Abstract
Purpose
On-pump beating-heart coronary artery bypass grafting represents a merger of standard on and off-pump techniques and is thought to benefit patients by coupling the dual absence of cardioplegic arrest (conventional coronary surgery), with the hemodynamic instability during manipulation seen in off-pump surgery. However, the clinical benefits are still under discussion. We improvised on the standard on-pump beating-heart surgeries by introducing use of “intermittent” bypass as and when required.
Methods
This study involved 108 patients. “Intermittent” on-pump-beating heart coronary artery bypass grafting was done using suction stabilizer and placing aortic and venous cannula, electively in all patients (group 1) who were supported by pump intermittently (n = 54). Retrospective data of patients who underwent off-pump surgery electively by the same surgeon (group 2, n = 54) was collected.
Results
There was a significant advantage in the number of grafts performed for the lateral surface (circumflex branches) using the new technique compared to conventional technique (68vs22). Similarly, significant advantage was also noted in terms of total number of grafts along with shorter operating times. There were no mortalities in the new group compared to the off-pump group and blood loss was also lesser.
Conclusions
“Intermittent” on-pump coronary revascularization is a technically reliable method of coronary revascularization taking advantage of the off-pump and conventional on-pump techniques while considerably eliminating the disadvantages of both. It has shown its superiority in safety, number of grafts, blood loss, operating time and perioperative course.
Similar content being viewed by others
Introduction
The morbidities of conventional coronary artery bypass grafting (C-CABG) have been attributed to the use of cardiopulmonary bypass (CPB) which has shown to be associated with systemic inflammatory response owing to the exposure of the blood to large foreign body surfaces. This has also shown to cause reperfusion injuries to the lungs and heart. It is also a well-known fact that once the heart is arrested, although being protected by cardioplegia of different kinds, there is still some extent of myocardial ischemia and a temporary decline in cardiac function. For this reason, the development of off-pump coronary artery bypass grafting (OPCAB) met a high popularity among surgeons and patients because it served to eliminate the harmful effects of the heart-lung machine and the need for cardioplegic arrest. Understandably, a lot of clinical, pharmaceutical, and biochemical trials have been undertaken to study the outcomes of OPCAB. Although the OPCAB technique has shown to reduce the mortality and morbidity in high-risk patients by eliminating the use of CPB and cardioplegic arrest, it has been also shown that hemodynamic instability and malignant arrhythmias could occur during the surgical manipulation and heart displacement for exposure of target coronary arteries and distal anastomoses. These technical difficulties are believed to be the leading cause of incomplete or suboptimal revascularization which is attributed to the OPCAB technique.
A newer technique which eliminates the disadvantages of, while preserving the advantages of both the on- and off-pump coronary artery bypass grafting (CABG) is the on-pump beating-heart CABG (ON-BH CABG) under normo-thermic CPB. This represents a merger of standard on-pump and off-pump CABG techniques, offering greater benefits to high-risk patients by coupling the dual absence of intraoperative global myocardial ischemia from cardioplegic arrest (occurring during C-CABG) with the hemodynamic instability guaranteed during extensive heart manipulation (as in OPCAB) and thus could be described as an acceptable trade-off in high-risk patients [1].
Although several studies have reported the advantage of ON-BH CABG in high-risk patients, the clinical benefits of ON-BH CABG are still under discussion.
Aims and objectives
We began this study already knowing the extensive research into the risks and benefits of off-pump vs on-pump surgeries as well as the recently introduced on-pump-beating heart surgeries and their benefits. However, we tried to further improvise on the ON-BH surgeries by introducing “intermittent on pump beating heart CABG” using CPB as and when required. Our aim was to study the early outcomes and benefits of this technique against the standard established techniques.
Methods
This study was conducted in patients who underwent CABG from January 2015 to October 2016. This was a bidirectional observational study involving 108 patients. During this period, we introduced a new technique of “Intermittent On pump beating heart CABG” using suction stabilizer and placing aortic and venous cannula, electively in all patients consecutively on the list. These patients were supported by pump intermittently, as and when required thus forming group 1 (n = 54). Retrospectively, we similarly obtained data from 54 consecutive patients in the past who underwent OPCAB electively by the same surgeon (group 2, n = 54) going back through the operating list. As the prospective arm was not randomized but rather a consecutive list, the retrospective arm was chosen in a similar fashion. Antiplatelet therapy (aspirin and/or clopidogrel) was discontinued at least 04 days prior to the surgery.
Inclusion criteria
All patients scheduled for isolated OPCAB retrospectively, or for isolated ON-BH CABG during the study period.
Exclusion criteria
Patients undergoing combined procedures involving CABG (valves, carotid endarterectomies, etc.), emergency surgery, or those with congenital or acquired platelet/clotting disorders.
The demographic data, risk factors, echocardiographic and angiographic findings, blood investigations, coagulation profiles, and perioperative and postoperative data including CK-MB, Trop I, NT-Pro BNP, and CRP preoperatively, at 24 and 48 h were recorded which are as such routinely done at our institution. Standard anesthesia techniques were used for induction and maintenance. After standard internal mammary artery takedown, anticoagulation was achieved using heparin (3 mg/kg) to achieve an ACT of more than 480 s. After completion of anastomosis, protamine was given in all the patients.
Statistical methods
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical Analysis Software. The values were represented in number (%) and mean ± SD.
The following statistical formulas were used:
-
1.
Mean
-
2.
Standard deviation
-
3.
Median
-
4.
Chi square test
-
5.
Student’s t test
-
6.
Level of significance
Results
The overall mean age of patients was 56.44 + 8.29 years and the ages were statistically matched in both groups. Gender difference was also not found to be significant although overall 16.67% of the total patients were females and 83.33% were males. Hypertension was the commonest comorbidity (88.89%) followed by hypercholesterolemia, smoking, and diabetes. This data along with the distribution in coronary disease anatomy is represented in Table 1.
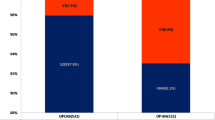
Operative data is depicted in Table 2 which shows that there was a significant advantage in the number of grafts done for the lateral surface (circumflex branches) in group 1 compared to group 2 (68 vs 22). This difference was found to be highly significant (p < 0.001). Similarly, a high significant advantage was also noted in group 1 patients in terms of total number of graft (3.31 ± 1.16 vs 2.30 ± 0.66) and mean operating time—i.e., beginning of internal mammary artery harvesting after sternotomy to completion of all anastomosis—(1.37 ± 0.23 h vs 2.22 ± 0.45 h), where p value was < 0.001. We also noted a CPB time of less than 15 min in the majority of group 1 patients (70.37%) with a mean of 16.81 min. CPB was required particularly during grafting of lateral vessels and was used intermittently when required.
Table 3 shows the postoperative data. There was no significant difference in the usage of postoperative ionotropic support, duration of ventilation, ICU stay, arrhythmias, neurological or renal events, or requirement of intra-aortic balloon pump. However, blood loss in the first group was constantly less than in the second group (406.30 ± 257.90 ml vs 567.41 ± 265.20 ml), and although the difference was about 160 ml only, it was significant statistically. There was no mortality associated with group 1 patients while there were four deaths in group 2.
Changes in blood/serum values before and after surgery for each group are shown in Table 4. The mean hemoglobin of patients of group I (10.05 + 1.53 g/dl) was found to be significantly higher than that of group II (9.06 + 1.22 g/dl) after 48 h of surgery and can be correlated to the lesser amount of blood loss in the first group. At 48 h post operatively, mean CK-MB of patients of group I (11.98 + 13.96 g/dl) was found to be higher than that of group II (5.98 + 3.39 g/dl) (p = 0.038). Similarly, the Trop-I values of patients of group I (0.85 + 1.52 units) was higher than that of group II (0.17 + 0.10 units) (p = 0.028). Additionally, the mean CRP values of patients of group I (118.35 + 27.08 mg/L) was found to be significantly higher than that of group II (57.23 + 14.18 mg/l) (p < 0.001) in conjunction with the mean NT-pro BNP which showed a similar pattern.
Discussion
This article describes our experience with intermittently using pump during beating heart CABG, as and when required and is technically a new and different strategy compared to other studies describing ON-BH CABGs which use CPB throughout the procedure.
The morbidities of C-CABG have been attributed to the use of CPB, cardioplegic arrest, and aortic cross clamping resulting in ischemia and reperfusion injury. The development of classical OPCAB served to eliminate these harmful effects of CPB, and, hence, using the OPCAB technique for multi-vessel myocardial revascularization in high-risk patients was believed to significantly reduce the incidence of perioperative MI and other major complications, ICU stay, and mortality [2]. Despite the fact that the initial results with OPCAB were reported to be positive, more recent studies have shown a less favorable outcome after OPCAB, for example, a meta-analysis of 22 studies, enrolling a total of > 100,000 patients, showed that C-CABG had better long-term survivals compared to OPCABG [3]. Furthermore, there are more adverse outcomes after emergency conversions from OPCAB to C-CABG [4].
For this reason, ON-BH CABGs have been described as an acceptable trade-off in high-risk patients preventing the hemodynamic compromise of OPCAB as well as reducing CPB, cross clamp, and cardioplegia associated outcomes of classical C-CABG. [1]. This therefore leads to better myocardial protection compared to the obligatory pan myocardial ischemia of C-CABG intraoperatively [5, 6]. Subsets of patients who have low cardiac functions and reserves as well as those who present with acute ischemia for emergency surgeries, may be vulnerable to the ischemia of C-CABG or to the extensive traction of the heart during OPCAB and, thus, ON-BH CABG can be a promising alternative for these patients. [7,8,9,10].
Surgically, the ON-BH CABG technique proposes to offer a more stable field for quality anastomosis when compared to the OPCAB technique because cardiac perfusion is maintained while at the same time, over distension of the heart is prevented [11,12,13]. Due to theoretical uncertainties regarding the ON-BH CABG technique, interest in this has not been significant and hence studies are scarce when we compare the other two strategies. For example in a recent study in 2018 by Dayan et al., it was concluded that both ON-BH CABG and C-CABG where similar in terms of long-term survival rates and operative mortalities [14]. While higher rates of prolonged ventilator support and blood sugar levels were seen in ON-BH CABG, C-CABG was associated with a higher need of longer inotropic support. As a conclusion, both these techniques scored even and the decision rested upon the surgeon to choose the most appropriate technique. Another new study showed that the use of CPB support makes ON-BH CABG technically similar to C-CABG, and there were no obvious clear differences between these two strategies either short or long term [15]. We would like to state here that it should be however considered that technically and biochemically, ON-BH CABG differs from classical C-CABG in that there is no aortic cross clamping, rendering the procedure more physiological.
Technically, during ON-BH CABG, the feasibility of grafting the branches of the circumflex artery is better because the heart volume is significantly lessened. Utilizing heart stabilizers (in the same manner as in OPCABs), wider exposure in the posterolateral fields of the heart can be obtained while the heart is beating, and although this exposure of the heart happens at the cost of extreme upward retraction potentially liable to cause myocardial compromise, reasonable myocardial protection is offered by on-pump beating-heart technique [16]. Our study also showed that there was an advantage gained by our technique when it came to the number of lateral branches revascularized. Comparing distal anastomosis between the two groups in our study, there were no significant differences in the left anterior descending and right coronary artery as target vessels between the two groups, while the difference in proportion of patient in whom distal anastomosis on circumflex was done in group I (77.78%) and group II (22.22%) was found to be significant (p < 0.001). Similarly, the proportion of patients with distal anastomosis done on the diagonal branches was significantly higher in group I (29.63%) when compared to group II (3.70%).
Traditionally, it was held that OPCAB is inferior to C-CABG in terms of the number of grafts performed, but with the passage of time and perfection of techniques, many studies showed OPCAB to be equivalent to C-CABG in this aspect [17]. Our center has been performing OPCAB surgeries nearly electively for all patients with good outcomes since the last decade 1. C-CABG was done when other concomitant surgery is also planned or for emergencies. Thus, in terms of technical feasibility of OPCAB even in difficult lesions, beating heart surgery is our center’s first choice. We however did encounter difficult situations in extreme manipulation of the heart in some of our previous cases, and this prompted us to undertake using intermittent CPB support, with beating heart to study and see whether there would be better outcomes compared to OPCAB alone, in elective patients.
Our study showed that number of grafts used in the majority of the study patients in group I (74.07%) were 3–4 and were significantly higher (p < 0.001) than those in group II where majority of the patients (88.89%) were served with 2–3 grafts. The use of CPB obviously necessitated cannulation and preparation for bypass. This however was nothing more than an addition of a routine basic procedure, and, moreover, it was seen that the operating time was significantly longer (p < 0.001) in group II (2.22 + 0:45 h) as compared to group I (1.37 + 0.23 h). There was thus an advantage gained over the OPCAB group particularly when difficult positioning and bad coronary anatomy necessitates more attention to detail and caution during completion of distal anastomosis particularly in vulnerable hearts during OPCAB. Utilizing intermittent ON-BH CABG on the other hand made these stretches of time-consuming difficult grafts more feasible and technically more sound with less risk of any adverse threat to the cardiac function.
The postoperative data collected for the ON-BH CABG group in our study has suggested better clinical results than do those for the OPCAB group. There was no mortality associated with group 1 patients while there were four deaths in group 2. Additionally, postoperative bleeding in group II was 567.41 + 267.73 ml which was significantly higher as compared to group I (406.30 + 260.37 ml). There was no significant difference in the usage of postoperative ionotropic support though the average duration of ionotrope usage was more in group 2. Although more number of patients in group 1 required prolonged ventilation (24 vs 18 in group 2), the duration of ventilation was not significant. Length of ICU stay and arrhythmias were more in the OPCAB group along with nonsignificant higher renal events and requirement of intra-aortic balloon pump perioperatively.
There was conversion of four cases of OPCAB into ON-BH CABG. During surgery, conversion from OPCAB to CABG-CPB occurs occasionally. The common factors leading to conversions which often may be unanticipated, poor coronary anatomy and extensive coronary and myocardial disease and scarring, tachy or brady arrhythmias, hemodynamically frail cardiac function and wall motion abnormalities, and ischemia [18]. Most commonly, patients get converted during grafting of the obtuse marginal vessels or the ramus intermedius [19], and conversion to C-CABG leads to a higher rate of adverse events as shown in previous studies. The use of CPB support electively as and when required, particularly at the first signs of deranged hemodynamics potentially, reduces the risk of emergency conversions and, thereby, adverse outcomes in patients when ON-BH CABG is used.
A significant rise in CRP level after 48 h and a less significant rise in CKMB, Trop I, and NT Pro BNP level from base line after 24/48 h of surgery was noted in group 1 patients as is expected after CPB. But, these did not affect the better postoperative outcome in these patients because of the relatively short duration of about 15 min average of CPB support without cross clamping.
Finally, according to the best evidence paper by Sepehripour [20], with the exception of one study that favored the off-pump technique, their review did not demonstrate a statistically significant difference in terms of mortality between the off-pump and on-pump beating-heart surgery neither any significant difference in any reported morbidity outcomes. However, there was a trend towards better outcomes for the on-pump beating-heart technique, despite a higher risk profile in terms of age, ejection fraction, and burden of coronary disease. Consistent statistically significant differences between the groups were the mean number of grafts performed and the completeness of revascularization, both of which were higher with the on-pump beating-heart technique.
Conclusion
“Intermittent” ON-BH CABG in our experience has shown to be a technically reliable method of coronary revascularization taking dual advantage of OPCAB and C-CABG on one hand while considerably eliminating the disadvantages and side effects of both the techniques on the other. It is a promising new method of coronary revascularization without the need for any new learning curve and can be likely considered for all patients requiring CABG.
Limitations of the study
-
1.
New technique - Although, it has shown its superiority in a number of outcomes like safety, more number of grafts, lesser blood loss, shorter operating time, and a better perioperative course, this newer technique still requires further validation in terms of risk stratification.
-
2.
Sample size - The other limitation was the few number of patients incorporated in the study. This was not unintentional since we needed a review of our technique in a short time to decide whether to carry on or not.
-
3.
Lack of randomization - This would be a better study if patients could be randomized rather than chosen as a cohort (due to the relatively small number which we tested). Randomization in the future with a much larger sample size would therefore be ideal to verify our present study.
References
Perrault LP, Menasche P, Peynet J, et al. On-pump, beating heart coronary artery operations in high risk patients: an acceptable trade-off. Ann Thorac Surg. 1997;64:1368–73.
Al-Ruzzeh S, Nakamura K, Athanasiou T, et al. Does off-pump coronary artery bypass (OPCAB) surgery improve the outcome in high-risk patients?: a comparative study of 1398 high risk patients. Eur J Cardiothorac Surg. 2003;23:50–5.
Takagi H, Umemoto T. Worse long-term survival after off-pump than on-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2014;148:1820–9.
Légaré JF, Buth KJ, Hirsch GM. Conversion to on pump from OPCAB is associated with increased mortality: results from a randomized controlled trial. Eur J Cardiothorac Surg. 2005;27:296–301.
Chaudhry UA, Harling L, Sepehripour AH, et al. Beating- heart versus conventional on-pump coronary artery bypass grafting: a meta-analysis of clinical outcomes. Ann Thorac Surg. 2015;100:2251–60.
Ueki C, Sakaguchi G, Akimoto T, Ohashi Y, Sato H. On-pump beating-heart technique is associated with lower morbidity and mortality following coronary artery bypass grafting: a meta-analysis. Eur J Cardiothorac Surg. 2016;50:813–21.
Miyahara K, Matsuura A, Takemura H, et al. On-pump beating-heart coronary artery bypass grafting after acute myocardial infarction has lower mortality and morbidity. J Thorac Cardiovasc Surg. 2008;135:521–6.
Izumi Y, Magishi K, Ishikawa N, Kimura F. On-pump beating- heart coronary artery bypass grafting for acute myocardial infarction. Ann Thorac Surg. 2006;81:573–6.
Rastan AJ, Eckenstein JI, Hentschel B, et al. Emergency coronary artery bypass graft surgery for acute coronary syndrome: beating heart versus conventional cardioplegic cardiac arrest strategies. Circulation. 2006;114:I477–85.
Brown WR, Moody DM, Challa VR, Stump DA, Hammon JW. Longer duration of cardiopulmonary bypass is associated with greater numbers of cerebral microemboli. Stroke. 2000;31:707–13.
Gould BL, Clayton PD, Jensen RL, Liddle HV. Association between early graft patency and late outcome for patients undergoing coronary artery bypass surgery. Circulation. 1984;69:569–76.
Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow- up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616–26.
Synnergren MJ, Ekroth R, Oden A, Rexius H, Wiklund L. Incomplete revascularization reduces survival benefit of coronary artery bypass grafting: role of off-pump surgery. J Thorac Cardiovasc Surg. 2008;136:29–36.
Dayan V, Paganini JJ, Marichal A, Brusich D. On-pump beating/non-beating CABG in stable angina have similar outcomes. Braz J Cardiovasc Surg. 2018;33:183–8.
Kim HJ, Oh YN, Ju MH, et al. On-pump beating heart versus conventional coronary artery bypass grafting: comparative study on early and long-term clinical outcomes. J Thorac Dis. 2018;10:2656–65.
Borowski A, Korb H. Myocardial infarction in coronary bypass surgery using on-pump, beating heart technique with pressure and volume-controlled coronary perfusion. J Card Surg. 2002;17:272–8.
Jones RH. Intraoperative crossover: the well-kept surgical secret to apparent surgical success. J Am Coll Cardiol. 2005;45:1529–31.
Kapetanakis EI, Stamou SC, Dullum MK, et al. The impact of aortic manipulation on neurologic outcomes after coronary artery bypass surgery: a risk-adjusted study. Ann Thorac Surg. 2004;78:1564–71.
Sergeant P, de Worm E, Meyns B, Wouters P. The challenge of departmental quality control in the re-engineering towards off-pump coronary artery bypass grafting. Eur J Cardiothorac Surg. 2001;20:538–43.
Sepehripour AH, Chaudhry UA, Harling L, Athanasiou T. Off-pump or on-pump beating heart: which technique offers better outcomes following coronary revascularization? Interact Cardiovasc Thorac Surg. 2015;20:546–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from the patient included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, S.K., Kumar, S., Prakash, V. et al. Intermittent on-pump beating-heart coronary artery bypass grafting—a safer option. Indian J Thorac Cardiovasc Surg 35, 557–563 (2019). https://doi.org/10.1007/s12055-019-00821-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-019-00821-2