Abstract
Background
Central nervous system (CNS) infections are particularly prevalent in the adult neurocritical care patient population and are associated with significant morbidity and mortality. Factors relevant to the nature of CNS infections pose significant challenges to clinicians treating afflicted patients. Intraventricular (IVT) administration of antibiotics may offer several benefits over systemic therapy; however, the outcomes and current practices of such treatments are poorly described in the literature.
Objective
To describe current practices and outcomes of patients receiving intraventricular antibiotic treatment for CNS infections in neurological intensive care units of academic medical centers nationwide.
Methods
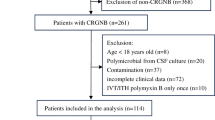
A retrospective cohort study was conducted on patients admitted to intensive care units who received IVT antibiotic treatment at participating centers in the USA between January 01, 2003, and December 31, 2013. Clinical and laboratory parameters, microbiology, surgical and antimicrobial management, and treatment outcomes were collected and described.
Results
Of the 105 patients included, all received systemic antimicrobial therapy along with at least one dose of IVT antimicrobial agents. Intraventricular vancomycin was used in 52.4% of patients. The average dose was 12.2 mg/day for a median duration of 5 days. Intraventricular aminoglycosides were used in 47.5% of the patients, either alone or in combination with IVT vancomycin. The average dose of gentamicin/tobramycin was 6.7 mg/day with a median duration of 6 days. Overall mortality was 18.1%. Cerebrospinal fluid (CSF) culture sterilization occurred in 88.4% of the patients with a rate of recurrence or persistence of positive cultures of 9.5%.
Conclusion
Intraventricular antimicrobial agents resulted in a high CSF sterilization rate. Contemporary use of this route typically results in a treatment duration of less than a week. Prospective studies are needed to establish the optimal patient population, as well as the efficacy and safety of this route of administration.
Similar content being viewed by others
References
Ziai WC, Lewin JJ III. Improving the role of intraventricular antimicrobial agents in the management of meningitis. Curr Opin Neurol. 2009;22(3):277–82.
Clifford H, Stewart G. Intraventricular administration of a new derivative of Polymyxin B in meningitis due to Ps. Pyocyanea. Lancet. 1961;2:177–80.
Arnell K, Enblad P, Wester T, Sjolin J. Treatment of cerebrospinal fluid shunt infections in children using systemic and intraventricular antibiotic therapy in combination with externalization of the ventricular catheter: efficacy in 34 consecutively treated infections. J Neurosurg. 2007;107(3 Suppl):213–9.
Chen K, Wu Y, Wang Q, et al. The methodology and pharmacokinetics study of intraventricular administration of vancomycin in patients with intracranial infections after craniotomy. J Crit Care. 2015;30(1):218e1–5.
Imberti R, Cusato M, Accetta G, et al. Pharmacokinetics of colistin in cerebrospinal fluid after intraventricular administration of colistin methanesulfonate. Antimicrob Agents Chemother. 2012;56(8):4416–21.
James HE, Wilson HD, Connor JD, Walsh JW. Intraventricular cerebrospinal fluid antibiotic concentrations in patients with intraventricular infections. Neurosurgery. 1982;10(1):50–4.
LeBras M, Chow I, Mabasa VH, Ensom MH. Systematic review of efficacy, pharmacokinetics, and administration of intraventricular aminoglycosides in adults. Neurocrit Care. 2016;25(3):492–507.
Popa D, Loewenstein L, Lam SW, et al. Therapeutic drug monitoring of cerebrospinal fluid vancomycin concentration during intraventricular administration. J Hosp Infect. 2016;92(2):199–202.
Tunkel AR, Hasbun R, Bhimraj A, et al. 2017 Infectious diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017;64:e34–65.
Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Bayston R, Hart CA, Barnicoat M. Intraventricular vancomycin in the treatment of ventriculitis associated with cerebrospinal fluid shunting and drainage. J Neurol Neurosurg Psychiatry. 1987;50:1419–23.
Eljaaly K. Dose and duration of intraventricular antibiotic therapy in meningitis. Clin Microbiol Infect. 2016;22(9):817.
Falagas ME, Bliziotis IA, Tam VH. Intraventricular or intrathecal use of polymyxins in patients with Gram-negative meningitis: a systematic review of the available evidence. Int J Antimicrob Agents. 2007;29:9–25.
Katz MD, Rapp RP, Walsh JW. Infection in a functioning ventriculoperitoneal shunt treated with intraventricular gentamicin. Am J Hosp Pharm. 1980;37(2):268–71.
McCracken GH Jr, Mize SG, Threlkeld N. Intraventricular gentamicin therapy in gram-negative bacillary meningitis of infancy. Report of the second neonatal meningitis cooperative study group. Lancet. 1980;1(8172):787–91.
Pfausler B, Haring HP, Kampfl A, et al. Cerebrospinal fluid (CSF) pharmacokinetics of intraventricular vancomycin in patients with staphylococcal ventriculitis associated with external CSF drainage. Clin Infect Dis. 1997;25(3):733–5.
Pfausler B, Spiss H, Beer R, et al. Treatment of staphylococcal ventriculitis associated with external cerebrospinal fluid drains: a prospective randomized trial of intravenous compared with intraventricular vancomycin therapy. J Neurosurg. 2003;98:1040–4.
Pickering LK, Ericsson CD, Ruiz-Palacios G, Blevins J, Miner ME. Intraventricular and parenteral gentamicin therapy for ventriculitis in children. Am J Dis Child. 1978;132:480–3.
Quintiliani R, Lentnek A. Polymixin B in the treatment of Klebsiella pneumoniae meningoventriculitis. Intraventricular and intrathecal administration. Am J Dis Child. 1971;121:239–42.
Shofty B, Neuberger A, Naffaa ME, et al. Intrathecal or intraventricular therapy for post-neurosurgical Gram-negative meningitis: matched cohort study. Clin Microbiol Infect. 2016;22(1):66–70.
Swayne R, Rampling A, Newsom SW. Intraventricular vancomycin for treatment of shunt-associated ventriculitis. J Antimicrob Chemother. 1987;19(2):249–53.
Ziaka M, Markantonis SL, Fousteri M, et al. Combined intravenous and intraventricular administration of colistin methanesulfonate in critically ill patients with central nervous system infection. Antimicrob Agents Chemother. 2013;57(4):1938–40.
Donauer E, Drumm G, Moringlane J, Ostertag C, Kivelitz R. Intrathecal administration of netilmicin in gentamicin-resistant ventriculitis. Acta Neurochir. 1987;86(3–4):83–8.
Gump WC, Walsh JW. Intrathecal colistin for treatment of highly resistant Pseudomonas ventriculitis. J Neurosurg. 2005;102:915–7.
Remes F, Tomas R, Jindrak V, Vanis V, Setlik M. Intraventricular and lumbar intrathecal administration of antibiotics in postneurosurgical patients with meningitis and/or ventriculitis in a serious clinical state. J Neurosurg. 2013;119(6):1596–602.
Ng K, Mabasa VH, Chow I, Ensom MH. Systematic review of efficacy, pharmacokinetics, and administration of intraventricular vancomycin in adults. Neurocrit Care. 2014;20(1):158–71.
Khan SA, Waqas M, Siddiqui UT, et al. Intrathecal and intraventricular antibiotics for postoperative Gram-negative meningitis and ventriculitis. Surg Neurol Int. 2017;8:226.
Wang JH, Lin PC, Chou CH, et al. Intraventricular antimicrobial therapy in postneurosurgical Gram-negative bacillary meningitis or ventriculitis: a hospital-based retrospective study. J Microbiol Immunol Infect. 2014;47(3):204–10.
Shah SS, Ohlsson A, Shah VS. Intraventricular antibiotics for bacterial meningitis in neonates. Cochrane Database Syst Rev. 2012;2012(7):CD004496.
Acknowledgements
This work was conducted through the Neurocritical Care Society Pharmacy Research Committee.
Funding
This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by Grant Number UL1 TR001079 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Author information
Authors and Affiliations
Contributions
JL, CG, WZ conceived of and planned the study. CG, JL developed the data collection tool with input from all authors. All listed authors participated in data collection for their respective centers. Statistical analyses were conducted by AC, DM, WZ, and JL. JL and AC took the lead in writing the manuscript, with assistance from DM. All authors reviewed the manuscript and provided substantive input and edits. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Drs. Lewin, Rowe, Cook, Zaniewski, Clark, Merola, Makii, Kurczewski, Peppard, Giarratano, Gonzales, Neyens, and Brophy have nothing to disclose. Dr. Tesoro reports personal fees from Arbor Pharmaceuticals, outside the submitted work. Dr. Ziai reports personal fees from Headsense, Inc., outside the submitted work.
Rights and permissions
About this article
Cite this article
Lewin, J.J., Cook, A.M., Gonzales, C. et al. Current Practices of Intraventricular Antibiotic Therapy in the Treatment of Meningitis and Ventriculitis: Results from a Multicenter Retrospective Cohort Study. Neurocrit Care 30, 609–616 (2019). https://doi.org/10.1007/s12028-018-0647-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0647-0