Abstract
Background
Cerebrovascular autoregulation can be continuously monitored from slow fluctuations of arterial blood pressure (ABP) and regional cerebral oxygen saturation (rSO2). The purpose of this study was to evaluate the index of dynamic cerebrovascular autoregulation (TOx) and the associated ‘optimal’ ABP in normal adult healthy subjects.
Methods
Twenty-eight healthy volunteers were studied. TOx was calculated as the moving correlation coefficient between spontaneous fluctuations of ABP and rSO2. ABP was measured with the Finometer photoplethysmograph. The ABP with optimal autoregulation (ABPOPT) was also determined as the ABP level with the lowest associated TOx (opt-TOx).
Results
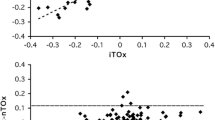
Average rSO2 and TOx was 72.3 ± 2.9% and 0.05 ± 0.18, respectively. Two subjects had impaired autoregulation with a TOx > 0.3. The opt-TOx was − 0.1 ± 0.26. ABPOPT was 87.0 ± 16.7 mmHg. The difference between ABP and ABPOPT was − 0.3 ± 7.5 mmHg. In total, 44% of subjects had a deviation of ABP from ABPOPT exceeding 5 mmHg. ABPOPT ranged from 57 to 117 mmHg.
Conclusions
TOx in healthy volunteers on average displays intact autoregulation and ABP close to ABPOPT. However, some subjects have possible autoregulatory dysfunction or a significant deviation of ABP from ABPOPT, which may confer a susceptibility to neurological injury.



Similar content being viewed by others
References
Czosnyka M, Smieleweski P, Kirkpatrick P, Menon DK, Pickard JD. Monitoring of cerebral autoregulation in head-injured patients. Stroke. 1996;27:1829–34.
Jaeger M, Soehle M, Schuhmann MU, Meixensberger J. Clinical significance of impaired cerebrovascular autoregulation after severe aneurysmal subarachnoid hemorrhage. Stroke. 2012;43:2097–101.
Bindra J, Pham P, Chuan A, Jaeger M, Aneman A. Is impaired cerebrovascular autoregulation associated with outcome in patients admitted to the ICU with early septic shock? Crit Care Resusc. 2016;18:95–101.
Pham P, Bindra J, Chuan A, Jaeger M, Aneman A. Are changes in cerebrovascular autoregulation following cardiac arrest associated with neurological outcome? Results of a pilot study. Resuscitation. 2015;96:192–8.
Ono M, Joshi B, Brady K, et al. Risks for impaired cerebral autoregulation during cardiopulmonary bypass and postoperative stroke. Br J Anaesth. 2012;109:391–8.
Chuan A, Short TG, Peng AZY, et al. Is cerebrovascular autoregulation associated with outcomes after major non-cardiac surgery? A prospective observational pilot study. Acta Anaesthesiol Scand. 2018. https://doi.org/10.1111/aas.13223.
Steiner LA, Pfister D, Strebel SP, Radolovich D, Smielewski P, Czosnyka M. Near-infrared spectroscopy can monitor dynamic cerebral autoregulation in adults. Neurocrit Care. 2008;10:122–8.
Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30:733–8.
Aries MJH, Czosnyka M, Budohoski KP, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40:2456–63.
Ono M, Brady KM, Easley RB, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147:483–9.
Bindra J, Pham P, Aneman A, Chuan A, Jaeger M. Non-invasive monitoring of dynamic cerebrovascular autoregulation using near infrared spectroscopy and the finometer photoplethysmograph. Neurocrit Care. 2016;24:442–7.
Lazaridis C, Smielewski P, Steiner LA, et al. Optimal cerebral perfusion pressure: Are we ready for it? Neurol Res. 2013;35:138–48.
Brady K, Joshi B, Zweifel C, et al. Real-time continuous monitoring of cerebral blood flow autoregulation using near-infrared spectroscopy in patients undergoing cardiopulmonary bypass. Stroke. 2010;41:1951–6.
Diedler J, Santos E, Poli S, Sykora M. Optimal cerebral perfusion pressure in patients with intracerebral hemorrhage: an observational case series. Crit Care. 2014;18:R51.
Jaeger M, Dengl M, Meixensberger J, Schuhmann MU. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Crit Care Med. 2010;38:1343–7.
Rasulo F, Girardini A, Lavinio A, et al. Are optimal cerebral perfusion pressure and cerebrovascular autoregulation related to long-term outcome in patients with aneurysmal subarachnoid hemorrhage? J Neurosurg Anesthesiol. 2012;24:3–8.
Jaeger M, Schuhmann MU, Soehle M, Meixensberger J. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med. 2006;34:1783–8.
Brady KM, Lee JK, Kibler KK, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38:2818–25.
Brady KM, Lee JK, Kibler KK, Easley RB, Koehler RC, Shaffner DH. Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke. 2008;39:2531–7.
Funding
This study was supported by an infrastructure grant from the University of New South Wales.
Author information
Authors and Affiliations
Contributions
PP, JB, and AA performed the experiments and data collection. AA, AC, JMW, and MJ planned and designed the study and obtained funding. PP, JB, AA, and MJ analysed the data. PP, JB, AA, AC, JMW, and MJ interpreted the results, drafted and finalized the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical Approval
The Human Research Ethics Committee of South Western Sydney Local Health District approved this study (HREC/14/LPOOL/135). Written informed consent was obtained from each participating subject.
Rights and permissions
About this article
Cite this article
Pham, P., Bindra, J., Aneman, A. et al. Noninvasive Monitoring of Dynamic Cerebrovascular Autoregulation and ‘Optimal Blood Pressure’ in Normal Adult Subjects. Neurocrit Care 30, 201–206 (2019). https://doi.org/10.1007/s12028-018-0600-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0600-2