Abstract
Background and Aims
Intracranial compliance refers to the relationship between a change in intracranial volume and the resultant change in intracranial pressure (ICP). Measurement of compliance is useful in managing cardiovascular and respiratory failure; however, there are no contemporary means to assess intracranial compliance. Knowledge of intracranial compliance could complement ICP and cerebral perfusion pressure (CPP) monitoring in patients with severe traumatic brain injury (TBI) and may enable a proactive approach to ICP management. In this proof-of-concept study, we aimed to capitalize on the physiologic principles of intracranial compliance and vascular reactivity to CO2, and standard-of-care neurocritical care monitoring, to develop a method to assess dynamic intracranial compliance.
Methods
Continuous ICP and end-tidal CO2 (ETCO2) data from children with severe TBI were collected after obtaining informed consent in this Institutional Review Board-approved study. An intracranial pressure-PCO2 Compliance Index (PCI) was derived by calculating the moment-to-moment correlation between change in ICP and change in ETCO2. As such, “good” compliance may be reflected by a lack of correlation between time-synched changes in ICP in response to changes in ETCO2, and “poor” compliance may be reflected by a positive correlation between changes in ICP in response to changes in ETCO2.
Results
A total of 978 h of ICP and ETCO2 data were collected and analyzed from eight patients with severe TBI. Demographic and clinical characteristics included patient age 7.1 ± 5.8 years (mean ± SD); 6/8 male; initial Glasgow Coma Scale score 3 [3–7] (median [IQR]); 6/8 had decompressive surgery; 7.1 ± 1.4 ICP monitor days; ICU length of stay (LOS) 16.1 ± 6.8 days; hospital LOS 25.9 ± 8.4 days; and survival 100%. The mean PCI for all patients throughout the monitoring period was 0.18 ± 0.04, where mean ICP was 13.7 ± 2.1 mmHg. In this cohort, PCI was observed to be consistently above 0.18 by 12 h after monitor placement. Percent time spent with PCI thresholds > 0.1, 0.2, and 0.3 were 62% [24], 38% [14], and 23% [15], respectively. The percentage of time spent with an ICP threshold > 20 mmHg was 5.1% [14.6].
Conclusions
Indirect assessment of dynamic intracranial compliance in TBI patients using standard-of-care monitoring appears feasible and suggests a prolonged period of derangement out to 5 days post-injury. Further study is ongoing to determine if the PCI—a new physiologic index, complements utility of ICP and/or CPP in guiding management of patients with severe TBI.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) is a leading cause of death and long-term neurologic impairment in adults and children. Nearly 1 in 5 childhood victims of severe TBI die as a direct consequence of their injury, and those that survive typically have significant neurological morbidity associated with poor quality of life [1, 2]. Despite the public health consequences, standard-of-care neuromonitoring for patients with severe TBI has not changed in decades. The currently accepted standard-of-care for severe TBI focuses on treating elevations in intracranial pressure (ICP), while ensuring adequate cerebral perfusion pressure (CPP) [3]. Thus, the “gold standard” for monitoring and management of severe TBI currently hinges on ICP-directed therapy. Remarkably, the clinical utility of ICP monitoring for severe TBI in both children and adults is controversial [4, 5]. Though attempts have been made to develop computational tools to enrich the utility of ICP monitoring data [6, 7], there exists no widely accepted bedside tool to inform a proactive approach to management of severe TBI and treatment decisions remain largely reactive or empirical. Methodology that would guide individualized application of therapies to prevent ICP from exceeding threshold, optimize cerebral perfusion, prevent catastrophic herniation, and facilitate initiation, titration and weaning of therapies/interventions would stand to significantly improve neurological outcomes. Assessment of intracranial compliance, i.e., the relationship between a change in intracranial volume and a resultant change in ICP, may help bridge this gap in clinical care. Similar to measuring compliance in cardiovascular and pulmonary physiology, assessment of intracranial compliance could provide critical insight into the capacity of the brain to tolerate abrupt physiologic changes and responses to therapeutic interventions.
The objective of this study was to explore whether minute-to-minute changes in continuous ICP and end-tidal carbon dioxide (ETCO2) data from clinical monitors considered standard-of-care in patients with severe TBI could be used to generate a physiologic index to indirectly assess intracranial compliance. The premise is based on the well-described concept of CO2-cerebral arterial/arteriolar reactivity, where increases or decreases in partial pressure of carbon dioxide (PCO2) produce predictable vasodilatation or vasoconstriction, respectively, quantitatively a 2–7% change in CBF per mmHg change in PCO2 in normal subjects [8, 9] and a ~ 3% change in patients with severe TBI including in children [10,11,12,13,14]. Since CBF is proportional to blood vessel radius to the fourth power and cerebral blood volume (CBV) is linearly related to CBF [15], CBV changes exponentially with small changes in PCO2, commonly seen during the ICU course for mechanically ventilated patients. CO2-driven changes in CBF and resultant changes in CBV would then be reflected as changes in ICP if intracranial compliance is poor. As proof-of-concept, we present a description of the ICP-PCO2 compliance index (PCI), an algorithm to derive a physiologic index that indirectly assesses intracranial compliance in real time, in eight children with severe TBI.
Methods
Study Design
We conducted an Institutional Review Board-approved, prospective observational study of children admitted to the pediatric intensive care unit (PICU) at UPMC Children’s Hospital of Pittsburgh with severe TBI defined as a Glasgow coma scale (GCS) score ≤ 8. In our center, patients with severe TBI are managed in a team approach by pediatric neurocritical care and pediatric neurosurgical physicians informed by published guidelines [16]. As part of standard-of-care, ICP is measured continuously with a surgically placed Codman microsensor (Integra Life Sciences, Plainsville, NJ, USA) and ETCO2 with a CAPNOSTAT 5 sensor (Respironics, Murraysville, PA, USA) in line with the patient’s ventilator. These devices are connected to a General Electric Solar 80,001 clinical monitor (GE Healthcare, Chicago, IL, USA). Data are temporarily stored on a separate server using BedMaster Ex (Excel Medical, Jupiter, FL, USA) software for remote viewing and quality assurance review of patient data. Patient data used in this study were archived after obtaining informed consent from the parents and/or legal guardians. No interventions were performed related to this study, specifically minute ventilation was not manipulated to provoke changes in patient PaCO2 or ETCO2 solely for the purposes of data collection.
Estimation of Intracranial Compliance
ETCO2 and ICP were collected every 5 s and archived. Customized software was developed to analyze archived time series data using MATLAB (MathWorks, Natick, MA, USA). Briefly, ETCO2 and ICP values were sampled at 5 s intervals and filtered to remove artifacts, including absent values at a given time point that represent monitor malfunction or disconnection, ICP values < 0, and ICP or ETCO2 values > 80 mmHg. Signals were smoothed by computation of a local mean representing one-minute windows advancing by 5 s per point. The 5 s interval data were converted to 1-minute mean ETCO2 and ICP, and minute-to-minute delta ETCO2 and delta ICP values. The Pearson’s correlation coefficient was computed between 60 min of synchronous ETCO2 and ICP values for the duration of the monitoring time. The Pearson’s correlations were smoothed to reveal periodic trends. The resulting smoothed correlations define the PCI, an index representing the Pearson’s correlation coefficient between ETCO2 and ICP or delta ETCO2 and delta ICP. The equation for calculating PCI is shown in Fig. 1. Hour-to-hour variability was reduced when calculating the Pearson’s correlation coefficient using delta ETCO2/delta ICP vs. ETCO2/ICP, therefore the correlation between the change in ETCO2 and change in ICP was used for determination of PCI.
Estimating intracranial compliance with continuous ICP and ETCO2 monitoring. Raw data signals are captured from GE Solar 80001 clinical monitors and exported to BedMaster Ex. Raw data are filtered to remove nonsensical data and moment-to-moment correlations between ETCO2 and ICP and ΔETCO2 and ΔICP are calculated using MATLAB, where Xa is a matrix of ETCO2 (or ΔETCO2) and Yb is a matrix of ICP (or ΔICP) values. Correlations are binned into 1 h epochs (n = 60). “Good compliance” may be reflected by a lack of correlation between ETCO2 (gray) and ICP (black), or a PCI ~ 0 (—), and “poor compliance” may be reflected by a positive correlation between ETCO2 and ICP and/or changes in ETCO2 and ICP over time, or a PCI > 0.18 (—). Shown is a patient with a PCI > 0.18 that improved over time (Patient 3). d delta; ETCO2 end-tidal carbon dioxide; ICP intracranial pressure; PCI PCO2 Compliance Index; R correlation (Color figure online)
Descriptive Analysis
Data are presented as mean ± standard deviation (SD) or median [interquartile range (IQR)] as appropriate. Hourly ICP, ETCO2, and PCI data for individual patients were generated using Prism 7.0c (GraphPad Software, Inc., La Jolla, CA, USA). Hourly ICP, CPP, and PCI were pooled for all patients and fit to a smooth curve using local polynomial regression fitting with a span of 0.10. Curve fitting for pooled patient data was performed using the ‘geom_smooth’ function in the ‘ggplot2’ package in R (www.r-project.org and R studio, Boston, MA). The percentage of time PCI was above thresholds of 0.1, 0.2, 0.3, 0.4, and 0.5 is presented as mean, median, 5, 25, 75, and 95th percentiles.
Results
Demographic data from eight consecutive patients with continuous ICP and ETCO2 monitoring as part of the management of severe TBI are shown in Table 1. The mean age was 7.1 ± 5.8 years (range 10 months—15 years), average monitor days 7.1 ± 1.4, average PICU length of stay (LOS) 16.1 ± 6.8 days, and average hospital LOS 25.9 ± 8.4 days. Most patients had intraparenchymal, intraventricular or subarachnoid hemorrhage (62.5%) and/or subdural hematoma (50%), with 37.5% having midline shift on initial head computed tomography (CT). Six of eight patients underwent decompressive surgery for relief of mass effect due to hemorrhage early after hospital admission and often prior to PICU admission and with ICP monitor placement occurring in the operating room (Patients 1, 3, 4, and 7). Patients 2 and 8 underwent decompressive surgery at 3 and 5 h after hospital admission, respectively. As such, decompressive surgery occurred before data collection for determination of PCI in all patients. All patients survived to hospital discharge with 7/8 discharged to an inpatient rehabilitation facility.
PCI was calculated from 978 h of ETCO2 and ICP monitoring (122 ± 33 h/patient). Figure 1 shows the raw ICP and ETCO2 monitor data, plotted at 5-s intervals before and after filtering and smoothing, and PCI calculations from Patient 3. Hourly ICP, ETCO2, and PCI data for all patients are provided in Supplemental Fig. 1 (for all patients, time is displayed as hours since ICU admission). Determining the correlation between ETCO2 and ICP demonstrated substantially more variability than determining the correlation between the change in ETCO2 and the corresponding change in ICP. For this reason, we evaluated PCI determined using changes in ETCO2 and changes in ICP in this patient cohort. The mean PCI across each patient’s entire ICP monitoring period is shown in Table 2. The average PCI for all patients was 0.18 ± 0.04, whereas the average ICP for all patients was 13.0 ± 2.8 mmHg. Several distinct temporal patterns were observed, including PCI ≤ 0.18 (cohort mean) throughout the majority of the monitoring period; PCI > 0.18 throughout the majority of the monitoring period; and PCI > 0.18 initially that resolved later during the monitoring period.
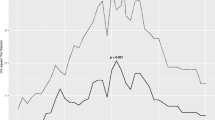
Aggregate data for all patients (n = 8) showing the temporal pattern for PCI, ICP, and CPP are provided in Fig. 2. In this cohort, PCI increases over the first 12 h after admission. Note that the majority of PCI values remain above 0.18 until ~ 90 h after admission. In contrast, aggregate ICP in this cohort remains consistently below our treatment threshold of 20 mmHg throughout the monitoring period. Aggregate temporal data are also provided for patients that did (n = 6) or did not (n = 2) undergo surgical decompression in Supplemental Fig. 2. There appear to be some temporal differences in PCI and ICP between groups; however, because of limited sample sizes particularly in the group that did not undergo surgical decompression, comparisons between groups are not warranted.
Temporal profile of PCI, ICP and CPP in children with severe TBI. Correlation between ΔICP and ΔETCO2 (PCI; blue), vs. ICP (red) and CPP (purple) (n = 8). Data displayed as local polynomial regression fitting with 95% confidence interval (CI) and mean ± SEM (ggplot2, geom_smooth, span 0.1; www.r-project.org). CPP cerebral perfusion pressure; ICP intracranial pressure; PCI PCO2 Compliance Index; SEM standard error of the mean (Color figure online)
Percent time PCI is above threshold for all patients is shown in Fig. 3. The percentage of time spent with a PCI threshold > 0.1, 0.2, 0.3, 0.4, and 0.5 was 62.0% [24.3], 37.5% [13.7], 22.5% [14.7], 7.9% [12.1], and 1.4% [3.2], respectively. The percentage of time spent with an ICP threshold > 20 mmHg was 5.1% [14.6].
Discussion
We present a method for indirectly assessing dynamic intracranial compliance using continuous ICP and ETCO2 data. This novel physiologic index calculates the moving correlations between minute-to-minute changes in ETCO2 and corresponding changes in ICP and is based on the physiologic principle of PCO2-cerebrovascular reactivity, where changes in cerebral blood vessel diameter are reflected in changes in ICP under conditions of poor intracranial compliance. This method is clinically feasible and does not require additional devices or monitors, as both ICP and ETCO2 monitoring are considered standard-of-care for patients with severe TBI.
A linear relationship has been established between the partial pressure of carbon dioxide in arterial blood (PaCO2) and CBV in multiple studies using radioactive and fluorescent tracers in animals undergoing hyperventilation and hypoventilation. The slope of this linear function is similar between species, including nonhuman primates [17,18,19]. Studies in humans have consistently demonstrated that a change in PCO2 of 1 mmHg yields a 2–7% change in CBF [20,21,22,23] with a subsequent 0.9–2.4% change in CBV that is related to changes in arterial CBV without changes in venous or capillary CBV [22, 24]. As CBV represents approximately 4.5% of brain volume [25, 26], it can be inferred that intracranial volume changes by approximately 0.1% for every 1 mmHg change in PaCO2 when CO2 reactivity is intact [20,21,22,23]. Remarkably, CO2-cerebral vascular reactivity has been shown to be at least partially intact in patients with severe TBI, where an ~ 3% change in CBF per 1 mmHg change in PCO2 is reported including studies in children [10,11,12,13,14]. When intracranial compliance is normal, increases in CBV produce no change in ICP. When compliance is poor, even small changes in CBV can profoundly change ICP. For example, in an adult human with 3% CO2 vasoreactivity and a change in PaCO2 by 10 mmHg, this would represent an absolute volume of approximately 1 mL. As such, CO2 control is a key strategy in severe TBI management [16, 27].
Intracranial compliance is a reflection of the capacity to accommodate for changes in volume of one or more of the individual components of the intracranial compartment (brain tissue, brain water, CBV, CSF, hematoma) without a concomitant change in ICP. For perspective, classic studies by Marmarou et al. determined compliance using the pressure volume index (PVI), a method where direct manipulation of intracranial volume is used to provoke changes in ICP [28]. In these studies, up to 2 mL of CSF was withdrawn to calculate PVIWD and determine a volume limit (Vlimit) for each patient, where:
and:
in order to “insure adequate perfusion pressure of 55 mmHg” [29]. Saline was injected into the ventricular catheter at a rate of 1 mL/min until Vlimit or ICPlimit were reached to determine actual PVI [28]. In adult patients with “uncontrollable ICP” PVI averaged 10.5± 3.7 mL during the first 24 h after TBI, and in those identified as having a “tight brain” (PVIWD < 15) the maximum injection volume did not exceed 1 mL [29]. Relevant to our study, the PVI was age-dependent in children without TBI (patients with tethered cord) ranging from 8.2 to 30.1 mL in 3-month to 14-year-old children, respectively [28]. In children with TBI, measured PVI ranged from 33-89% of predicted PVI, and reduced PVI was an accurate predictor of intracranial hypertension [30]. The findings in our current study, indirectly assessing intracranial compliance by determining whether ICP changes occur in response to changes in CO2, are consistent with these classic studies that used direct manipulation of intracranial volume to directly assess compliance.
In this cohort of children with severe TBI, the PCI increases over the first 12 h after admission, with the majority of PCI values remaining above 0.18 until ~ 90 h (Fig. 2). The PCI was above a threshold of 0.18 approximately 40% of the monitoring period (Fig. 3). In contrast, ICP in this cohort remained below the guidelines-based target threshold of 20 mmHg the majority of the monitoring period, the latter related to the fact that clinical interventions are directed at treating and/or preventing ICP “spikes” > 20 mmHg [3]. This implies that alterations in PCI could reflect a more subtle derangement in brain swelling than raised ICP. Indeed, ICP was above the most commonly targeted treatment threshold of 20 mmHg for 5% of the monitoring period in this cohort. Management of ICP includes osmolar therapies, sedation, blood pressure manipulation, CO2 control, CSF diversion and/or surgical decompression empirically or in response to ICP above threshold. Knowledge of the PCI may allow the clinician to predict the patient’s response to therapies, permitting proactive implementation and titration of medications and interventions. Such an approach could individualize the application of therapies to prevent intracranial hypertension and catastrophic herniation, optimize cerebral perfusion, and facilitate weaning when compliance is favorable, and thus direct significant improvements in the quality of neurological outcomes in patients with TBI and other neurocritical care patients requiring ICP monitoring. Support for the potential value of using the PCI to help direct management in pediatric TBI was suggested in early studies of point assessments of the aforementioned PVI [30]. Our proposed continuous assessment of PCI builds on that concept, and uses a safer approach, where continuous changes in PaCO2 in normal care serve to perturb the intracranial compartment, rather than the need for withdrawal of CSF followed by saline boluses.
In this cohort of children with severe TBI several distinct patterns of PCI were observed. These included patients with a PCI ≤ 0.18 throughout the majority of the monitoring period, perhaps a reflection of “good compliance” (Table 2 and Supplemental Fig. 1; patient 2); patients with a PCI > 0.18 throughout the majority of the monitoring period, perhaps a reflection of “poor compliance” (Table 2 and Supplemental Fig. 1; patients 1 and 7); and an initial PCI > 0.18 that resolved later during the monitoring period, perhaps a reflection of transitioning from a state of “poor compliance” to “good compliance” (Table 2 and Supplemental Fig. 1; patients 3, 6, and 8).
It is important to note that six of the eight patients included in this study underwent craniotomy/craniectomy, which would improve intracranial compliance and reduce ICP [31, 32]. However, since the PCI is based on correlations between changes in ETCO2 and ICP, and not magnitude of change, PCI may yield relevant clinical information as to the brain’s capacity to tolerate changes in intracranial volume related to changes in CBV, ventricular CSF volume, edema, or hemorrhage, even after craniotomy/craniectomy. Furthermore, intracranial hypertension often persists despite decompression [33, 34] and assessment of compliance remains physiologically relevant in the lung and vasculature which are not confined to a fixed volume as is the case with the intact cranial vault. In addition, two patients suffered penetrating TBI from gunshot wounds, which likely worsened intracranial compliance due to cerebral edema surrounding the bullet tract [35]. Further study in a larger group of patients is necessary to identify the potential significance of temporal PCI patterns and the impact of surgical interventions and penetrating injury.
This exploratory study has other important limitations. First is the small sample size. However, this dataset produced nearly 1000 h of synchronized monitor data, likely sufficient to generate prototype mathematical models in this proof-of-concept study. A prospective study is underway to monitor PCI in a larger cohort of patients with severe TBI and evaluate possible associations with clinical management and patient outcome. Second, patients included in this study spent a limited amount of time with an ICP above a threshold of 20 mmHg (5.1% of the monitoring time), likely related to the clinical emphasis on preventing and treating intracranial hypertension [16]. The PCI and other cerebral physiologic measures would be more clinically relevant when ICP is increased; however, it remains possible that assessment of the PCI would provide clinically relevant information even when ICP is being aggressively controlled. Third, the PCI relies on the assumption that CO2 vasoreactivity is intact. CO2 vasoreactivity can be reduced after TBI; although, it typically remains at least partially intact except in the setting of overwhelming injury. In cases deemed salvageable and managed with standard-of-care, the reported mean CO2 reactivity in severe TBI patients is ~ 3%, including in children [10,11,12,13,14]. CO2 reactivity can be blunted by prolonged durations of hyperventilation. However, since failed clinical trials of hyperventilation [36], CO2 is no longer manipulated as a therapeutic target and hyperventilation is avoided [16]. Attempts have been made to assess intracranial compliance directly; however, none are currently used clinically. This is likely due to the fact that these methods either require additional invasive monitoring [34] or direct manipulation of the intracranial space [29]. Our method capitalizes on data already collected as part of standard-of-care management and as such does not require additional invasive techniques. Also, we used continuous ETCO2 as a surrogate for PaCO2, although changes in ETCO2 strongly correlate with changes in PaCO2 in mechanically ventilated patients [37]. Fourth, our approach is most valid when all other parameters that affect CBF and CBV are constant, such as responses to metabolic demand or blood pressure autoregulation. While this would rarely be the case, the monitoring epochs used (5 s) appear granular enough to detect correlations between changes in ETCO2 and ICP in the milieu of other changing physiologic parameters, as the vascular response to changes in CO2 occurs in seconds [38]. Fifth, our proof-of-concept study does not address the most relevant question from the clinical standpoint, the potential significance of the index to predict elevated ICP or other untoward events. Expanding the sample size and dataset and comparison of PCI thresholds with clinically meaningful parameters including burden of intracranial hypertension and intensity of therapies used to control ICP using advanced mathematical modeling [39] are planned in future studies.
The PCI as currently derived is parsimonious and relies on detecting changes in ICP in response to changes in cerebrovascular volume. It does not take into account other potential contributions to fluctuations in ICP such as changes in CSF volume due to outflow or formation [40], venous capacitance [41], or increased brain tissue water content. However, under physiologic circumstances where a correlation between ETCO2 and ICP is observed (i.e., PCI > 0.18) it could be anticipated that the capacity for further CSF or venous outflow is minimal due to exhausted CSF reservoirs secondary to internal and/or external drainage, and/or that significant brain edema exists. Under physiologic circumstances where vascular volume changes can be counter balanced by outflow of CSF or venous blood out of the cranium, it could be anticipated that fluctuations in ICP will not be observed (i.e., PCI < 0.18). The PCI as currently derived also does not take into account the time constant of the response of cerebral arteries/arterioles to changes in PaCO2 [42]. The cerebrovascular response to changes in PaCO2 has been shown to be rapid [38], and anecdotally hyperventilation quickly reduces ICP in patients with intracranial hypertension. However, since the time constant of CO2-induced cerebrovascular changes may differ during hyper- versus hypoventilation [43], development of PCI models that include cerebrovascular time constants, CBF changes independent of CO2 reactivity, blood pressure autoregulation, and CSF dynamics appears warranted. Development of more robust and less parsimonious models and use of advanced engineering methodologies including filtering procedures and Markov models would also likely reduce variability seen currently with the PCI and improve upon clinical utility.
Finally, it has been shown in classic studies that age is an important determinant of intracranial compliance [28]. At equal pressure, for example, in a series of 23 normal children and 7 normal adults, the mean compliance of infants was 0.34 while that of the older children was 0.62. This is anticipated given the smaller neuroaxis volume in infants, and an age-dependent PVI was demonstrated. The impact of age would thus need to be included in the evaluation of compliance using PCI and should be characterized in future studies including assessment of PCI in adult TBI patients.
Conclusions
Indirect assessment of dynamic intracranial compliance in TBI patients using standard-of-care monitoring appears feasible. Further study is ongoing to determine if the PCI compliments utility of ICP and/or CPP in guiding management or assessing prognosis in pediatric and adult patients with severe TBI.
References
Murphy S, Thomas NJ, Gertz SJ, Beca J, Luther JF, Bell MJ, Wisniewski SR, Hartman AL, Tasker RC. Tripartite stratification of the glasgow coma scale in children with severe traumatic brain injury and mortality: an analysis from a multi-center comparative effectiveness study. J Neurotrauma. 2017;34(14):2220–9. https://doi.org/10.1089/neu.2016.4793.
Sarnaik A, Ferguson NM, O’Meara AI, Agrawal S, Deep A, Buttram S, Bell MJ, Wisniewski SR, Luther JF, Hartman AL, Vavilala MS. Age and mortality in pediatric severe traumatic brain injury: results from an international study. Neurocrit Care. 2018;28(3):302–13.
Kochanek PM, Tasker RC, Bell MJ, Adelson PD, Carney N, Vavilala MS, Selden NR, Bratton SL, Grant GA, Kissoon N, Reuter-Rice KE, Wainwright MS. Management of pediatric severe traumatic brain injury: 2019 consensus and guidelines-based algorithm for first and second tier therapies. Pediatr Crit Care Med. 2019;20(3):269–79. https://doi.org/10.1097/pcc.0000000000001737.
Bennett TD, DeWitt PE, Greene TH, Srivastava R, Riva-Cambrin J, Nance ML, Bratton SL, Runyan DK, Dean JM, Keenan HT. Functional outcome after intracranial pressure monitoring for children with severe traumatic brain injury. JAMA Pediatr. 2017;171(10):965–71. https://doi.org/10.1001/jamapediatrics.2017.2127.
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, Petroni G, Lujan S, Pridgeon J, Barber J, Machamer J, Chaddock K, Celix JM, Cherner M, Hendrix T. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367(26):2471–81. https://doi.org/10.1056/nejmoa1207363.
Donnelly J, Czosnyka M, Adams H, Robba C, Steiner L, Cardim D, Cabella B, Liu X, Ercole A, Hutchinson P, Menon D, Aries M, Smielewski P. Pressure reactivity-based optimal cerebral perfusion pressure in a traumatic brain injury cohort. Acta Neurochir Suppl. 2018;126:209–12.
Akhondi-Asl A, Vonberg FW, Au CC, Tasker RC. Meaning of intracranial pressure-to-blood pressure fisher-transformed pearson correlation-derived optimal cerebral perfusion pressure: testing empiric utility in a mechanistic model. Crit Care Med. 2018;46(12):e1160–6. https://doi.org/10.1097/ccm.0000000000003434.
Battisti-Charbonney A, Fisher J, Duffin J. The cerebrovascular response to carbon dioxide in humans. J Physiol. 2011;589(12):3039–48.
Bruginaux JV, Hodges AN, Hanley PJ, Poulin MJ. Cerebrovascular responses to altitude. Respir Physiol Neurobiol. 2007;158(2–3):212–23.
Enevoldsen EM, Jensen FT. Autoregulation and CO2 responses of cerebral blood flow in patients with acute severe head injury. J Neurosurg. 1978;48(5):689–703. https://doi.org/10.3171/jns.1978.48.5.0689.
Lee JH, Kelly DF, Oertel M, McArthur DL, Glenn TC, Vespa P, Boscardin WJ, Martin NA. Carbon dioxide reactivity, pressure autoregulation, and metabolic suppression reactivity after head injury: a transcranial Doppler study. J Neurosurg. 2001;95(2):222–32. https://doi.org/10.3171/jns.2001.95.2.0222.
Marion DW, Bouma GJ. The use of stable xenon-enhanced computed tomographic studies of cerebral blood flow to define changes in cerebral carbon dioxide vasoresponsivity caused by a severe head injury. Neurosurgery. 1991;29(6):869–73.
Obrist WD, Langfitt TW, Jaggi JL, Cruz J, Gennarelli TA. Cerebral blood flow and metabolism in comatose patients with acute head injury. Relationship to intracranial hypertension. J Neurosurg. 1984;61(2):241–53. https://doi.org/10.3171/jns.1984.61.2.0241.
Ma T, Yeates KO, Moore-Clingenpeel M, O’Brien NF. Age-related carbon dioxide reactivity in children after moderate and severe traumatic brain injury. J Neurosurg Pediatr. 2016;18:38–73.
Leenders KL, Perani D, Lammertsma AA, Heather JD, Buckingham P, Healy MJR, Gibbs JM, Wise RJS, Hatazawa J, Herold S, Beaney RP, Brooks DJ, Spinks T, Rhodes C, Frackowiak RSJ, Jones T. Cerebral blood flow, blood volume, and oxygen utilization. Brain. 1990;113:27–47.
Kochanek PM, Tasker RC, Carney N, Totten AM, Adelson PD, Selden NR, Davis-O’Reilly C, Hart EL, Bell MJ, Bratton SL, Grant GA, Kissoon N, Reuter-Rice KE, Vavilala MS, Wainwright MS. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the brain trauma foundation guidelines, executive summary. Neurosurgery. 2019. https://doi.org/10.1093/neuros/nyz051.
Grubb RLJ, Raichle ME, Eichling JO, Ter-Pogossian MM. The effects of changes in PaCO2 on cerebral blood volume, blood flow, and vascular mean transit time. Stroke. 1974;5(5):630–9.
Phelps ME, Grubb RLJ, Ter-Pogossian MM. Correlation between PaCO2 and regional cerebral blood volume by x-ray fluorescence. J Appl Physiol. 1973;35(2):274–80.
Smith AL, Neufeld GR, Ominsky AJ, Wollman H. Effect of arterial CO2 tension on cerebral blood flow, mean transit time, and vascular volume. J Appl Physiol. 1971;31(5):701–7.
Greenberg JH, Alvi A, Reivich Martin, Kuhl D, Uzell B. Local cerebral blood volume response to carbon dioxide in man. Circ Res. 1978;43:324–33.
Ito H, Kanno I, Ibaraki M, Hatazawa J, Miura S. Changes in human cerebral blood flow and cerebral blood volume during hypercapnia and hypocapnia measured by positron emission tomography. J Cereb Blood Flow Metab. 2003;23(6):665–70. https://doi.org/10.1097/01.wcb.0000067721.64998.f5.
Reinstrup P, Ryding E, Ohlsson T, Dahm PL, Uski T. Cerebral blood volume (CBV) in humans during normo- and hypocapnia. Anesthesiology. 2001;95:1079–82.
Rostrup E, Knudsen GM, Law I, Holm S, Larsson HB, Paulson OB. The relationship between cerebral blood flow and volume in humans. Neuroimage. 2005;24(1):1–11. https://doi.org/10.1016/j.neuroimage.2004.09.043.
Ito H, Ibaraki M, Kanno I, Fukuda H, Miura S. Changes in the arterial fraction of human cerebral blood volume during hypercapnia and hypocapnia measured by positron emission tomography. J Cereb Blood Flow Metab. 2005;25(7):852–7. https://doi.org/10.1038/sj.jcbfm.9600076.
Engvall C, Ryding E, Wirestam R, Holtas S, Ljunggren K, Ohlsson T, Reinstrup P. Human cerebral blood volume (CBV) measured by dynamic susceptibility contrast MRI and 99mTc-RBC SPECT. J Neurosurg Anesthesiol. 2008;20(1):41–4. https://doi.org/10.1097/ana.0b013e31815d4c70.
Ito H, Kanno I, Iida H, Hatazawa J, Shimosegawa E, Tamura H, Okudera T. Arterial fraction of cerebral blood volume in humans measured by positron emission tomography. Ann Nucl Med. 2001;15(2):111–6.
Kim S, McNames J, Goldstein B. Intracranial pressure variation associated with changes in end-tidal CO2. Conf Proc IEEE Eng Med Biol Soc. 2006;1:9–12.
Shapiro K, Marmarou A, Shulman K. Characterization of clinical CSF dynamics and neural axis compliance using the pressure-volume index: I. The normal pressure-volume index. Ann Neurol. 1980;7(6):508–14. https://doi.org/10.1002/ana.410070603.
Maset AL, Marmarou A, Ward JD, Choi S, Lutz HA, Brooks D, Moulton RJ, DeSalles A, Muizelaar JP, Turner H. Pressure-volume index in head injury. J Neurosurg. 1987;67(6):832–40.
Shapiro K, Marmarou A. Clinical applications of the pressure-volume index in treatment of pediatric head injuries. J Neurosurg. 1982;56(6):819–25. https://doi.org/10.3171/jns.1982.56.6.0819.
Timofeev I, Czosnyka M, Nortje J, Smielewski P, Kirkpatrick P, Gupta A, Hutchinson P. Effect of decompressive craniectomy on intracranial pressure and cerebrospinal compensation following traumatic brain injury. J Neurosurg. 2008;108(1):66–73.
Abdullah J, Zamzuri I, Awang S, Sayuthi S, Ghani A, Tahir A, Naing NN. Preliminary report on spiegelberg pre and post-operative monitoring of severe head-injured patients who received decompressive craniectomy. Acta Neurochir Suppl. 2005;95:311–4. https://doi.org/10.1007/3-211-32318-x_64.
Picetti E, Caspani ML, Iaccarino C, Pastorello G, Salsi P, Varioli E, Servadel F. Intracranial pressure monitoring after primary decompressive craniectomy in traumatic brain injury: a clinical study. Acta Neurochir (Wien). 2017;159(4):615–22.
Portella G, Cormio M, Citerio G, Contant C, Kiening K, Enblad P, Piper I. Continuous cerebral compliance monitoring in severe head injury: its relationship with intracranial pressure and cerebral perfusion pressure. Acta Neurochir (Wien). 2005;147(7):707–13.
Oehmichen M, Gehl HB, Meissner C, Petersen D, Hoche W, Gerling I, Konig HG. Forensic pathological aspects of postmortem imaging of gunshot injury to the head: documentation and biometric data. Acta Neuropathol. 2003;105(6):570–80.
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731–9.
Razi E, Moosavi GA, Omidi K, Khakpour Saebi A, Razi A. Correlation of end-tidal carbon dioxide with arterial carbon dioxide in mechanically ventilated patients. Arch Trauma Res. 2012;1(2):58–62. https://doi.org/10.5812/atr.6444.
Vovk A, Cunningham DA, Kowalchuk JM, Paterson DH, Duffin J. Cerebral blood flow responses to changes in oxygen and carbon dioxide in humans. Can J Physiol Pharmacol. 2002;80(8):819–27. https://doi.org/10.1139/y02-105.
Clermont G, Kaplan V, Moreno R, Vincent JL, Linde-Zwirble WT, Hout BV, Angus DC. Dynamic microsimulation to model multiple outcomes in cohorts of critically ill patients. Intensive Care Med. 2004;30(12):2237–44. https://doi.org/10.1007/s00134-004-2456-5.
Davson H. Formation and drainage of the cerebrospinal fluid. Sci Basis Med Annu Rev. 1966;238-59.
Marmarou A, Maset AL, Ward JD, Choi S, Brooks D, Lutz HA, Moulton RJ, Muizelaar JP, DeSalles A, Young HF. Contribution of CSF and vascular factors to elevation of ICP in severely head-injured patients. J Neurosurg. 1987;66(6):883–90. https://doi.org/10.3171/jns.1987.66.6.0883.
Czosnyka M, Richards HK, Reinhard M, Steiner LA, Budohoski K, Smielewski P, Pickard JD, Kasprowicz M. Cerebrovascular time constant: dependence on cerebral perfusion pressure and end-tidal carbon dioxide concentration. Neurol Res. 2012;34(1):17–24.
Puppo C, Kaspirowicz M, Steiner LA, Yelicich B, Lalou DA, Smielewski P, Czosnyka M. Hypocapnea after traumatic brain injury: how does it affect the time constant of the cerebral circulation? J Clin Med Comput. 2019.
Acknowledgements
We would like to recognize the late Dr. Anthony Marmarou for his seminal studies characterizing the PVI in patients with TBI; and thank the entire PICU staff at UPMC Children’s Hospital of Pittsburgh for providing exceptional patient care.
Funding
This study was supported by NIH T32 HD40686 (MSW, JR) and R21 NS115174 (CMH, GC, RSBC), and the Children’s Hospital of Pittsburgh Scientific Program.
Author information
Authors and Affiliations
Contributions
MSW participated in study design, collected and interpreted data, wrote and refined algorithms, and drafted the manuscript; JR collected and analyzed data, wrote R script, and reviewed the final manuscript; CMH analyzed and interpreted data, wrote R script, edited and reviewed the final manuscript; DWS approved the clinical protocol, edited and reviewed the final manuscript; PMK reviewed and interpreted data, and edited the manuscript; GC refined algorithms, analyzed and interpreted data, secured funding, and edited the manuscript; RSBC conceptualized and designed the study, analyzed and interpreted data, secured funding, and edited the manuscript.
Corresponding author
Ethics declarations
Disclosures
U.S. Provisional Patent Application No. 62/848,966 and International Patent Application PCT/US20/25932 have been filed related to the systems and methods for monitoring intracranial compliance.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval/Informed consent
This article reports an Institutional Review Board-approved observational study that did not involve procedures or interventions beyond standard-of-care and solely for the purposes of research. Informed consent from the parents and/or legal guardians was obtained to utilize patient data for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2020_1004_MOESM1_ESM.tif
Estimating intracranial compliance with continuous ICP and ETCO2 monitoring. Raw data signals are captured from GE Solar 80001 clinical monitors and exported to BedMaster Ex. Raw data are filtered to remove nonsensical data and moment-to-moment correlations between ETCO2 (gray) and ICP (black) and ΔETCO2 and ΔICP are calculated using MATLAB. Correlations are binned into 1 h epochs (n = 60) to derive PCI (—). Shown are individual data from all 8 patients. Block arrows denote time of surgical decompression (if applicable). (TIFF 11597 kb)
12028_2020_1004_MOESM2_ESM.tif
Temporal profile of PCI, ICP and CPP in children with severe TBI. Patients are grouped by those that did not undergo surgical decompression (A, n = 2) and those that underwent surgical decompression (B, n = 6). Correlation between ΔICP and ΔETCO2 (PCI; blue), vs. ICP (red) and CPP (purple). Data displayed as local polynomial regression fitting with 95% confidence interval (CI) and mean ± SEM (ggplot2, geom_smooth, span 0.1; www.r-project.org). Note that SEM are provided for Group A despite an n = 2 to show variance. (TIFF 9551 kb)
Rights and permissions
About this article
Cite this article
Wolf, M.S., Rakkar, J., Horvat, C.M. et al. Assessment of Dynamic Intracranial Compliance in Children with Severe Traumatic Brain Injury: Proof-of-Concept. Neurocrit Care 34, 209–217 (2021). https://doi.org/10.1007/s12028-020-01004-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01004-3