Abstract
Background
Status epilepticus (SE) has been identified as a predictor of morbidity and mortality in many acute brain injury patient populations. We aimed to assess the prevalence and impact of SE after intracerebral hemorrhage (ICH) in a large patient sample to overcome limitations in previous small patient sample studies.
Methods
We queried the Nationwide Inpatient Sample for patients admitted for ICH from 1999 to 2011, excluding patients with other acute brain injuries. Patients were stratified into SE diagnosis and no SE diagnosis cohorts. We identified independent risk factors for SE and assessed the impact of SE on morbidity and mortality with multivariable logistic regression models. Logistic regression was used to evaluate the trend in SE diagnoses over time as well.
Results
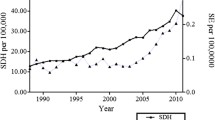
SE was associated with significantly increased odds of both mortality and morbidity (odds ratios (OR) 1.18 [confidence intervals (CI) 1.01–1.39], and OR 1.53 [CI 1.22–1.91], respectively). Risk factors for SE included female sex (OR 1.17 [CI 1.01–1.35]), categorical van Walraven score (vWr 5–14: OR 1.68 [CI 1.41–2.01]; vWr > 14: OR 3.77 [CI 2.98–4.76]), sepsis (OR 2.06 [CI 1.58–2.68]), and encephalopathy (OR 3.14 [CI 2.49–3.96]). Age was found to be associated with reduced odds of SE (OR 0.97 [CI 0.97–0.97]). From 1999 to 2011, prevalence of SE diagnosis increased from 0.25 to 0.61% (p < 0.001). Factors associated with SE were female sex, medium and high risk vWr score, sepsis, and encephalopathy. Independent predictors associated with increased mortality from SE were increased age, pneumonia, myocardial infarction, cardiac arrest, and sepsis.
Conclusions
SE is a significant, likely underdiagnosed, predictor of morbidity and mortality after ICH. Future studies are necessary to better identify which patients are at highest risk of SE to guide resource utilization.

Similar content being viewed by others
References
Elixhauser Comorbidity Software, Version 3.7. In: Healthcare cost and utilization project: agency for healthcare research and quality.
Elixhauser Composite Scores. In: Cleveland Clinic.
Bateman BT, Claassen J, Willey JZ, Hirsch LJ, Mayer SA, Sacco RL, et al. Convulsive status epilepticus after ischemic stroke and intracerebral hemorrhage: frequency, predictors, and impact on outcome in a large administrative dataset. Neurocrit Care. 2007;7:187–93.
Bladin CF, Alexandrov AV, Bellavance A, Bornstein N, Chambers B, Cote R, et al. Seizures after stroke: a prospective multicenter study. Arch Neurol. 2000;57:1617–22.
Bleck TP. Status epilepticus and the use of continuous EEG monitoring in the intensive care unit. Continuum (Minneap Minn). 2012;18:560–78.
Bruning T, Awwad S, Al-Khaled M. Do early seizures indicate survival of patients with nontraumatic intracerebral hemorrhage? Cerebrovasc Dis. 2016;41:68–73.
Claassen J, Jette N, Chum F, Green R, Schmidt M, Choi H, et al. Electrographic seizures and periodic discharges after intracerebral hemorrhage. Neurology. 2007;69:1356–65.
De Herdt V, Dumont F, Henon H, Derambure P, Vonck K, Leys D, et al. Early seizures in intracerebral hemorrhage: incidence, associated factors, and outcome. Neurology. 2011;77:1794–800.
Dhakar MB, Sivakumar S, Bhattacharya P, Shah A, Basha MM. A retrospective cross-sectional study of the prevalence of generalized convulsive status epilepticus in traumatic brain injury: United States 2002–2010. Seizure. 2015;32:16–22.
Dolera-Moreno C, Palazon-Bru A, Colomina-Climent F, Gil-Guillen VF. Construction and internal validation of a new mortality risk score for patients admitted to the intensive care unit. Int J Clin Pract. 2016;70:916–22.
Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. Med Klin Intensivmed Notfmed. 2016;111:417–24.
Forsgren L, Bucht G, Eriksson S, Bergmark L. Incidence and clinical characterization of unprovoked seizures in adults: a prospective population-based study. Epilepsia. 1996;37:224–9.
Gilmore EJ, Gaspard N, Choi HA, Cohen E, Burkart KM, Chong DH, et al. Acute brain failure in severe sepsis: a prospective study in the medical intensive care unit utilizing continuous EEG monitoring. Intensive Care Med. 2015;41:686–94.
Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935–1984. Epilepsia. 1993;34:453–68.
Hoyert DL: 75 Years of Mortality in the United States, 1935–2010, in Services USDoHaH (ed), 2012.
Jette NA, Hirsch LA. Continous electroencephalogram monitoring in critically Ill patients. Curr Neurol Neurosci Rep. 2005;5:312–21.
Kennedy JD, Gerard EE. Continuous EEG monitoring in the intensive care unit. Curr Neurol Neurosci Rep. 2012;12:419–28.
Laccheo I, Sonmezturk H, Bhatt AB, Tomycz L, Shi Y, Ringel M, et al. Non-convulsive status epilepticus and non-convulsive seizures in neurological ICU patients. Neurocrit Care. 2015;22:202–11.
Lin CL, Dumont AS, Lieu AS, Yen CP, Hwang SL, Kwan AL, et al. Characterization of perioperative seizures and epilepsy following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2003;99:978–85.
Madzar D, Kuramatsu JB, Gollwitzer S, Lucking H, Kloska SP, Hamer HM, et al. Seizures among long-term survivors of conservatively treated ICH patients: incidence, risk factors, and impact on functional outcome. Neurocrit Care. 2014;21:211–9.
McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS ONE. 2015;10:e0135834.
Naeije G, Depondt C, Meeus C, Korpak K, Pepersack T, Legros B. EEG patterns compatible with nonconvulsive status epilepticus are common in elderly patients with delirium: a prospective study with continuous EEG monitoring. Epilepsy Behav. 2014;36:18–21.
Nagayama M. Nonconvulsive status epilepticus: clinical practice and pathophysiology. Brain Nerve. 2013;65:561–72.
Naidech AM, Garg RK, Liebling S, Levasseur K, Macken MP, Schuele SU, et al. Anticonvulsant use and outcomes after intracerebral hemorrhage. Stroke. 2009;40:3810–5.
Ney JP, van der Goes DN, Nuwer MR, Nelson L, Eccher MA. Continuous and routine EEG in intensive care: utilization and outcomes, United States 2005–2009. Neurology. 2013;81:2002–8.
Passero S, Rocchi R, Rossi S, Ulivelli M, Vatti G. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 2002;43:1175–80.
Sethi NK, Rapaport BS, Solomon GE. An audit of continuous EEG monitoring in the neurological-neurosurgical intensive care unit. J Clin Neurophysiol. 2014;31:416–7.
Sheth KN, Martini SR, Moomaw CJ, Koch S, Elkind MS, Sung G, et al. Prophylactic antiepileptic drug use and outcome in the ethnic/racial variations of intracerebral hemorrhage study. Stroke. 2015;46:3532–5.
Sutter R. Are We prepared to detect subtle and nonconvulsive status epilepticus in critically Ill patients? J Clin Neurophysiol. 2016;33:25–31.
Thompson NR, Fan Y, Dalton JE, Jehi L, Rosenbaum BP, Vadera S, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015;53:374–9.
Urtecho J, Snapp M, Sperling M, Maltenfort M, Vibbert M, Athar MK, et al. Hospital mortality in primary admissions of septic patients with status epilepticus in the United States*. Crit Care Med. 2013;41:1853–62.
van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–7.
Yang TM, Lin WC, Chang WN, Ho JT, Wang HC, Tsai NW, et al. Predictors and outcome of seizures after spontaneous intracerebral hemorrhage. Clinical article. J Neurosurg. 2009;111:87–93.
Young GB, Jordan KG, Doig GS. An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality. Neurology. 1996;47:83–9.
Zandieh A, Messe SR, Cucchiara B, Mullen MT, Kasner SE, Collaborators V-I. Prophylactic use of antiepileptic drugs in patients with spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:2159–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning.
Rights and permissions
About this article
Cite this article
Mehta, A., Zusman, B.E., Shutter, L.A. et al. The Prevalence and Impact of Status Epilepticus Secondary to Intracerebral Hemorrhage: Results from the US Nationwide Inpatient Sample. Neurocrit Care 28, 353–361 (2018). https://doi.org/10.1007/s12028-017-0489-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0489-1