Abstract
Aim
Cardiogenic shock has poor prognosis with medical management alone and/or intra-aortic balloon pump support. Levitronix Centrimag®centrifugal pump has been increasingly used to bridge patients to decision for further advanced mechanical uni- or bi-ventricular support with a view to heart transplantation on the newly implemented super-urgent recipient scheme. We sought to review our experience as a designated centre for mechanical circulatory support to investigate its role despite the emergence of percutaneously implantable miniature devices.
Methods
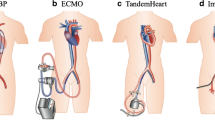
Between April 2009 and December 2015, 98 patients in cardiogenic shock [age 41.4 ± 12.7 years; 52 (53%) male and 46 (47%) female] underwent mechanical circulatory support of whom 90 were treated with Levitronix Centrimag as a primary procedure. Diagnosis was dilated cardiomyopathy [37 (38.1%)], ischaemic cardiomyopathy [25 (25.8%)], and other [36 (36.1%)]. Main indications were cardiogenic shock or decompensated heart failure. Other indications were early graft failure following heart transplant or right ventricular failure following left ventricular assist device insertion. Levitronix support was as follows: extra corporeal membrane oxygenation [22 (24.4%) central, 26 (28.9%) peripheral], Left Ventricular Assist Device [12 (13.3%)], Right Ventricular Assist Device [5 (5.6%)], and Bi-Ventricular Assist Device [25 (27.8%)].
Results
The average duration of support on Levitronix was 17.1 days (range 1–111). The 30-day survival was 52% (47 patients), 6-month survival was 40% (36 patients), and 12-month survival was 37.7% (34 patients). Of the surviving patients, five underwent successful orthotopic heart transplantation, one received a HeartMate II which was subsequently explanted because of myocardial recovery, and one received a HeartMate II and is currently on the transplant list. Cause of death while on support was multiorgan failure [12 (13.3%)], cardiovascular system (CVA)/Neurological [10 (11.1%)], further haemodynamic deterioration [9 (10%)], graft failure [5 (5.6%)], bleeding [4 (4.4%)], sepsis [3 (3.3%)], myocardial infarction [3 (3.3%)], right ventricular failure [3 (3.3%)], pulmonary embolism [1 (1.1%)], embolic [1 (1.1%)], respiratory failure [1 (1.1%)], influenza + rejection [1 (1.1%)], and unknown [3 (3.3%)].
Conclusion
Levitronix Centrimag® remains a versatile device with potential in an acute setting. Early aggressive treatment and a younger patient population may well justify its use.




Similar content being viewed by others
References
Thiele H, Schuler G, Neumann FJ, et al. Intraaortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock: design and rationale of the Intraaortic Balloon Pump in Cardiogenic Shock II (IABP-SHOCK II) trial. Am Heart J. 2012;163:938–45.
Thiele H, Zeymer U, Neumann FJ, et al. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013;382:1638–45.
Perera D, Lumley M, Pijls N, Patel MR. Intra-aortic balloon pump trials. Questions, answers and unresolved issues. Circ Cardiovasc Interv. 2013;6:317–21.
De Robertis F, Birks EJ, Rogers P, Dreyfus G, Pepper JR, Khaghani A. Clinical performance with the Levitronix Centrimag short-term ventricular assist device. J Heart Lung Transplant. 2006;25:181–6.
Shuhaiber JH, Jenkins D, Berman M, et al. The Papworth experience with the Levitronix CentriMag ventricular assist device. J Heart Lung Transplant. 2008;27:158–64.
Mikus E, Tripodi A, Calvi S, Giglio MD, Cavallucci A, Lamarra M. CentriMag venoarterial extracorporeal membrane oxygenation support as treatment for patients with refractory postcardiotomy cardiogenic shock. ASAIO J. 2013;59:18–23.
Whitson BA, D'CunhaJ KAC, Boyle AJ, Liao KK. Levitronix ventricular assist devices as a bridge to recovery after profound biventricular heart failure associated with pulmonary aspergillosis. J Heart Lung Transplant. 2007;26:345–9.
Vollroth M, Barten MJ, Mohr FW, Garbade J. Biventricular Levitronix CentriMag assist device: a “bridge to recovery” solution in patients with acute fulminant myocarditis. Case Rep Surg. 2012; ID 907490.
John R, Liao K, Lietz K, et al. Experience with the Levitronix CentriMag circulatory support system as a bridge to decision in patients with refractory acute cardiogenic shock and multisystem organ failure. J Thorac Cardiovasc Surg. 2007;134:351–8.
De Robertis F, Rogers P, Amrani M, et al. Bridge to decision using the Levitronix Centrimag short-term ventricular assist device. J Heart Lung Transplant. 2008;27:474–8.
Santise G, Petrou M, Pepper JR, Dreyfus G, Khaghani A, Birks EJ. Levitronix as a short-term salvage treatment for primary graft failure after heart transplantation. J Heart Lung Transplant. 2006;25:495–8.
Bělohlávek J, Mlček M, Huptych M, et al. Coronary versus carotid blood flow and coronary perfusion pressure in a pig model of prolonged cardiac arrest treated by different modes of venoarterial ECMO and intraaortic balloon counterpulsation. Crit Care. 2012;16:R50.
Patrick H. “The rhythm is gonna get you...”: extracorporeal membrane oxygenation with and without intra-aortic balloon pumps. Crit Care Med. 2014;42:2143–4.
Petroni T, Harrois A, Amour J, et al. Intra-aortic balloon pump effects on macrocirculation and microcirculation in cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation. Crit Care Med. 2014;42:2075–82.
Yang F, Jia ZS, Xing JL, et al. Effects of intra-aortic balloon pump on cerebral blood flow during peripheral venoarterial extracorporeal membrane oxygenation support. J Transl Med. 2014;12:106.
Clark JB, Wang S, Palanzo DA, et al. Current techniques and outcomes in extracorporeal life support. Artif Organs. 2015;39:926–30.
Life support organization registry report, International summary, January 2015. Ann Arbor, MI. Extracorporeal Life Support Organization. 2015; p. 1–26.
Burkhoff D, Cohen H, Brunckhorst C, O'Neill WW, for the Tandem Heart Investigators Group. A randomized multicenter clinical study to evaluate the safety and efficacy of the Tandem Heart percutaneous left ventricular assist device versus conventional therapy with intraaortic balloon pumping for treatment of cardiogenic shock. Am Heart J. 2006;152:469.e1–8.
Thiele H, Smalling RW, Schuler GC. Percutaneous left ventricular assist devices in acute myocardial infarction complicated by cardiogenic shock. Eur Heart J. 2007;28:2057–63.
Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving outcomes. Circulation. 2008;117:686–97.
Cheng JM, den Uil CA, Hoeks SE, et al. Percutaneous left ventricular assist devices vs. intra-aortic balloon pump counterpulsation for treatment of cardiogenic shock: a meta-analysis of controlled trials. Eur Heart J. 2009;30:2102–8.
Desai NR, Bhatt DL. Evaluating percutaneous support for cardiogenic shock: data shock and sticker shock. Eur Heart J. 2009;30:2073–5.
Seyfarth M, Sibbing D, Bauer I, et al. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J Am Coll Cardiol. 2008;52:1584–8.
Kar B, Basra SS, Shah NR, Loyalka P. Percutaneous circulatory support in cardiogenic shock. Interventional bridge to recovery. Circulation. 2012;125:1809–17.
O'Neill WW, Kleiman NS, Moses J, et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II Study. Circulation. 2012;126:1717–27.
Dangas GD, Kini AS, Sharma SK, et al. Impact of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump on prognostically important clinical outcomes in patients undergoing high-risk percutaneous coronary intervention (from the PROTECT II Randomized Trial). Am J Cardiol. 2014;113:222–8.
Guglin M, Burchett A. VA-ECMO in cardiogenic shock in adults: indications and outcomes. VAD J. 2016; doi:10.13023/VAD.2016.08.
Wang S, Izer JM, Clark JB, et al. In vivo hemodynamic performance evaluation of novel electrocardiogram-synchronized pulsatile and nonpulsatile extracorporeal life support systems in an adult swine model. Artif Organs. 2015;39:E90–E101.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Compliance with ethical standards
This is a retrospective observational study performed at the Golden Jubilee National Hospital and was approved by the clinical governance and ethics committee of the hospital. All patients had given informed consent. There was no funding for the study. The authors had no conflicts of interest(s) to declare. This article does not contain any studies with animals performed by any of the authors.
Additional information
This work has been presented as a Poster at EuroELSO 2016, 1–4 June 2016, Glasgow
Rights and permissions
About this article
Cite this article
Capoccia, M., Avtaar Singh, S., Hegazy, Y. et al. Rescue Levitronix Centrimag as a bridge to decision: is it still worthwhile?. Indian J Thorac Cardiovasc Surg 33, 303–308 (2017). https://doi.org/10.1007/s12055-017-0582-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-017-0582-2