal of Drug Policy, 20(3), 217–226.
de Montigny, L., Moudon, A. V., Leigh, B. C., & Kim, S.-Y. (2011). A spatial analysis of the physical and social environmental correlates of discarded needles. Health & Place, 17(3), 757–766.
DeBeck, K., Kerr, T., Bird, L., Zhang, R., Marsh, D., Tyndall, M., … & Wood, E. (2011). Injection drug use cessation and use of North America's first medically supervised safer injecting facility. Drug and Alcohol Dependence, 113(2–3), 172–176.
Donovan, R. J., Jancey, J., & Jones, S. (2002). Tobacco point of sale advertising increases positive brand user imagery. Tobacco Control, 11(3), 191–194.
Egunjobi, L. (1983). Factors influencing choice of hospitals: A case study of the northern part of Oyo state, Nigeria. Social Science & Medicine, 17(9), 585–589.
Flanagan, B. E., Gregory, E. W., Hallisey, E. J., Heitgerd, J. L., & Lewis, B. (2011). A social vulnerability index for disaster management. Journal of homeland security and emergency management, 8(1).
Fulcher, C., & Kaukinen, C. (2005). Mapping and visualizing the location HIV service providers: An exploratory spatial analysis of Toronto neighborhoods. AIDS Care, 17(3), 386–396.
Guerrero, E. G., Kao, D., & Perron, B. E. (2013). Travel distance to outpatient substance use disorder treatment facilities for Spanish-speaking clients. International Journal of Drug Policy, 24(1), 38–45.
HABIB, O. S., & Vaughan, J. (1986). The determinants of health services utilization in southern Iraq: A household interview survey. International Journal of Epidemiology, 15(3), 395–403.
Hembree, C., Galea, S., Ahern, J., Tracy, M., Piper, T. M., Miller, J., … Tardiff, K. J. (2005). The urban built environment and overdose mortality in new York City neighborhoods. Health & Place, 11(2), 147–156.
Latkin, C. A., Williams, C. T., Wang, J., & Curry, A. D. (2005). Neighborhood social disorder as a determinant of drug injection behaviors: A structural equation modeling approach. Health Psychology, 24(1), 96.
LaVeist, T. A., & Wallace, J. M., Jr. (2000). Health risk and inequitable distribution of liquor stores in African American neighborhood. Social Science & Medicine, 51(4), 613–617.
Lovelace, R. (2017). Creating Maps in R. Available at https://github.com/Robinlovelace/Creating-maps-in-R. Last Accessed August 5, 2019.
Manchikanti, L., Fellows, B., Janata, J. W., Pampati, V., Grider, J. S., & Boswell, M. V. (2012). Opioid epidemic in the United States. Pain Physician, 15(3 Suppl), ES9–E38.
Marshall, B. D., Milloy, M. J., Wood, E., Montaner, J. S., & Kerr, T. (2011). Reduction in overdose mortality after the opening of North America's first medically supervised safer injecting facility: A retrospective population-based study. The Lancet, 377(9775), 1429–1437.
Martinez, A. N., Lorvick, J., & Kral, A. H. (2014). Activity spaces among injection drug users in San Francisco. International Journal of Drug Policy, 25(3), 516–524.
Massachusetts Department of Public Health. (2017). An Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts (2011 – 2015). August, 2017. Available at https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Last Accessed June 29, 2019.
Massachusetts Department of Public Health (2019). MA Opioid-Related EMS Incidents 2013-September 2018. Available online https://www.mass.gov/files/documents/2019/02/12/Emergency-Medical-Services-Data-February-2019.pdf. Last Accessed August 5, 2019.
Moore, A., & Carpenter, T. (1999). Spatial analytical methods and geographic information systems: Use in health research and epidemiology. Epidemiologic Reviews, 21(2), 143–161.
National Academies of Sciences. (2017). Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse; Phillips JK, Ford MA, Bonnie RJ, editors. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington (DC): National Academies Press (US); 2017 Jul 13. 4, Trends in Opioid Use, Harms, and Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK458661/
National Institute on Drug Abuse (2017). National overdose deaths from select pre-scription and illicit drugs, Data sourced from the Centers for Disease Control accessed on May 17, 2019. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
Ndumele, C. D., Russell, B. E., Ayanian, J. Z., Landon, B. E., Keegan, T., O'Malley, A. J., & Hicks, L. S. (2009). Strategies to improve chronic disease management in seven metro Boston community health centers. Progress in Community Health Partnerships: Research, Education, and Action, 3(3), 203.
Phillips, J. K., Ford, M. A., & Bonnie, R. J. (2017). Trends in opioid use, harms, and treatment. Washington, DC: National Academies Press (US).
Pilon, D., Tandon, N., Lafeuille, M. H., Kamstra, R., Emond, B., Lefebvre, P., & Joshi, K. (2017). Treatment patterns, health care resource utilization, and spending in Medicaid beneficiaries initiating second-generation long-acting injectable agents versus oral atypical antipsychotics. Clinical Therapeutics, 39(10), 1972–1985.
Rowe, C., Santos, G.-M., Vittinghoff, E., Wheeler, E., Davidson, P., & Coffin, P. O. (2016). Neighborhood-level and spatial characteristics associated with lay naloxone reversal events and opioid overdose deaths. Journal of Urban Health, 93(1), 117–130.
Sherman, L. W., Gartin, P. R., & Buerger, M. E. (1989). Hot spots of predatory crime: Routine activities and the criminology of place. Criminology, 27(1), 27–56.
Stopka, T. J., Lutnick, A., Wenger, L. D., DeRiemer, K., Geraghty, E. M., & Kral, A. H. (2012). Demographic, risk, and spatial factors associated with over-the-counter syringe purchase among injection drug users. American Journal of Epidemiology, 176(1), 14–23.
Tobin, K. E., Davey, M. A., & Latkin, C. A. (2005). Calling emergency medical services during drug overdose: An examination of individual, social and setting correlates. Addiction, 100(3), 397–404.
Van der Stuyft, P., Sorensen, S. C., Delgado, E., & Bocaletti, E. (1996). Health seeking behaviour for child illness in rural Guatemala. Tropical Medicine & International Health, 1(2), 161–170.
Warner, B. D., & Pierce, G. L. (1993). Reexamining social disorganization theory using calls to the police as a measure of crime. Criminology, 31(4), 493–517.
Weitzman, E. R., Nelson, T. F., & Wechsler, H. (2003). Taking up binge drinking in college: The influences of person, social group, and environment. Journal of Adolescent Health, 32(1), 26–35.
Zalkind, S. (2017). The Infrastructure of the Heroin Epidemic. Available at https://www.citylab.com/equity/2017/09/methadone-mile/539742/. Last Accessed August 5, 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barboza, G.E. A Spatiotemporal Analysis of Heroin-Related Calls for Emergency Medical Services and Community-Health Centers in Boston, Massachusetts. Appl. Spatial Analysis 13, 507–525 (2020). https://doi.org/10.1007/s12061-019-09315-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12061-019-09315-5