Abstract
Background
Spreading depolarizations (SDs) occur in 50–60% of patients after surgical treatment of severe traumatic brain injury (TBI) and are independently associated with unfavorable outcomes. Here we performed a pilot study to examine the relationship between SDs and various types of intracranial lesions, progression of parenchymal damage, and outcomes.
Methods
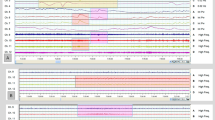
In a multicenter study, fifty patients (76% male; median age 40) were monitored for SD by continuous electrocorticography (ECoG; median duration 79 h) following surgical treatment of severe TBI. Volumes of hemorrhage and parenchymal damage were estimated using unbiased stereologic assessment of preoperative, postoperative, and post-ECoG serial computed tomography (CT) studies. Neurologic outcomes were assessed at 6 months by the Glasgow Outcome Scale-Extended.
Results
Preoperative volumes of subdural and subarachnoid hemorrhage, but not parenchymal damage, were significantly associated with the occurrence of SDs (P’s < 0.05). Parenchymal damage increased significantly (median 34 ml [Interquartile range (IQR) − 2, 74]) over 7 (5, 8) days from preoperative to post-ECoG CT studies. Patients with and without SDs did not differ in extent of parenchymal damage increase [47 ml (3, 101) vs. 30 ml (− 2, 50), P = 0.27], but those exhibiting the isoelectric subtype of SDs had greater initial parenchymal damage and greater increases than other patients (P’s < 0.05). Patients with temporal clusters of SDs (≥ 3 in 2 h; n = 10 patients), which included those with isoelectric SDs, had worse outcomes than those without clusters (P = 0.03), and parenchymal damage expansion also correlated with worse outcomes (P = 0.01). In multivariate regression with imputation, both clusters and lesion expansion were significant outcome predictors.
Conclusions
These results suggest that subarachnoid and subdural blood are important primary injury factors in provoking SDs and that clustered SDs and parenchymal lesion expansion contribute independently to worse patient outcomes. These results warrant future prospective studies using detailed quantification of TBI lesion types to better understand the relationship between anatomic and physiologic measures of secondary injury.





Similar content being viewed by others
References
Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41.
Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375–8.
Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91:1637–40.
Dreier JP. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med. 2011;17:439–47.
de Crespigny A, Rother J, van Bruggen N, Beaulieu C, Moseley ME. Magnetic resonance imaging assessment of cerebral hemodynamics during spreading depression in rats. J Cereb Blood Flow Metab. 1998;18:1008–17.
Murphy TH, Li P, Betts K, Liu R. Two-photon imaging of stroke onset in vivo reveals that NMDA-receptor independent ischemic depolarization is the major cause of rapid reversible damage to dendrites and spines. J Neurosci. 2008;28:1756–72.
Risher WC, Croom D, Kirov SA. Persistent astroglial swelling accompanies rapid reversible dendritic injury during stroke-induced spreading depolarizations. Glia. 2012;60:1709–20.
Dreier JP, Lemale CL, Kola V, Friedman A, Schoknecht K. Spreading depolarization is not an epiphenomenon but the principal mechanism of the cytotoxic edema in various gray matter structures of the brain during stroke. Neuropharmacology 2017.
Hartings JA, Shuttleworth CW, Kirov SA, et al. The continuum of spreading depolarizations in acute cortical lesion development: examining Leao’s legacy. J Cereb Blood Flow Metab. 2017;37:1571–94.
Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab. 2011;31:17–35.
Dreier JP, Fabricius M, Ayata C, et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J Cereb Blood Flow Metab. 2017;37:1595–625.
Hartings JA, Bullock MR, Okonkwo DO, et al. Spreading depolarisations and outcome after traumatic brain injury: a prospective observational study. Lancet Neurol. 2011;10:1058–64.
Hartings JA, Watanabe T, Bullock MR, et al. Spreading depolarizations have prolonged direct current shifts and are associated with poor outcome in brain trauma. Brain. 2011;134:1529–40.
Hinzman JM, Wilson JA, Mazzeo AT, Bullock MR, Hartings JA. Excitotoxicity and metabolic crisis are associated with spreading depolarizations in severe traumatic brain injury patients. J Neurotrauma. 2016;33:1775–83.
Hinzman JM, Andaluz N, Shutter LA, et al. Inverse neurovascular coupling to cortical spreading depolarizations in severe brain trauma. Brain 2014.
Hartings JA, Vidgeon S, Strong AJ, et al. Surgical management of traumatic brain injury: a comparative-effectiveness study of 2 centers. J Neurosurg. 2014;120:434–46.
von Bornstadt D, Houben T, Seidel JL, et al. Supply-demand mismatch transients in susceptible peri-infarct hot zones explain the origins of spreading injury depolarizations. Neuron. 2015;85:1117–31.
Hartings JA, Dreier JP. Real-time detection of lesion development in acute brain injury. J Cereb Blood Flow Metab. 2017;37:1550–2.
Nakamura H, Strong AJ, Dohmen C, et al. Spreading depolarizations cycle around and enlarge focal ischaemic brain lesions. Brain. 2010;133:1994–2006.
Drenckhahn C, Winkler MK, Major S, et al. Correlates of spreading depolarization in human scalp electroencephalography. Brain. 2012;135:853–68.
Hartings JA, York J, Carroll CP, et al. Subarachnoid blood acutely induces spreading depolarizations and early cortical infarction. Brain. 2017;140:2673–90.
Dreier JP, Woitzik J, Fabricius M, et al. Delayed ischaemic neurological deficits after subarachnoid haemorrhage are associated with clusters of spreading depolarizations. Brain. 2006;129:3224–37.
Luckl J, Lemale CL, Kola V, et al. The negative ultraslow potential, electrophysiological correlate of infarction in the human cortex. Brain 2018.
Hartings JA, Strong AJ, Fabricius M, et al. Spreading depolarizations and late secondary insults after traumatic brain injury. J Neurotrauma. 2009;26:1857–66.
Strong AJ, Fabricius M, Boutelle MG, et al. Spreading and synchronous depressions of cortical activity in acutely injured human brain. Stroke. 2002;33:2738–43.
Fabricius M, Fuhr S, Bhatia R, et al. Cortical spreading depression and peri-infarct depolarization in acutely injured human cerebral cortex. Brain. 2006;129:778–90.
Eriksen N, Rostrup E, Andersen K, et al. Application of stereological estimates in patients with severe head injuries using CT and MR scanning images. Br J Radiol. 2010;83:307–17.
Gundersen HJ, Jensen EB, Kieu K, Nielsen J. The efficiency of systematic sampling in stereology–reconsidered. J Microsc. 1999;193:199–211.
Hartings JA, Watanabe T, Dreier JP, Major S, Vendelbo L, Fabricius M. Recovery of slow potentials in AC-coupled electrocorticography: application to spreading depolarizations in rat and human cerebral cortex. J Neurophysiol. 2009;102:2563–75.
Jimenez-Roldan L, Alen JF, Gomez PA, et al. Volumetric analysis of subarachnoid hemorrhage: assessment of the reliability of two computerized methods and their comparison with other radiographic scales. J Neurosurg. 2013;118:84–93.
Chastain CA, Oyoyo UE, Zipperman M, et al. Predicting outcomes of traumatic brain injury by imaging modality and injury distribution. J Neurotrauma. 2009;26:1183–96.
Yuh EL, Cooper SR, Ferguson AR, Manley GT. Quantitative CT improves outcome prediction in acute traumatic brain injury. J Neurotrauma. 2012;29:735–46.
Clatterbuck RE, Sipos EP. The efficient calculation of neurosurgically relevant volumes from computed tomographic scans using Cavalieri’s Direct Estimator. Neurosurgery. 1997;40:339–42 (discussion 43).
Stocchetti N, Croci M, Spagnoli D, Gilardoni F, Resta F, Colombo A. Mass volume measurement in severe head injury: accuracy and feasibility of two pragmatic methods. J Neurol Neurosurg Psychiatry. 2000;68:14–7.
Eriksen N, Rostrup E, Fabricius M, et al. Early focal brain injury after subarachnoid hemorrhage correlates with spreading depolarizations. Neurology 2018 (in press).
Krenzlin H, Jussen D, Plath M, et al. Occurrence of spontaneous cortical spreading depression is increased by blood constituents and impairs neurological recovery after subdural hematoma in rats. J Neurotrauma. 2019;36:395–402.
Karabiyikoglu M, Keep R, Hua Y, Xi G. Acute subdural hematoma: new model delineation and effects of coagulation inhibitors. Neurosurgery. 2005;57:565–72 discussion -72.
Lapilover EG, Lippmann K, Salar S, et al. Peri-infarct blood-brain barrier dysfunction facilitates induction of spreading depolarization associated with epileptiform discharges. Neurobiol Dis. 2012;48:495–506.
Dreier JP, Korner K, Ebert N, et al. Nitric oxide scavenging by hemoglobin or nitric oxide synthase inhibition by N-nitro-l-arginine induces cortical spreading ischemia when K+ is increased in the subarachnoid space. J Cereb Blood Flow Metab. 1998;18:978–90.
Alahmadi H, Vachhrajani S, Cusimano MD. The natural history of brain contusion: an analysis of radiological and clinical progression. J Neurosurg. 2010;112:1139–45.
Flint AC, Manley GT, Gean AD, Hemphill JC 3rd, Rosenthal G. Post-operative expansion of hemorrhagic contusions after unilateral decompressive hemicraniectomy in severe traumatic brain injury. J Neurotrauma. 2008;25:503–12.
Stiver SI. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus. 2009;26:E7.
Loane DJ, Kumar A, Stoica BA, Cabatbat R, Faden AI. Progressive neurodegeneration after experimental brain trauma: association with chronic microglial activation. J Neuropathol Exp Neurol. 2014;73:14–29.
Oertel M, Kelly DF, McArthur D, et al. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg. 2002;96:109–16.
Agrawal A, Timothy J, Pandit L, Manju M. Post-traumatic epilepsy: an overview. Clin Neurol Neurosurg. 2006;108:433–9.
Hukkelhoven CW, Steyerberg EW, Habbema JD, et al. Predicting outcome after traumatic brain injury: development and validation of a prognostic score based on admission characteristics. J Neurotrauma. 2005;22:1025–39.
Maas AI, Hukkelhoven CW, Marshall LF, Steyerberg EW. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005;57:1173–82 discussion -82.
Acknowledgements
The authors thank Claus Holst at Frederiksberg Hospital, Copenhagen, Denmark, for statistical advice and Dr. Achala Vagal at the University of Cincinnati Medical Center, OH, USA, for radiologic guidance.
Author Contributions
NE performed stereologic assessments, analyzed data, and drafted the manuscript. BP and ER conceived the project, advised on design and methods, supervised CT analysis, and edited and approved the manuscript. DOO, DM, LAS, AJS, JW, and CP recruited subjects into the study, provided associated data, and edited and approved the manuscript. JPD performed data analysis, contributed to writing and interpretation, and edited and approved the manuscript. PM performed the primary statistical analyses and edited and approved the manuscript. MJL conceived and supervised the project, and edited and approved the manuscript. MF performed data analysis, contributed to writing, and edited and approved the manuscript. JAH recruited subjects into the study, organized data, prepared figures, and drafted and approved the manuscript.
Source of Support
Research was supported by the US Army CDMRP PH/TBI Research Program (Contract No. W81XWH-08-2-0016), the Agnes and Poul Friis´Foundation, the Aase and Ejnar Danielsens Foundation, the Dagmar Marshall’s Foundation, Deutsche Forschungsgemeinschaft (DFG DR 323/5-1), Bundesministerium für Bildung und Forschung (BMBF CSB 01 EO 0801) and FP7 No. 602150 CENTER-TBI.
Conflicts of Interest
The authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eriksen, N., Pakkenberg, B., Rostrup, E. et al. Neurostereologic Lesion Volumes and Spreading Depolarizations in Severe Traumatic Brain Injury Patients: A Pilot Study. Neurocrit Care 30, 557–568 (2019). https://doi.org/10.1007/s12028-019-00692-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00692-w