Abstract
Background
Studies suggested that the neutrophil-to-lymphocyte ratio (NLR) was associated with unfavorable outcomes in different diseases such as intracerebral hemorrhage, cardiovascular problem, cancer, and severe traumatic brain injury (sTBI). We aimed to evaluate the relationship between peak NLR and 1-year outcomes in patients with sTBI.
Methods
We retrospectively reviewed the clinical data of patients with sTBI who were treated in our department between January 2013 and January 2017. NLRs between day 1 and day 12 after admission as well as other related indicators were collected. The relationship between peak NLR and 1-year outcomes was analyzed. Factors associated with larger peak NLR were also explored.
Results
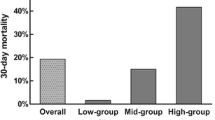
A total of 316 patients were included, and 81.3% (257/316) experienced unfavorable outcomes. Peak NLR was identified as an independent predictor for unfavorable outcomes after sTBI in multivariable logistic regression analysis (odds ratio, 1.086; 95% confidence interval, 1.037–1.137; P < 0.001). Its predictive value was confirmed by receiver operating characteristic analysis (area under curve = 0.775; P < 0.001). The day 1 NLR as well as admission Glasgow Coma Scale score was independently correlated with increased peak NLR.
Conclusion
Peak NLR was associated with the clinical prognosis after sTBI and was a promising predictor for 1-year outcomes.


Similar content being viewed by others
References
Carney NA, Ghajar J. Guidelines for the management of severe traumatic brain injury. Introduction. J Neurotrauma. 2007;24(Suppl 1(5)):1–106.
Cheng P, Yin P, Ning P, et al. Trends in traumatic brain injury mortality in China, 2006–2013: a population-based longitudinal study. PLoS Med. 2017;14(7):e1002332.
Søreide K, Krüger AJ, Vårdal AL, et al. Epidemiology and contemporary patterns of trauma deaths: changing place, similar pace, older face. World J Surg. 2007;31(11):2092–103.
Myburgh JA, Cooper DJ, Finfer SR, et al. Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. J Trauma Inj Infect Crit Care. 2008;64(4):854–62.
Murray GD, Teasdale GM, Braakman R, et al. The European brain injury consortium survey of head injuries. Acta Neurochir. 1999;141(3):223–36.
Barlow KM. Traumatic brain injury. Handb Clin Neurol. 2013;112:891–904.
Saatman KE, Duhaime AC, Bullock R, et al. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25(7):719–38.
Smajic J, Tupkovic LR, Husic S, et al. Systemic inflammatory response syndrome in surgical patients. Med Arch. 2018;72(2):116–9.
Tschoeke SK, Hellmuth M, Hostmann A, Ertel W, Oberholzer A. The early second hit in trauma management augments the proinflammatory immune response to multiple injuries. J Trauma Acute Care Surg. 2007;62(6):1403–4.
Lumsdaine W, Easton RM, Lott NJ, et al. Neutrophil oxidative burst capacity for peri-operative immune monitoring in trauma patients. Inj Int J Care Inj. 2014;45(8):1144–8.
Faist E, Kupper TS, Baker CC, et al. Depression of cellular immunity after major injury. Its association with posttraumatic complications and its reversal with immunomodulation. Arch Surg. 1986;121(9):1000–5.
Albertsmeier M, Quaiser D, Von DV, et al. Major surgical trauma differentially affects T-cells and APC. Innate Immun. 2015;21(1):55–64.
Zahorec R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratislavské Lekárske Listy. 2001;102(1):5–14.
Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M. Neutrophil-to-lymphocyte ratio and neurological deterioration following acute cerebral hemorrhage. Oncotarget. 2017;8(34):57489.
Giede-Jeppe A, Bobinger T, Gerner ST, et al. Neutrophil-to-lymphocyte ratio is an independent predictor for in-hospital mortality in spontaneous intracerebral hemorrhage. Cerebrovasc Dis. 2017;44(1–2):26–34.
Celikbilek A, Ismailogullari S, Zararsiz G. Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease. J Clin Lab Anal. 2014;28(1):27–31.
Yu S, Arima H, Bertmar C, et al. Neutrophil to lymphocyte ratio and early clinical outcomes in patients with acute ischemic stroke. J Neurol Sci. 2018;387:115–8.
Bambury RM, Teo MY, Power DG, et al. The association of pre-treatment neutrophil to lymphocyte ratio with overall survival in patients with glioblastoma multiforme. J Neurooncol. 2013;114(1):149–54.
Proctor MJ, McMillan DC, Morrison DS, et al. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer. 2012;107(4):695–9.
Bhat T, Teli S, Rijal J, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther. 2013;11(1):55–9.
Chen W, Yang J, Li B, et al. Neutrophil to lymphocyte ratio as a novel predictor of outcome in patients with severe traumatic brain injury. J Head Trauma Rehabil. 2018;33(1):E53–9.
Dilektasli E, Inaba K, Haltmeier T, et al. The prognostic value of neutrophil-to-lymphocyte ratio on mortality in critically ill trauma patients. J Trauma Acute Care Surg. 2016;81(5):882–8.
Brain Trauma Foundation. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(1):S59–64.
Galgano M, Toshkezi G, Qiu X, et al. Traumatic brain injury: current treatment strategies and future endeavors. Cell Transpl. 2017;26(7):1118–30.
Feinberg M, Mai JC, Ecklund J. Neurosurgical management in traumatic brain injury. Semin Neurol. 2015;35(1):50–6.
Hilden J, Glasziou P. Regret graphs, diagnostic uncertainty and Youden’s index. Stat Med. 2015;15(10):969–86.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–5.
Marshall L. The outcome of severe closed head injury. J Neurosurg. 1991;75(5):S28–36.
Hanley JA, Mcneil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29.
Saika A, Bansal S, Philip M, Devi BI, Shukla DP. Prognostic value of FOUR and GCS scores in determining mortality in patients with traumatic brain injury. Acta Neurochir. 2015;157(8):1323.
Poon WS, Zhu XL, Ng SC, Wong GK. Predicting one year clinical outcome in traumatic brain injury (TBI) at the beginning of rehabilitation. Acta Neurochir Suppl. 2005;93(93):207–8.
Xue M, Bigio MRD. Comparison of brain cell death and inflammatory reaction in three models of intracerebral hemorrhage in adult rats. J Stroke Cerebrovasc Dis. 2003;12(3):152–9.
Gong C, Hoff JT, Keep RF. Acute inflammatory reaction following experimental intracerebral hemorrhage in rat. Brain Res. 2000;871(1):57–65.
Rhind SG, Crnko NT, Baker AJ, et al. Prehospital resuscitation with hypertonic saline-dextran modulates inflammatory, coagulation and endothelial activation marker profiles in severe traumatic brain injured patients. J Neuroinflamm. 2010;7(1):5.
Roth TL, Nayak D, Atanasijevic T, et al. Transcranial amelioration of inflammation and cell death after brain injury. Nature. 2014;505(7482):223.
Carlos TM, Clark RSB, Franicola-Higgins D, Schiding JK, Kochanek PM. Expression of endothelial adhesion molecules and recruitment of neutrophils after traumatic brain injury in rats. J Leukoc Biol. 1997;61(3):279–85.
Liao Y, Liu P, Guo F, Zhang Z, Zhang Z. Oxidative burst of circulating neutrophils following traumatic brain injury in human. PLoS ONE. 2013;8(7):e68963.
Schwartz M, Moalem G. Beneficial immune activity after CNS injury: prospects for vaccination. J Neuroimmunol. 2001;113(2):185–92.
Palm N. R Not so fast: adaptive suppression of innate immunity. Nat Med. 2007;13(10):1142.
Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci. 2005;6(10):775–86.
Acknowledgements
We’d like to express our sincere gratitude to Chengguang Huang, Minkun Yu, Kehua Sun, and Rulin Bai in Changzheng Hospital for their work in providing the clinical data.
Funding
This study was funded by the National Nature Science Foundation of China (Grant No. 81671206).
Author information
Authors and Affiliations
Contributions
JC and XQ conducted the study design, data collection, and data analysis. ZL and DZ prepared the manuscript. LH reviewed and finalized the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Lijun Hou received grants from National Nature Science Foundation of China. The other authors declared they had no conflicts of interest.
Ethical Approval
All procedures performed in the studies were in accordance with the ethical standards of the Changzheng Hospital and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Chen, J., Qu, X., Li, Z. et al. Peak Neutrophil-to-Lymphocyte Ratio Correlates with Clinical Outcomes in Patients with Severe Traumatic Brain Injury. Neurocrit Care 30, 334–339 (2019). https://doi.org/10.1007/s12028-018-0622-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0622-9