Abstract
Purpose
Surveillance, treatment, and outcomes for African-American (AA) populations with hepatocellular carcinoma (HCC) remain under evaluated. This study evaluated demographics, surveillance, therapy, and outcomes for a predominately AA population.
Methods
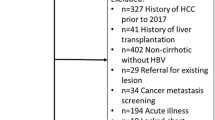
The electronic medical records of a large health-care provider were used to identify 274 patients with visits for HCC between 2010 and 2017. Tumor size at diagnosis was defined by imaging with ≤ 5 cm being defined as “small.” Surveillance for HCC was defined based on ultrasound (US) assessments.
Results
Patients were primarily AA (78%) and male (76%) with an average age at diagnosis of 62 years. Hepatitis C virus (HCV) was more likely to be a risk factor for the development of HCC in AA as compared to non-AA (92% vs 67%; p < 0.005). Surveillance rates were low (16% for AA vs 7% for non-AA). An aspartate aminotransferase platelet ratio index (APRI) value > 0.7 within 2 years of tumor diagnosis was a strong predictor for the risk of the development of HCC (86% AA vs 79 % non-AA). In this study, race was not a factor in treatment or outcomes, and most patients received tumor ablative treatment.
Conclusion
Given the low surveillance rates and the demonstrated increased survival for patients with small tumors, ways to increase surveillance must be initiated. The results of this study demonstrate the need for physician/patient education on the importance of surveillance US. Further, this study supports routine assessment of APRI in AA patients in an effort to identify patients in whom intensive surveillance will significantly improve earlier detection of tumors.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Njei B, Rotman Y, Ditah I, Lim JK. Emerging trends in hepatocellular carcinoma incidence and mortality. Hepatology. 2015;61(1):191–9. https://doi.org/10.1002/hep.27388.
Alazawi W, Cunningham M, Dearden J, Foster GR. Systematic review: outcome of compensated cirrhosis due to chronic hepatitis C infection. Aliment Pharmacol Ther. 2010;32(3):344–55. https://doi.org/10.1111/j.1365-2036.2010.04370.x.
Mittal S, El-Serag HB. Epidemiology of hepatocellular carcinoma: consider the population. J Clin Gastroenterol. 2013;47(Suppl):S2–6. https://doi.org/10.1097/MCG.0b013e3182872f29.
Ghouri YA, Mian I, Rowe JH. Review of hepatocellular carcinoma: epidemiology, etiology, and carcinogenesis. J Carcinog. 2017;16:1. https://doi.org/10.4103/jcar.JCar_9_16.
Bowen DG, Walker CM. Adaptive immune responses in acute and chronic hepatitis C virus infection. Nature. 2005;436(7053):946–52. https://doi.org/10.1038/nature04079.
Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc. 2006;98(12):1934–9.
Xu L, Kim Y, Spolverato G, Gani F, Pawlik TM. Racial disparities in treatment and survival of patients with hepatocellular carcinoma in the United States. Hepatobiliary Surg Nutr. 2016;5(1):43–52. https://doi.org/10.3978/j.issn.2304-3881.2015.08.05.
Mathur AK, Osborne NH, Lynch RJ, Ghaferi AA, Dimick JB, Sonnenday CJ. Racial/ethnic disparities in access to care and survival for patients with early-stage hepatocellular carcinoma. Arch Surg. 2010;145(12):1158–63. https://doi.org/10.1001/archsurg.2010.272.
Ha J, Yan M, Aguilar M, Bhuket T, Tana MM, Liu B, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer. 2016;122(16):2512–23. https://doi.org/10.1002/cncr.30103.
Howlader NNA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) SEER Cancer Statistics Review, 1975-2016, National Cancer Institute. Bethesda, MD, . https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
Estevez J, Yang JD, Leong J, Nguyen P, Giama NH, Zhang N, et al. Clinical features associated with survival outcome in African-American patients with hepatocellular carcinoma. Am J Gastroenterol. 2019;114(1):80–8. https://doi.org/10.1038/s41395-018-0261-y.
Winters AC, Sung JC, Wyatt B, Berera D, Schiano TD, Schwartz ME, et al. At diagnosis of hepatocellular carcinoma, African Americans with hepatitis C have better liver function than other patients. Clin Liver Dis (Hoboken). 2018;12(4):109–12. https://doi.org/10.1002/cld.745.
Rich NE, Hester C, Odewole M, Murphy CC, Parikh ND, Marrero JA, et al. Racial and ethnic differences in presentation and outcomes of hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2019;17(3):551–559.e551. https://doi.org/10.1016/j.cgh.2018.05.039.
Reddy N, Naylor P, Hakim Z, Asbahi R, Ravindran K, May E, et al. Effect of treatment for CHC on liver disease progression and hepatocellular carcinoma development in African Americans. J Clin Transl Hepatol. 2015;3(3):163–8. https://doi.org/10.14218/jcth.2015.00013.
Stubbs A, Naylor P, Ravindran K, Benjaram S, Reddy N, Mutchnick S, et al. Racial diversity in mortality and morbidity in urban patients with hepatitis C. J Viral Hepat. 2016;23(6):439–46. https://doi.org/10.1111/jvh.12504.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–2. https://doi.org/10.1002/hep.24199.
Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med. 1996;101(4):422–34. https://doi.org/10.1016/s0002-9343(96)00197-0.
Trinchet JC, Chaffaut C, Bourcier V, Degos F, Henrion J, Fontaine H, et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology. 2011;54(6):1987–97. https://doi.org/10.1002/hep.24545.
Santi V, Trevisani F, Gramenzi A, Grignaschi A, Mirici-Cappa F, Del Poggio P, et al. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010;53(2):291–7. https://doi.org/10.1016/j.jhep.2010.03.010.
Khalaf N, Ying J, Mittal S, Temple S, Kanwal F, Davila J, et al. Natural history of untreated hepatocellular carcinoma in a US cohort and the role of cancer surveillance. Clin Gastroenterol Hepatol. 2017;15(2):273–281.e271. https://doi.org/10.1016/j.cgh.2016.07.033.
Kanwal F, Singal AG. Surveillance for hepatocellular carcinoma: current best practice and future direction. Gastroenterology. 2019. https://doi.org/10.1053/j.gastro.2019.02.049.
Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan Z, et al. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154(2):85–93. https://doi.org/10.7326/0003-4819-154-2-201101180-00006.
Zhao C, Jin M, Le RH, Le MH, Chen VL, Jin M, et al. Poor adherence to hepatocellular carcinoma surveillance: a systematic review and meta-analysis of a complex issue. Liver Int. 2018;38(3):503–14. https://doi.org/10.1111/liv.13555.
EASL clinical practice guidelines: management of hepatocellular carcinoma (2018). J Hepatol 69 (1):182-236. https://doi.org/10.1016/j.jhep.2018.03.019
Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317–70. https://doi.org/10.1007/s12072-017-9799-9.
Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–80. https://doi.org/10.1002/hep.29086.
Covey AM. Hepatocellular carcinoma: updates to screening and diagnosis. 2018;16(5S):663. https://doi.org/10.6004/jnccn.2018.0052.
Fitzmorris P, Shoreibah M, Anand BS, Singal AK. Management of hepatocellular carcinoma. J Cancer Res Clin Oncol. 2015;141(5):861–76. https://doi.org/10.1007/s00432-014-1806-0.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90. https://doi.org/10.1056/NEJMoa0708857.
Costentin CE, Layese R, Bourcier V, Cagnot C, Marcellin P, Guyader D, et al. Compliance with hepatocellular carcinoma surveillance guidelines associated with increased lead-time adjusted survival of patients with compensated viral cirrhosis: a multi-center cohort study. Gastroenterology. 2018;155(2):431–442.e410. https://doi.org/10.1053/j.gastro.2018.04.027.
Kawamura Y, Arase Y, Ikeda K, Seko Y, Imai N, Hosaka T, et al. Large-scale long-term follow-up study of Japanese patients with non-alcoholic fatty liver disease for the onset of hepatocellular carcinoma. Am J Gastroenterol. 2012;107(2):253–61. https://doi.org/10.1038/ajg.2011.327.
Hann HW, Wan S, Lai Y, Hann RS, Myers RE, Patel F, et al. Aspartate aminotransferase to platelet ratio index as a prospective predictor of hepatocellular carcinoma risk in patients with chronic hepatitis B virus infection. J Gastroenterol Hepatol. 2015;30(1):131–8. https://doi.org/10.1111/jgh.12664.
Acknowledgment
This abstract was presented at the Digestive Disease Week in Chicago, IL, USA, on May 8, 2017, and was published as Abstract Mo1419.
Funding
This research was supported in part by an individual investigator-initiated grant from Gilead Sciences to Dr. Milton Mutchnick and Dr. Paul Naylor. Dr. Milton Mutchnick is a member of the Speaker’s Bureau for Abbvie, CLDF, Gilead, and Intercept.
Author information
Authors and Affiliations
Contributions
Drs. Brian Rutledge, Neha Sahni, Paul Naylor, Philip Philip, Murray Ehrinpreis, and Milton Mutchnick were responsible for the conception and design of the study and interpretation of data analysis and drafting of the manuscript. Dr. Paul Naylor was responsible for the data analysis. Drs. Jenny Jan and Sindhuri Benjaram made substantial contributions to the acquisition of the data and also subsequent analysis and interpretation of the data along with being responsible for the revisions and critical review of the drafts. All authors have approved the final version of this manuscript.
Corresponding author
Ethics declarations
Statement of Ethics
This original research article is in compliance with the guidelines for human studies and in accordance with the World Medical Association Declaration of Helsinki. The subjects of this study have not been referred to by their real name, and further no identifying image has been included in this report.
Conflict of Interest
The authors declare that they have no conflict(s) of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rutledge, B., Jan, J., Benjaram, S. et al. Racial Diversity in Hepatocellular Carcinoma in a Predominately African-American Population at an Urban Medical Center. J Gastrointest Canc 51, 972–979 (2020). https://doi.org/10.1007/s12029-019-00342-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-019-00342-6